Abstract
Cerebrospinal fluid (CSF) leakage is a well-known complication of craniotomies and there are several dural closure techniques. One commonly used commercial product as adjunct for dural closure is the collagen-bound fibrin sealant TachoSil®. We analysed whether the addition of TachoSil has beneficial effects on postoperative complications and outcomes. Our prospective, institutional database was retrospectively queried, and 662 patients undergoing craniotomy were included. Three hundred fifty-two were treated with dural suture alone, and in 310, TachoSil was added after primary suture. Our primary endpoint was the rate of postoperative complications associated with CSF leakage. Secondary endpoints included functional, disability and neurological outcome. Systematic review according to PRISMA guidelines was performed to identify studies comparing primary dural closure with and without additional sealants. Postoperative complications associated with CSF leakage occurred in 24 (7.74%) and 28 (7.95%) procedures with or without TachoSil, respectively (p = 0.960). Multivariate analysis confirmed no significant differences in complication rate between the two groups (aOR 0.97, 95% CI 0.53–1.80, p = 0.930). There were no significant disparities in postoperative functional, disability or neurological scores. The systematic review identified 661 and included 8 studies in the qualitative synthesis. None showed a significant superiority of additional sealants over standard technique regarding complications, rates of revision surgery or outcome. According to our findings, we summarize that routinary use of TachoSil and similar products as adjuncts to primary dural sutures after intracranial surgical procedures is safe but without clear advantage in complication avoidance or outcome. Future studies should investigate whether their use is beneficial in high-risk settings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cerebrospinal fluid (CSF) leakage is an imminent risk of cranial neurosurgery, whenever the dura mater is opened. Possible complications secondary to CSF leakage include persistent CSF fistula, pseudo-meningocele or secondary infection (meningitis/cerebritis), leading to increased morbidity and mortality, prolongation of hospital stay and higher cost of care [1,2,3]. According to the literature, the incidence of CSF leakage varies between 1 and 30%, depending on the location of surgery (e.g. higher likelihood is commonly reported after posterior fossa surgery), pathology- and patient-related factors and the technique used for dural closure [4,5,6,7]. Standard methods of dural closure include use of running or interrupted sutures, which may be supplemented with additional sealants, glues or dural substitutes in order to achieve a water-tight closure [8].
One of the most commonly used commercial products as adjunct in dural closure for neurosurgical interventions is the collagen-bound fibrin sealant called TachoSil® (Takeda Pharmaceutical Company, Tokyo, Japan) [9]. TachoSil is a ready-to-use membrane-like adhesive product, which contains exclusively human coagulation factors [10, 11]. While there is an ongoing development of new sealing materials, there still is no consensus on a standardization of dural closure. Only few clinical studies evaluated outcomes of different closure techniques in a randomized and controlled manner [8, 12]. More comparative data on complication rates and outcomes for different dural closure techniques is needed.
Hence, the aim of this study was to investigate postoperative complication rates and outcomes in patients undergoing craniotomy with or without TachoSil as adjunct to dural sutures. In addition, the results of our own institutional data are complemented by a systematic review of the literature, identifying studies that compared different surgical techniques for dural closure.
Material and methods
This paper is composed of two parts. In a first step, we conducted a retrospective analysis of a single-centre prospective database, containing demographic, disease- and treatment-specific complication and outcome data of all neurosurgical interventions conducted at the University Hospital of Zurich, Switzerland [13]. In a second step, we conducted a systematic review of the literature identifying and analysing any studies comparing postoperative CSF leakages in patients undergoing craniotomy and appertaining dural closure with or without the use of additional sealing material.
The protocol of this study was designed and carried out according to International Conference of Harmonisation – Good Clinical Practice standards [14]. The data collection was approved by the local Ethics Committee (KEK-ZH 2012–0244) and included patients that signed an informed consent sheet to allow research with their de-identified personal data. The data collection was registered at http://www.clinicaltrials.gov (identifier: NCT01628406) and follows the STROBE recommendation for observational studies.
Part I — Institutional data collection and analysis
Data sources
Our institutional database [15] includes prospectively collected information on patient age and sex, operation date, indication for and type of surgery, lesion location, re-operation, surgeons, operation time and occurrence of a complication [16,17,18]. Furthermore, standardized scores used to estimate general well-being and function in daily life (Karnofsky Performance Score (KPS)), disability (modified Rankin Scale (mRS)) and neurological status (National Institutes of Health Stroke Scale (NIHSS)) at time points of hospital admission, discharge and 3 to 6 months after surgery are documented in the database [19,20,21]. The information whether TachoSil was used for closure during any neurosurgical procedure was extracted manually from the billing form for all patients. The extracted data were entered into an ad hoc database for analysis.
Inclusion/exclusion criteria
All patients undergoing craniotomy in a timespan of 22 months between January 2018 and October 2019 with opening and closing of the dura mater during the same procedure were included. Interventions involving extensive dural opening without closure, e.g. as for decompressive craniectomies, were not considered. Also, paediatric neurosurgical interventions (e.g. posterior fossa decompression for Chiari malformations) were excluded for their distinct risk profile. Whereas re-operations due to postoperative complications (e.g. wound healing issues, infections, rebleeding) were excluded as index procedures, previous surgery at the same site for, e.g., tumour relapse in neurooncological or aneurysm regrowth in vascular patients, were not considered exclusion criteria as previous literature indicates a similar risk profile [18].
Surgical procedure and TachoSil application
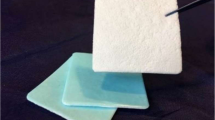
All surgeries involved a dural incision and subsequent dural closure during the same procedure. In each case, the dura was closed primarily with sutures (Prolene®, PDS® or Vicryl®, Ethicon Inc., Somerville, NJ, USA). The additional administration of TachoSil was optional and decided by the responsible surgeon according to personal preference. TachoSil is a collagen sponge coated with the human coagulation factors fibrinogen and thrombin. It is a ready-to-use product with simple application onto the surgical site, as it firmly glues to the tissue surface upon contact with blood, other body fluids or saline [11]. The sponge is absorbed by the body within several weeks. In our hospital, TachoSil is applied to the external side of the dura mater, on the suture line, slightly exceeding it with a small overlap with the surrounding pachymeninx on all sides. To achieve optimal and uniform contact, the applied TachoSil is gently pressed onto the dura with moistened surgical gauze.
Outcomes and statistical analysis
Relevant demographic data as well as baseline and surgery characteristics were extracted from the database and summarized in a synoptic table. Data are presented as frequencies and percentages for categorical variables and as mean ± standard deviation (SD) or median ± interquartile range (IQR) for continuous variables. Statistical significance was analysed using students’ t test for quantitative, the Wilcoxon rank sum test for ordinal and the Pearson chi-squared test for categorical variables, respectively.
As primary end point, the frequency of postoperative complications associated with CSF leakage was compared between the study group (dural closure with TachoSil) and the control group (dural closure without TachoSil). Postoperative complications until 6 months after the index procedure were considered and classified as CSF leakage, CSF fistula, any kind of CSF infection (meningitis and/or cerebritis), wound infection or wound dehiscence. Results are shown as frequencies and percentages for the individual complications, as well as for total complications. For complications, statistical significance was assessed using a chi-squared test. Furthermore, a multivariable logistic regression model was created to adjust for baseline group differences. To include potential confounders in our regression model, variable selection was performed according to the “purposeful variable selection” algorithm described by Bursac et al. [22] Results were analysed for changes after adjustment, and results are expressed as (adjusted) odds ratios (aORs) with 95% confidence interval.
The following secondary end points were considered: KPS, mRS and NIHSS at the time point of hospital admission, discharge and 3 to 6 months postoperative. Statistical significance was calculated using Wilcoxon rank-sum test, and results are presented as p-value.
Statistical analyses were performed using R (version 3.6.2, R Foundation for Statistical Computing, Vienna, Austria). The p-value was assumed to be statistically significant when ≤ 0.05.
Part II — Systematic review of the literature
A systematic review of the literature was carried out to identify studies comparing postoperative CSF leakage in patients who underwent cranial neurosurgery involving dural opening and closure with or without the use of a sealing additive. The individual steps of title and abstract screening, full-text review and data extraction were performed independently by two reviewers (ME and LL), and disagreements at any stage were resolved by discussion and consensus. In case of persisting discordance, resolution was achieved through discussion with a third, neutral reviewer. For this part of the study, the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) protocol was applied [23].
Search strategy
For the identification of eligible articles, the PubMed/MEDLINE (OVID), Embase (OVID) and Cochrane Library and Scopus (Elsevier) database were searched. The search strategy included combinations of the terms “cerebrospinal fluid leakage, dural defects, postoperative CSF leakage, dural sealant, dural closure, TachoSil, surgical revision, craniotomy, cranial and neurosurgery”, while excluding the terms “transsphenoidal, pituitary and spinal” as those procedures are not of interest for the current research question (Supplemental Table 1). To optimize data mining, word variations and exploded medical subject headings were included whenever feasible. Additionally, reference lists of identified articles were hand-searched to include further studies of interest. The last comprehensive search was conducted on 11 April 2020.
Study selection
Only in vivo studies including human subjects and written in English, Italian, Spanish, French, Dutch or German were considered. For a study to be included, patients had to undergo craniotomy with opening and primary closure of the dura mater. Included studies had to compare at least two dural closure techniques, one of which had to include the addition of a sealing additive. Finally, they had to report at least either (a) the proportion of patients with postoperative CSF leakage or (b) other relevant postoperative complications secondary to CSF leakage or (c) the proportion of patients requiring revision surgery because of inadequate dural closure. Detailed in- and exclusion criteria are listed in Supplemental Table 2.
Data extraction and assessment of evidence level
The following information was extracted from included publications, whenever available: authors, year of publication, study design, study arms, population, number of patients, outcome measures, results with focus on the primary endpoint and author conclusion. The evidence level of the included studies was determined based on data from the Oxford Centre for Evidence-based Medicine (Supplemental Table 3) [24].
Results
Part I — Retrospective single-centre comparative cohort study
A total of 1915 patients were identified, of which 1253 patients undergoing either craniectomy, burr-hole trepanation or endoscopic cranial procedures were excluded or were lost to follow-up within 6 months after surgery and hence omitted from analysis. A total of 662 patients were included: for 352 of them, dural suture alone was performed (control group) and in 310, TachoSil was added in addition to the primary suture (study group). Patient- and disease-specific information, as well as surgery characteristics of the included patients, is summarized in Table 1.
Analysis of the primary endpoint
Postoperative complications occurred in 7.74% (n = 24) of procedures, in which TachoSil was added and in 7.95% (n = 28) of procedures with sutures alone (p = 0.960; Table 2). Significant differences in disease- and surgery-specific baseline characteristics were also found (Table 1). TachoSil application was more commonly reported in neuro-oncological procedures when compared to neurovascular procedures (p < 0.01) and in high-grade glioma and metastasis when compared to other neuro-oncological procedures (p = 0.017). Furthermore, TachoSil was also more commonly used in reoperations than in first surgeries, with borderline significance (p = 0.056). Therefore, a multivariable logistic regression model was built. In the adjusted model, patients in the study group were 97% as likely as patients in the control group to experience a postoperative complication associated with CSF leakage (aOR 0.97, 95% CI 0.53–1.80, p = 0.930; Table 3).
Analysis of secondary endpoints
In both groups, average scores of function, disability and neurological status showed a slight decline between baseline and 6-month postoperative. There were no significant differences in the change in KPS (− 5.48 vs. − 6.59, p = 0.667), mRS (+ 0.37 vs. + 0.01, p = 0.182) and NIHSS (+ 0.32 vs. + 0.34, p = 0.741) between the study and control group, respectively.
Part II — Systematic review of the literature
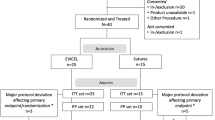
A flow-diagram for the systematic literature search is provided in Fig. 1. The database search — after removal of duplicates — yielded 352 eligible articles. During title and abstract screening, 309 articles were excluded for not meeting in- or for meeting exclusion criteria. Of the remaining 43 articles, further 35 records were excluded during full-text screening, resulting in eight articles that were used for qualitative synthesis. Excluded papers during full-text screening did not meet the in- or met exclusion criteria, as described in the “Material and methods” section and in Supplemental Table 2. Among those, 14 papers were excluded because of the study design, 6 did not adequately compare the analysed closing techniques, 3 because of anatomical reasons (transsphenoidal or pituitary surgeries) and 12 for other reasons (incomplete studies, duplicates). A comprehensive overview of the included articles is provided in Table 4. Five studies were randomized controlled trials; the remaining were pro- and retrospective cohort studies with control groups. A total of 2045 participants were analysed, of which 1086 were treated with the addition of adjunctive sealant or technique during dural closure (study group), and 959 were treated with standard of care (control groups).
As a crucial endpoint, the occurrence of postoperative CSF leak after dural closure was compared. All eight studies showed less postoperative CSF leaks in the study group. However, the differences of CSF leak incidence between study and control groups were reported to be statistically insignificant in six of these studies (Table 4) [12, 25,26,27,28,29].
Discussion
Dural closure remains a critical step in any neurosurgical procedure that involves opening meningeal layers of the central nervous system. Insufficient closure may lead to postoperative CSF leakage, which can result in unanticipated morbidity and prolonged length of hospitalization, thereby resulting in increased healthcare costs [2, 32]. During recent decades, a variety of new sealing materials and surgical techniques have been developed and used in clinical practice. However, robust evidence about their efficacy is scarce due to the paucity of relevant studies. There still is no official consensus on a standardization of dural closure technique in the neurosurgical community [33].
In this retrospective institutional single-centre study, we observed a similar rate of CSF-related complications, with a rate of about 8% in both the experimental and control group (Table 2). To minimize the risk of bias from baseline group differences, multivariable logistic regression models were built without changing the main finding of this study (Table 3). To further investigate the potential clinical relevance of CSF leakage — its potential effect on patient outcome — the pre- to postoperative change of standardized scores of function, disability and neurological status was compared. Again, there was no significant difference in outcome between the study and control group.
It is important to note that for the included cases and procedures, surgeons were allowed to choose for each case whether or not to use TachoSil as an additive to dural suture. In our department, there are surgeons across all experience levels with preferences regarding the use of TachoSil or not, which results in a relatively even distribution of cases with low, moderate or high complexity into the study and control group. Still, we cannot fully exclude a systematic bias resulting from operative experience, as junior neurosurgeons with less developed dexterity and potentially less optimal dural readaptation might be tempted to add TachoSil more frequently than experienced senior neurosurgeons. Hence, the self-contained choice of the dural closure technique by each individual surgeon may be a confounder, where the occurrence of postoperative CSF leakage could result more from surgical experience than from the dural closure technique. It was also for this inevitable limitation of our institutional data that we considered a validation of our findings against the currently available relevant literature mandatory.
The findings of the systematic review (Table 4) mirrored our own institutional data, as none of the included studies found a significant difference in the occurrence of clinically relevant complications resulting from CSF leakage between study and control groups. In a study, significantly less postoperative CSF collection was found in the study group compared to the control group [31]. However, CSF collection was often self-limiting and had no influence on the rate of postoperative complications during follow up. Altogether, the investigated new adjuncts and techniques for dural closure were reported as safe and easy-to-use options for the prevention of CSF leakage after dural closure. In conclusion, none of the studies could show a statistically significant superiority over standard of care dural closure techniques regarding overall postoperative complications due to CSF leakage and rate of patients requiring additional revision surgery. Some authors still concluded that the experimental sealing technique might show advantages for dural closure in certain high-risk settings, e.g. after posterior fossa surgery [29] or in patients with critical comorbidities, such as diabetes [27]. While the use of even more water-tight dural closure techniques may be beneficial under these circumstances, no evidence is currently available to support the standardized use of additional dural sealant in daily clinical routine if the dura is meticulously closed using microsurgical techniques.
We decided to not perform a quantitative synthesis (meta-analysis) from the systematic review, as the available studies showed extreme and unavoidable heterogeneity to in- and exclusion criteria, experimental and control techniques and choice or definition of complications and outcomes. Based on the experience made throughout the systematic review, a critical step towards finding the optimal dural sealing technique in the future may require a better standardization of studies in order to allow comparison of different surgical techniques. We anticipate the use of clinically relevant outcomes only, such as postoperative CSF fistula, wound dehiscence and infection and to exclude often self-limiting and purely imaging-based outcome measures (e.g. subcutaneous CSF collection) without clinical relevance. Furthermore, future studies should ideally record quality outcomes such as length of hospital stay, days spent on the intensive care or intermediate care units, as well as the necessity of revision surgery until 90 days postoperative, besides cost-effectiveness [27].
Strengths and limitations
This paper contains prospectively collected data with high granularity from a tertiary European neurosurgical department, allowing for robust estimate of the effect size of the experimental technique on complications and clinical outcomes due to the reasonably large sample size. We consider the inclusion of a high number of different surgeons and procedures as a distinct strength, as the findings are more likely to be representative of the real-life clinical scenario and can more easily be transferred to other centres and settings. Moreover, a systematic literature review validates our results against the available literature, building up additional credibility to the reported findings.
Unavoidable limitations are inherent to the retrospective nature of the study. Also, it is likely that there are other parameters that can influence the primary outcome, which, although conceivable, have neither been studied in our own nor in the papers included in the systematic review. Those factors could include significant comorbidities, immune system strength and general capacity for wound healing [27], or elevated preoperative C-reactive protein levels [6, 27]. The limitation regarding the level of experience and selection of additional dural sealant as potential confounder has been discussed above.
Conclusions and implications of our study
According to own institutional data and in agreement with a systematic review of the current literature, the general use of TachoSil and similar products as adjuncts to primary dural sutures does not seem to reduce CSF-related postoperative complications or improve clinical outcomes. Whether or not additional dural sealant may be beneficial in certain high-risk settings (e.g. posterior fossa surgery, revision surgery) remains unclear and should be the focus of future studies that should ideally include cost-effectiveness analyses.
References
Cosgrove GR, Delashaw JB, Grotenhuis JA, Tew JM, Van Loveren H, Spetzler RF, Payner T, Rosseau G, Shaffrey ME, Hopkins LN, Byrne R, Norbash A (2007) Safety and efficacy of a novel polyethylene glycol hydrogel sealant for watertight dural repair. J Neurosurg 106:52–58. https://doi.org/10.3171/jns.2007.106.1.52
Grotenhuis JA (2005) Costs of postoperative cerebrospinal fluid leakage: 1-year, retrospective analysis of 412 consecutive nontrauma cases. Surg Neurol 64:490–493. https://doi.org/10.1016/j.surneu.2005.03.041 (discussion 493–494)
Horowitz G, Fliss DM, Margalit N, Wasserzug O, Gil Z (2011) Association between cerebrospinal fluid leak and meningitis after skull base surgery. Otolaryngol Head Neck Surg 145:689–693. https://doi.org/10.1177/0194599811411534
Becker SS, Jackler RK, Pitts LH (2003) Cerebrospinal fluid leak after acoustic neuroma surgery: a comparison of the translabyrinthine, middle fossa, and retrosigmoid approaches. Otol Neurotol 24:107–112. https://doi.org/10.1097/00129492-200301000-00021
Coucke B, Van Gerven L, De Vleeschouwer S, Van Calenbergh F, van Loon J, Theys T (2022) The incidence of postoperative cerebrospinal fluid leakage after elective cranial surgery: a systematic review. Neurosurg Rev 45:1827–1845. https://doi.org/10.1007/s10143-021-01641-y
Kumar A, Maartens NF, Kaye AH (2003) Evaluation of the use of BioGlue in neurosurgical procedures. J Clin Neurosci 10:661–664. https://doi.org/10.1016/s0967-5868(03)00163-2
Merkus P, Taibah A, Sequino G, Sanna M (2010) Less than 1% cerebrospinal fluid leakage in 1,803 translabyrinthine vestibular schwannoma surgery cases. Otol Neurotol 31:276–283. https://doi.org/10.1097/MAO.0b013e3181cc06ad
Walcott BP, Neal JB, Sheth SA, Kahle KT, Eskandar EN, Coumans J-V, Nahed BV (2014) The incidence of complications in elective cranial neurosurgery associated with dural closure material. J Neurosurg 120:278–284. https://doi.org/10.3171/2013.8.JNS13703
Montano N, Pignotti F, Auricchio AM, Fernandez E, Olivi A, Papacci F (2019) Results of TachoSil® associated with fibrin glue as dural sealant in a series of patients with spinal intradural tumors surgery. Technical note with a review of the literature. J Clin Neurosci 61:88–92. https://doi.org/10.1016/j.jocn.2018.10.138
Kawasaki S, Origasa H, Tetens V, Kobayashi M (2017) Comparison of TachoSil and TachoComb in patients undergoing liver resection-a randomized, double-blind, non-inferiority trial. Langenbecks Arch Surg 402:591–598. https://doi.org/10.1007/s00423-017-1571-z
Rickenbacher A, Breitenstein S, Lesurtel M, Frilling A (2009) Efficacy of TachoSil a fibrin-based haemostat in different fields of surgery–a systematic review. Expert Opin Biol Ther 9:897–907. https://doi.org/10.1517/14712590903029172
George B, Matula C, Kihlström L, Ferrer E, Tetens V (2017) Safety and efficacy of TachoSil (absorbable fibrin sealant patch) compared with current practice for the prevention of cerebrospinal fluid leaks in patients undergoing skull base surgery: a randomized controlled trial. Neurosurgery 80:847–853. https://doi.org/10.1093/neuros/nyx024
Stienen MN, Serra C, Stieglitz LH, Krayenbühl N, Bozinov O, Regli L (2018) UniversitätsSpital Zürich: 80 years of neurosurgical patient care in Switzerland. Acta Neurochir (Wien) 160:3–22. https://doi.org/10.1007/s00701-017-3357-z
Switula D (2000) Principles of good clinical practice (GCP) in clinical research. Sci Eng Ethics 6:71–77. https://doi.org/10.1007/s11948-000-0025-z
Sarnthein J, Stieglitz L, Clavien P-A, Regli L (2016) A patient registry to improve patient safety: recording general neurosurgery complications. PLoS ONE 11:e0163154. https://doi.org/10.1371/journal.pone.0163154
Stienen MN, Zhang DY, Broggi M, Seggewiss D, Villa S, Schiavolin S, Bozinov O, Krayenbühl N, Sarnthein J, Ferroli P, Regli L (2018) The influence of preoperative dependency on mortality, functional recovery and complications after microsurgical resection of intracranial tumors. J Neurooncol 139:441–448. https://doi.org/10.1007/s11060-018-2882-9
Vasella F, Velz J, Neidert MC, Henzi S, Sarnthein J, Krayenbühl N, Bozinov O, Regli L, Stienen MN (2019) Safety of resident training in the microsurgical resection of intracranial tumors: data from a prospective registry of complications and outcome. Sci Rep 9:954. https://doi.org/10.1038/s41598-018-37533-3
Zattra CM, Zhang DY, Broggi M, Velz J, Vasella F, Seggewiss D, Schiavolin S, Bozinov O, Krayenbühl N, Sarnthein J, Ferroli P, Regli L, Stienen MN (2019) Repeated craniotomies for intracranial tumors: is the risk increased? Pooled analysis of two prospective, institutional registries of complications and outcomes. J Neurooncol 142:49–57. https://doi.org/10.1007/s11060-018-03058-y
Broderick JP, Adeoye O, Elm J (2017) Evolution of the modified Rankin scale and its use in future stroke trials. Stroke 48:2007–2012. https://doi.org/10.1161/STROKEAHA.117.017866
Lyden P (2017) Using the National Institutes of Health Stroke Scale: a cautionary tale. Stroke 48:513–519. https://doi.org/10.1161/STROKEAHA.116.015434
Péus D, Newcomb N, Hofer S (2013) Appraisal of the Karnofsky Performance Status and proposal of a simple algorithmic system for its evaluation. BMC Med Inform Decis Mak 13:72. https://doi.org/10.1186/1472-6947-13-72
Bursac Z, Gauss CH, Williams DK, Hosmer DW (2008) Purposeful selection of variables in logistic regression. Source Code Biol Med 3:17. https://doi.org/10.1186/1751-0473-3-17
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700. https://doi.org/10.1136/bmj.b2700
Medicine OCfE-b. Oxford Centre for Evidence-based medicine - levels of evidence (2009). Available at http://www.cebm.net/index.aspx?o=10252009.
Strong MJ, West GA, Woo H, Couture DE, Wilson JA, Munoz LF, Rosen CL, Greenlee JD, van Loveren HR, Iantosca M, Baird CJ, Smith M, McGirt M, Parish J, Asher AL (2017) A pivotal randomized clinical trial evaluating the safety and effectiveness of a novel hydrogel dural sealant as an adjunct to dural repair. Oper Neurosurg (Hagerstown) 13:204–212. https://doi.org/10.1093/ons/opw004
Green AL, Arnaud A, Batiller J, Eljamel S, Gauld J, Jones P, Martin D, Mehdorn M, Ohman J, Weyns F (2015) A multicentre, prospective, randomized, controlled study to evaluate the use of a fibrin sealant as an adjunct to sutured dural repair. Br J Neurosurg 29:11–17. https://doi.org/10.3109/02688697.2014.948808
Hutter G, von Felten S, Sailer MH, Schulz M, Mariani L (2014) Risk factors for postoperative CSF leakage after elective craniotomy and the efficacy of fleece-bound tissue sealing against dural suturing alone: a randomized controlled trial. J Neurosurg 121:735–744. https://doi.org/10.3171/2014.6.JNS131917
Osbun JW, Ellenbogen RG, Chesnut RM, Chin LS, Connolly PJ, Cosgrove GR, Delashaw JB, Golfinos JG, Greenlee JDW, Haines SJ, Jallo J, Muizelaar JP, Nanda A, Shaffrey M, Shah MV, Tew JM, van Loveren HR, Weinand ME, White JA, Wilberger JE (2012) A multicenter, single-blind, prospective randomized trial to evaluate the safety of a polyethylene glycol hydrogel (Duraseal Dural Sealant System) as a dural sealant in cranial surgery. World Neurosurg 78:498–504. https://doi.org/10.1016/j.wneu.2011.12.011
Arlt F, Trantakis C, Krupp W, Renner C, Winkler D, Strauss G, Meixensberger J (2011) Cerebrospinal fluid leak after microsurgical surgery in vestibular schwannomas via retrosigmoidal craniotomy. Neurol Res 33:947–952. https://doi.org/10.1179/1743132811Y.0000000042
Than KD, Baird CJ, Olivi A (2008) Polyethylene glycol hydrogel dural sealant may reduce incisional cerebrospinal fluid leak after posterior fossa surgery. Neurosurgery 63:ONS182-186. https://doi.org/10.1227/01.neu.0000335034.08274.d2 (discussion ONS186–187)
Yoshimoto T, Sawamura Y, Houkin K, Abe H (1997) Effectiveness of fibrin glue for preventing postoperative extradural fluid leakage. Neurol Med Chir (Tokyo) 37:886–889. https://doi.org/10.2176/nmc.37.886 (discussion 889–890)
Boogaarts JD, Grotenhuis JA, Bartels RHMA, Beems T (2005) Use of a novel absorbable hydrogel for augmentation of dural repair: results of a preliminary clinical study. Neurosurgery 57:146–151. https://doi.org/10.1227/01.neu.0000164384.05351.59
Barzo P, Szabo S, Orbay P, Jamieson V (2020) First time in human study: neuroseal dural sealant prevents cerebrospinal fluid leakage following elective cranial surgery. OAJNN 12:112–115. https://doi.org/10.19080/OAJNN.2020.12.555850
Funding
Open access funding provided by University of Zurich
Author information
Authors and Affiliations
Contributions
Conceptualization: Mirka Epskamp, Martin N. Stienen. Methodology: Mirka Epskamp, Martin N. Stienen. Formal analysis and investigation: Alessandro Carretta, Mirka Epskamp, Linus Ledermann, Victor E. Staartjes, Martin N. Stienen. Writing — original draft preparation: Alessandro Carretta, Mirka Epskamp. Writing — review and editing: Victor E. Staartjes, Martin N. Stienen. Supervision: Victor E. Staartjes, Marian C. Neidert, Luca Regli, Martin N. Stienen. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Carretta, A., Epskamp, M., Ledermann, L. et al. Collagen-bound fibrin sealant (TachoSil®) for dural closure in cranial surgery: single-centre comparative cohort study and systematic review of the literature. Neurosurg Rev 45, 3779–3788 (2022). https://doi.org/10.1007/s10143-022-01886-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-022-01886-1