Abstract
Introduction
Several factors that affect functional recovery after surgery in severe brachial plexus lesions have been identified, i.e., time to surgery and presence of root avulsions. The body mass index (BMI) of the patient could be one of these possible factors. The objective of the present paper is to systematically study the relationship between BMI and the outcome of abduction following spinal accessory to suprascapular nerve transfer.
Methods
We retrospectively studied 18 cases that followed these inclusion criteria: (1) Male patients with a spinal accessory to suprascapular nerve transfer as the only procedure for shoulder function reanimation; (2) at least C5-C6 root avulsion; (3) interval between trauma and surgery less than 12 months; (4) follow-up was at least 2 years; (5) no concomitant injury of the shoulder girdle. Pearson correlation analysis and linear regression was performed for BMI versus shoulder abduction.
Results
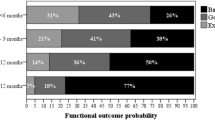
The mean range of post-operative abduction obtained across the entire series was 49.7° (SD ± 30.2). Statistical evaluation revealed a significant, negative moderately strong correlation between BMI and post-operative range of shoulder abduction (r = −0.48, p = 0.04). Upon simple linear regression, time to surgery (p = 0.04) was the only statistically significant predictor of abduction range negatively correlated.
Conclusions
Analysis of this series suggests that a high BMI of patients undergoing brachial plexus surgery is a negative predictor of outcome, albeit less important than others like time from trauma to surgery. Nevertheless, the BMI of patients should be taken into consideration when planning surgical strategies for reconstruction.


Similar content being viewed by others
References
Aparecida Leandro-Merhi V, Luiz Braga de Aquino J, Gonzaga Teixeira de Camargo J (2012) Agreement between body mass index, calf circumference, arm circumference, habitual energy intake and the MNA in hospitalized elderly. J Nutr Health Aging 16:128–132
Bertelli JA, Ghizoni MF (2004) Reconstruction of C5 and C6 brachial plexus avulsion injury by multiple nerve transfers: spinal accessory to suprascapular, ulnar fascicles to biceps branch, and triceps long or lateral head branch to axillary nerve. J Hand Surg [Am] 29:131–139
BMC Public Health (2012) Body mass index (BMI) by country, Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (2011) http://www1.imperial.ac.uk/medicine/about/divisions/publichealth/eph/projects/eresh/majidezzati/
Chuang DC, Lee GW, Hashem F, Wei FC (1995) Restoration of shoulder abduction by nerve transfer in avulsed brachial plexus injury: evaluation of 99 patients with various nerve transfers. Plast Reconstr Surg 96:122–128
Cooley SM, Donnelly JC, Walsh T, Durnea U, Collins C, Rodeck CH, Hindmarsh PC, Geary MP (2011) The relationship between body mass index and mid-arm circumference in a pregnant population. J Obstet Gynaecol 31:594–596
Dong Z, Zhang CG, Gu YD (2010) Surgical outcome of phrenic nerve transfer to the anterior division of the upper trunk in treating brachial plexus avulsion. J Neurosurg 112:383–385
Elhassan B, Bishop AT, Hartzler RU, Shin AY, Spinner RJ (2012) Tendon transfer options about the shoulder in patients with brachial plexus injury. J Bone Joint Surg Am 94:1391–1398
Finucane MM, Stevens GA, Cowan MJ, Danaei G, Lin JK, Paciorek CJ, Singh GM, Gutierrez HR, Lu Y, Bahalim AN, Farzadfar F, Riley LM, Ezzati M (2011) National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet 377:557–567
Flores LP (2012) Clinical patterns of spontaneous recovery of paralyzed triceps brachii associated with C5 to C7 injuries of the brachial plexus. J Reconstr Microsurg 28:181–187
Jivan S, Kumar N, Wiberg M, Kay S (2009) The influence of pre- surgical delay on functional outcome after reconstruction of brachial plexus injuries. J Plast Reconstr Aesthet Surg 62:472–479
Khadivzadeh T (2002) Mid upper arm and calf circumferences as indicators of nutritional status in women of reproductive age. East Mediterr Health J 8:612–618
Luedemann W, Hamm M, Blömer U, Samii M, Tatagiba M (2002) Brachial plexus neurotization with donor phrenic nerves and its effect on pulmonary function. J Neurosurg 96:523–526
Malessy MJ, de Ruiter GC, de Boer KS, Thomeer RT (2004) Evaluation of suprascapular nerve neurotization after nerve graft or transfer in the treatment of brachial plexus traction lesions. J Neurosurg 101:377–389
Malessy MJ, van Duinen SG, Feirabend HK, Thomeer RT (1999) Correlation between histopathological findings in C-5 and C-6 nerve stumps and motor recovery following nerve grafting for repair of brachial plexus injury. J Neurosurg 91:636–644
Merrell GA, Barrie KA, Katz DL, Wolfe SW (2001) Results of nerve transfer techniques for restoration of shoulder and elbow function in the context of a meta-analysis of the English literature. J Hand Surg [Am] 26:303–314
Midha R (2004) Nerve transfers for severe brachial plexus injuries: a review. Neurosurg Focus 15:E5
Samii A, Carvalho GA, Samii M (2003) Brachial plexus injury: factors affecting functional outcome in spinal accessory nerve transfer for the restoration of elbow flexion. J Neurosurg 98:307–312
Socolovsky M, Di Masi G, Battaglia D (2011) Use of long autologous nerve grafts in brachial plexus reconstruction: factors that affect the outcome. Acta Neurochir 153:2231–2240
United Nations Department of Economic and Social Affairs Population Division (2011) World population prospects: the 2010 revision. CD-ROM Edition, UN, New York
WHO Global Infobase Team (2005) The SuRF report 2. Surveillance of chronic disease risk factors: country-level data and comparable estimates. World Health Organization, Geneva
Disclosure
No funding or financial support was received upon confection of the present paper by the authors.
This original material has never been presented or published previously.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Socolovsky, M., Di Masi, G., Bonilla, G. et al. Spinal to accessory nerve transfer in traumatic brachial plexus palsy: is body mass index a predictor of outcome?. Acta Neurochir 156, 159–163 (2014). https://doi.org/10.1007/s00701-013-1896-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-013-1896-5