Abstract
Background
The results of peripheral nerve repair, especially for high-level peripheral nerve injuries, have been unsatisfactory. The method of side-to-side neurorrhaphy was developed in our laboratory from 1994 to 2002. This method involves suturing the injured nerve to a nearby donor nerve in a side-to-side manner. This study was performed to assess the clinical results of side-to-side neurorrhaphy in patients with high-level peripheral nerve injuries.
Methods
Twenty-five patients with various types of high-level peripheral nerve injuries who underwent side-to-side neurorrhaphy were studied. The British Medical Research Council (BMRC) scale was used to assess recovery of nerve function.
Results
Average follow-up duration was 3.2 years. Before surgery the patients had a nerve function of M0/S0 to M1/S1. After side-to-side neurorrhaphy, 7 patients had a score of M3/S4, 8 patients a score of M3/S3 and 10 patients a score of M2/S3. The total useful recovery rate (BMRC grade ≥3) was 60% for motor function and 100% for sensory function. Side-to-side neurorrhaphy did not result in any significant loss of donor nerve function. There was significant correlation between both the type of injury and the time interval between injury and surgery and motor nerve function. Age, gender and location of the injured nerve did not correlate with sensory or motor nerve function.
Conclusion
Side-to-side neurorrhaphy appears to be promising as a feasible method for repair of high-level peripheral nerve injuries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The clinical results of peripheral nerve repair, especially repair of high-level peripheral nerve injuries, which are injuries that involve the long peripheral nerves that are above the first branch and are often distributed in the limbs, have been unsatisfactory despite the development of various techniques and instruments to perform peripheral nerve repair. A major obstacle to successful nerve reconnection with the target organ is the slow speed of nerve regrowth [11]. In high-level peripheral nerve injury there is a long distance from the injured site to the target organ, and atrophy of denervated skeletal muscles often occurs which may be irreversible.
Recently, additional techniques have been developed and applied clinically together with normal exploration and repair of peripheral nerve injury. These techniques use a donor nerve and include end-to-end neurorrhaphy, end-to-side neurorrhaphy and side-to-side neurorrhaphy. In end-to-end neurorrhaphy, the proximal end of a donor sensory nerve is connected to the caudal end of an injured motor nerve. It involves sacrifice of a normal sensory nerve [5, 8]. End-to-side neurorrhaphy without injury to the donor nerve or its innervated muscles was introduced in the early 1990s by Viterbo et al. [15, 16]. Many animal experiments [4, 10] and clinical practices [6, 9, 19] have shown that end-to-side neurorrhaphy has beneficial effects. Nevertheless, in end-to-side neurorrhaphy the donee nerve has to be cut, and the caudal end has to be coapted to the side of the donor nerve. In some kinds of injury, the nerve may not be completely damaged and cutting this nerve will cause additional functional loss. Moreover, Dvali and Myckatyn [3] have reviewed the literature on end-to-side nerve repair and concluded that although this technique results in some nerve regeneration, the regeneration is not robust.
Side-to-side neurorrhaphy was first developed by the first author (S.C. Zhang) in 1994. Laboratory studies suggest that this method effectively prevents muscle atrophy [7, 17, 24]. In a rat model, the peroneal nerve was transected, and the distal segment was sutured side-to-side to the neighboring tibial nerve. In the control leg, the peroneal nerve was resected for a length of 0.5 cm, and then the resected segment was reversely autografted at the same position. Three months later, the mass of the anterior tibial muscle and the cross-sectional areas of muscle fibers on the side-to-side neurorrhaphy side were similar to those on the nerve grafting side [17]. Yüksel et al. [18] reported that in both morphometric and gait analysis, the repair with the side-to-side method was better than with the end-to-side method in a rat model. Although the method has been applied clinically for many years in our department, the outcome has only been reported in Chinese [20–23, 25]. This report describes the clinical results of side-to-side neurorrhaphy in recent patients with high-level peripheral nerve injury.
Materials and Methods
General clinical data
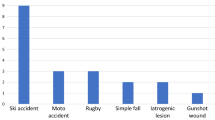
Twenty-five consecutive patients (16 male and 9 female) with high-level peripheral nerve injuries who were treated with side-to-side neurorrhaphy were studied (Table 1). The patients were selected for enrollment if they had a high-level peripheral nerve injury and had the possibility of having distal muscular atrophy. The ages of the patients ranged from 14 to 38 years (average, 26.0 ± 2.8 years). The type of injuries that the patients had are listed in Table 1. The patients were admitted from 1 day to 13 months (average, 5 months) after the injuries. This study was approved by the ethics board of Changhai Hospital. Informed consent was obtained from all patients.
Surgical technique and treatment
First, the patients received traditional exploration and repair of the injured nerve. The proximal and distal ends of a severed nerve were reconnected microsurgically by precisely aligning the fascicles, and autologous nerve grafting, which is used in cases where a nerve segment of significant length is missing, was carried out when necessary. End-to-end neurorrhaphy was performed at the injury point. Then side-to-side neurorrhaphy was performed downstream of the injured site between the distal end of the injured nerve and a nearby donor nerve.
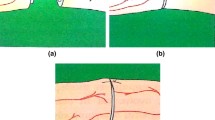
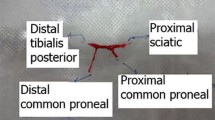
Side-to-side neurorrhaphy mainly involved motor nerves. The procedures are shown in Fig. 1. First, a relatively normal nerve root was identified as close as possible to the injured nerve to serve as the “donor” nerve. Then this “donor” nerve was drawn toward the injured nerve (the recipient nerve). For example, if the L4 and L5 lumbar root was injured, the common femoral nerve was chosen for side-to-side neurorrhaphy at the lower ventral thigh. If the lower trunk of the brachial plexus was injured, the ulnar and median nerves were chosen for side-to-side neurorrhaphy. Subsequently, the two nerves were placed closely abreast at an appropriate segment. Incisions 1 to 2 cm long, depending on nerve thickness, of the epineurium and partial perineurium were made at the neighboring sides (Fig. 1a). Then the incised epineurium and partial perineurium were sutured closely side to side with 9 to 11 monofilament nylon and microsurgical instruments (Figs. 1b-f). Nerve bundles were also sutured. Figure 2a shows the operation on patient 16 (Table 1), who received a knife injury in the upper thigh. After standard nerve repair, side-to-side neurorrhaphy was performed on the injured peripheral nerve using the tibial nerve as the donor nerve.
Schematic diagram of side-to-side neurorrhaphy: a. Epineurium incision of two neighboring nerves. b. Suture on one side of the epineurium. c. Incision of the perineurium. d. Suture on one side of the perineurium. e. Suture on another side of the perineurium. f. Suture on another side of the epineurium
After the operation, the limb with neurorrhaphy was immobilized with a cast for 3 to 4 weeks to avoid any tension on the sutured nerves. Finally, physical therapy and neurotropic medication were given.
Assessment of motor and sensory function
The British Medical Research Council (BMRC) scale was used to assess recovery of motor function. Scoring for motor function is based on the M system: M0 = no contraction; M1 = palpable contraction, barely visible; M2 = horizontally along the bed surface; M3 = against gravity only; M4 = against gravity and resistance; M5 = full strength. The key muscle innervated by the injured nerve was graded.
The BMRC scale was used to assess recovery of sensory function. Scoring for sensory function is based on the S system: S0 = no sensation; S1 = deep pain reestablished; S2 = some response to touch and pin, with over-response; S3 = good response to touch and pain, without over-response; S3+ = location and some tactile discrimination; S4 = complete recovery.
Statistical analysis
Statistical analyses were performed using SPSS 15.0 statistics software (SPSS Inc, Chicago, IL, USA). Continuous data were expressed as mean and standard deviation. Correlations between nerve functions and demographic and clinical variables were evaluated with Kendall’s rank-correlation method. P < 0.05 was considered significant.
Results
Before surgery, the BMRC scale scores were M0/S0 for ten patients, M0/S1 for seven patients and M1/S1 for eight patients (Table 1). The patients were followed up from 2 to 5 years (average, 3.2 years). Side-to-side neurorrhaphy improved both motor and sensory nerve function as indicated by the fact that seven patients had a BMRC score of M3/S4, eight a score of M3/S3 and ten a score of M2/S3. The total useful recovery rate (BMRC grade ≥3) was 60% for motor function and 100% for sensory function. Among them, seven patients obtained a motor function of “against gravity only” (M3) from “no contraction” (M0); seven patients’ sensory function was completely recovered (S4) from the level of “no sensation” (S0) or “deep pain reestablished” (S1). No significant functional reduction of the donor nerve was found in any patients. Only very few patients had atrophy. In four patients the function of the donor nerve decreased from M5/S5 to M4/S4. However, these patients completely recovered from 3 weeks to 3 months later (Fig. 2b). No complications directly related to side-to-side neurorrhaphy were observed.
Table 2 shows the correlations between nerve function after surgery and several demographic and clinical variables. According to Kendall’s rank-correlation coefficient, there were no significant correlations of sensory function with age, gender, type of injury, location of the injured nerve or the time interval between injury and surgery. However, motor function was significantly correlated with the type of injured nerve and time interval between injury and surgery (P < 0.05). We found that the longer the time interval between injury and surgery, the better the recovery of motor function (P = 0.001).
Discussion
Based on improvement in BMRC grades, our results showed that patients with high-level peripheral nerve injury had improved motor and sensory nerve function after side-to-side neurorrhaphy. As Table 1 demonstrates, there was improvement in sensory and motor nerve function following surgery based on assessment using the BMRC scale. These positive clinical results for side-to-side neurorrhaphy confirm the findings from animal studies in which this nerve repair technique has been used. We also found that there was significant correlation between both the type of injury and the time interval between injury and surgery and motor nerve function (Table 2). Age, gender and location of the injured nerve did not correlate with sensory or motor nerve function.
The poor results of peripheral nerve repair have been attributed to several factors, including prolonged denervation of the distal nerve stump resulting in a progressive reduction in the capacity of nerve stump Schwann cells and the long time that it takes many neurons to regenerate axons [13, 14]. Recently, it has been proposed that chronic Schwann cell denervation is the main cause of poor functional recovery, with muscle atrophy playing a lesser role [12]. Currently available methods of peripheral nerve repair often result in skeletal muscle atrophy. Therefore, the availability of an effective method to keep the denervated skeletal muscle from undergoing atrophy until the regenerating nerve reaches the muscle has been considered to be very important.
In 1992, Viterbo and colleagues [15], who used end-to-side neurorrhaphy, reported that axons can grow from an intact donor nerve to the distal end of a recipient nerve. Improvement was also reported for a patient who received end-to-side neurorrhaphy of the accessory nerve to the suprascapular nerve [9]. An attempt to use end-to-side neurorrhaphy in a patient with severe upper-extremity nerve injuries resulted in improvement, with the patient being able to return to work [19].
Side-to-side neurorrhaphy was first used in a clinical trial by our group to treat localized spasm cerebral palsy [21, 23], paralysis [20] and peripheral nerve injury [22, 24, 25]. In 2000, we reported that 6 out of 16 patients with spastic cerebral palsy who underwent side-to-side neurorrhaphy had no spasm without extra stimulation and had recovery of the main limb functions [23]. In another study, we compared the outcome of operations with and without side-to-side neurorrhaphy on patients with high-level nerve injury. Among 21 patients receiving normal nerve repair and side-to-side neurorrhaphy, 5 had nerve function of M4/S4, 8 M3/S3, 5 M3/S2 and 3 M2/S2 after 2–5 years of follow-up. By contrast, none of 21 patients with similar preoperative injury and receiving only normal nerve repair had a function of M4/S4 [22]. Recently, Yüksel et al. reported satisfactory results in a patient who had side-to-side nerve neurorrhaphy between the ulnar and median nerves [19]. A combination of end-to-side and side-to-side neurorrhaphy was applied in 11 patients with brachial plexus lesions [2] and 5 patients with complete traumatic brachial plexus palsy by Amr’s group [1]. The improved outcomes in these studies are consistent with our observations.
Although experimental evidence shows that muscle denervation atrophy plays a secondary role in poor functional recovery after nerve injuries [12], we observed that side-to-side neurorrhaphy reduces muscle atrophy in a rat model [17] and in previous clinical reports [22] as well as in this clinical study. However, we cannot exclude the possibility that involvement of trophic effects on Schwann cells contributes to the outcome of side-to-side neurorrhaphy. However, regardless of the relative roles of muscle atrophy and chronic Schwann cell denervation in poor functional recovery, our clinical outcomes and some clinical outcomes of others suggest that side-to-side neurorrhaphy combined with routine nerve repair is an effective method for the treatment of high-level peripheral nerve injury.
It should be noted that there are some important limitations to the method of side-to-side neurorrhaphy. For example, the availability of a normal donor nerve near the injured nerve is necessary. Also, advanced knowledge of peripheral nerve anatomy and skill in performing microsurgical techniques are required for application of this method. In addition, this study had a small sample size, and our patients had different types of nerve injuries rather than one type, making the findings more difficult to interpret. To obtain more definitive data on the clinical value of side-to-side neurorrhaphy prospectively, randomized studies are needed comparing patients receiving side-to-side neurorrhaphy with those receiving no side-to-side neurorrhaphy after conventional procedures.
Conclusions
The results of this clinical study indicate that the method of side-to-side neurorrhaphy, which does not block nerve regeneration in the injured nerve and does not significantly harm the normal donor nerve, is feasible and improves motor and sensory nerve function. For high-level peripheral nerve injury, because of poor outcome due to the long duration of nerve recovery at a low level distally, we recommend using side-to-side neurorrhaphy.
References
Amr SM, Essam AM, Abdel-Meguid AM, Kholeif AM, Moharram AN, El-Sadek RE (2009) Direct cord implantation in brachial plexus avulsions: revised technique using a single stage combined anterior (first) posterior (second) approach and end-to-side side-to-side grafting neurorrhaphy. J Brachial Plex Peripher Nerve Inj 4:8
Amr SM, Moharram AN (2005) Repair of brachial plexus lesions by end-to-side side-to-side grafting neurorrhaphy: experience based on 11 cases. Microsurgery 25:126–146
Dvali LT, Myckatyn TM (2008) End-to-side nerve repair: review of the literature and clinical indications. Hand Clin 24:455–460
Hong GX, Zheng Y, Wang FB, Wan SX, Chen ZB (1998) The study on the nerve regeneration of end-to-side neurorrhaphy after peripheral nerve injury. Chinese J Hand Surg 14:42–44 (in Chinese)
Hynes NM, Bain JR, Thoma A, Veltri K, Maguire JA (1997) Preservation of denervated muscle by sensory protection in rats. J Reconstr Microsurg 13:337–343
Lundborg G, Zhao Q, Kanje M, Danielsen N, Kerns JM (1994) Can sensory and motor collateral sprouting be induced from intact peripheral nerve by end-to-side anastomosis? J Hand Surg Brit Eur 19:277–282
Ma YH, Zhang SC, Cao L, He C, Jia BC (2002) Experimental study of peripheral nerve regeneration after side-to-side neurorrhaphy in rabbits. Chin Int J Med 2:206–210 (in Chinese)
Papakonstantinou KC, Kamin E, Terzis JK (2002) Muscle preservation by prolongled sensory protection. J Reconstr Microsurg 18:173–184
Ray WZ, Kasukurthi R, Yee A, Mackinnon SE (2010) Functional recovery following an end to side neurorrhaphy of the accessory nerve to the suprascapular nerve: case report. Hand (NY) 5:313–317
Song C, Oswald T, Yan H, Chen MB, Zhang J, Chen T, Lineaweaver WC, Zhang F (2009) Repair of partial nerve injury by bypass nerve grafting with end-to-side neurorrhaphy. J Reconstr Microsurg 25:507–515
Stoll G, Müller HW (1999) Nerve injury, axonal degeneration and neural regeneration: basic insights. Brain Pathol 9:313–325
Sulaiman OA, Gordon T (2009) Role of chronic schwann cell denervation in poor functional recovery after nerve injuries and experimental strategies to combat it. Neurosurgery 65(4 Suppl):A105–A114
Sulaiman OAR, Boyd JG, Gordon T (2004) Neuroglia. In: Kettenmann H, Ransom BR (eds) Regeneration in the peripheral nervous system of mammals, 2nd edn. Oxford University Press, Oxford, pp 454–466
Sulaiman WA, Kline DG (2006) Nerve surgery: a review and insights about its future. Clin Neurosurg 53:38–47
Viterbo F, Amr AH, Stipp EJ, Reis FJ (2009) End-to-side neurorrhaphy: past, present, and future. Plast Reconstr Surg 124(6 Suppl):e351–e358
Viterbo F, Trindade JC, Hoshino K, Mazzoni A (1994) Two end-to-side neurorrhaphies and nerve graft with removal of the epineural sheath: experimental study in rats. Br J Plast Surg 47:75–80
Xiu XL, Zhang SC, Xu SG, Chen Y, Yu BQ, Zheng XD (2000) Experimental study of peripheral nerve side-to-side neurorrhaphy. Chin J Orthopaed 20:583–585 (in Chinese)
Yüksel F, Karacaoğlu E, Güler MM (1999) Nerve regeneration through side-to-side neurorrhaphy sites in a rat model: a new concept in peripheral nerve surgery. Plast Reconstr Surg 104:2092–2099
Yüksel F, Peker F, Celiköz B (2004) Two applications of end-to-side nerve neurorrhaphy in severe upper-extremity nerve injuries. Microsurgery 24:363–368
Zhang SC, Guo FL, Yan GZ, Ma YH, Jia JP, Wu CH, Xiu XL (2002) The reconstruction of sensory function for paralysis patients with side-to-side neurorrhaphy. Orthoped J China 9:987–988 (in Chinese)
Zhang SC, Luo CL, Zhang XS (2001) Spastic cerebral palsy treatment with side-to-side neuroanastemosis. J Neurol Orthopaed Med Surg 21:307–310 (in Chinese)
Zhang SC, Ma YH, Sun LQ, Zhu YZ, Fu Q, Zhang YP, Zhang QL (2005) Prevention of irreversible muscle atrophy after high-level nerve injury by side-to-side neurorrhaphy. Chin J Orthopaed Trauma 7:335–337 (in Chinese)
Zhang SC, Xiu XL, Huang P, Li QT, Yao YP (2000) The treatment of spasmic cerebral palsy patients with side-to-side neurorrhaphy. Academic Journal of Second Military Medical University 21:395–396 (in Chinese)
Zhang SC, Xiu XL, Yu BQ, Cai ZD, Dang RS, Xu JJ (1999) Experimental study and primary clinical report on peripheral nerve side-to-side neurorrhaphy. Chin J Anat 22:314 (in Chinese)
Zhang SC, Zhang XS, Nian SS, Wang JL, Pan YT, Yu BQ, Li M, Shi ZC, Liu HR, Zheng XD, Wang SP, Hou HC, Li ZQ (2002) Treatment of peripheral nerve injury with side-to-side anastomosis. Chin J Orthopaed 22:398–401 (in Chinese)
Conflicts of interest
None.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding authors
Additional information
ShaoCheng Zhang and Fang Ji contributed equally to this work.
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Zhang, S., Ji, F., Tong, D. et al. Side-to-side neurorrhaphy for high-level peripheral nerve injuries. Acta Neurochir 154, 527–532 (2012). https://doi.org/10.1007/s00701-011-1264-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-011-1264-2