Abstract
Background
Brainstem surgery bears a risk of damage to the corticospinal tract (CST). Motor-evoked potentials (MEPs) are used intraoperatively to monitor CST function in order to detect CST damage at a reversible stage and thus impede permanent neurological deficits. While the method of MEP is generally accepted, warning criteria in the context of brainstem surgery still have to be agreed on.
Method
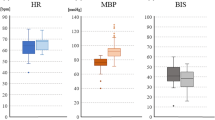
We analyzed 104 consecutive patients who underwent microsurgical resection of lesions affecting the brainstem. Motor grade was documented prior to surgery, early postoperatively and at discharge. A baseline MEP stimulation intensity threshold was defined and intraoperative testing aimed to keep MEP response amplitude constant. MEPs were considered deteriorated and the surgical team was notified whenever the threshold was elevated by ≥20 mA or MEP response fell under 50%.
Findings
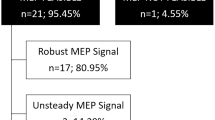
On the first postoperative day, 18 patients experienced new paresis that resolved by discharge in 11. MEPs deteriorated in 39 patients, and 16 of these showed new postoperative paresis, indicating a 41% risk of new paresis. In the remaining 2/18 patients, intraoperative MEPs were stable, although new paresis appeared postoperatively. In one of these patients, intraoperative hemorrhage caused postoperative swelling, and the new motor deficit persisted until discharge. Of all 104 patients, 7 deteriorated in motor grade at discharge, 92 remained unchanged, and 5 patients have improved.
Conclusions
Adjustment of surgical strategy contributed to good motor outcome in 33/39 patients. MEP monitoring may help significantly to prevent motor deficits during demanding neurosurgical procedures on the brainstem.



Similar content being viewed by others
References
Calancie B, Molano MR (2008) Alarm criteria for motor-evoked potentials: what's wrong with the "presence-or-absence" approach? Spine 33:406–414
Deletis V, Rodi Z, Amassian VE (2001) Neurophysiological mechanisms underlying motor evoked potentials in anesthetized humans. Part 2. Relationship between epidurally and muscle recorded MEPs in man. Clin Neurophysiol 112:445–452
Kang DZ, Wu ZY, Lan Q, Yu LH, Lin ZY, Wang CY, Lin YX (2007) Combined monitoring of evoked potentials during microsurgery for lesions adjacent to the brainstem and intracranial aneurysms. Chin Med J (Engl) 120:1567–1573
Kombos T, Süss O (2009) Neurophysiological basis of direct cortical stimulation and applied neuroanatomy of the motor cortex: a review. Neurosurg Focus 27:E3
Kothbauer KF, Deletis V, Epstein FJ (1998) Motor-evoked potential monitoring for intramedullary spinal cord tumor surgery: correlation of clinical and neurophysiological data in a series of 100 consecutive procedures. Neurosurg Focus 4:e1
Lieberman JA, Lyon R, Feiner J, Diab M, Gregory GA (2006) The effect of age on motor evoked potentials in children under propofol/isoflurane anesthesia. Anesth Analg 103:316–321
Lyon R, Feiner J, Lieberman JA (2005) Progressive suppression of motor evoked potentials during general anesthesia: the phenomenon of "anesthetic fade". J Neurosurg Anesthesiol 17:13–19
MacDonald DB (2006) Intraoperative motor evoked potential monitoring: overview and update. J Clin Monit Comput 20:347–377
Møller AR (2006) Intraoperative Neurophysiological Monitoring. Humana Press Totowa, NJ
Neuloh G, Pechstein U, Cedzich C, Schramm J (2004) Motor evoked potential monitoring with supratentorial surgery. Neurosurgery 54:1061–1070, discussion 1070–1062
Neuloh G, Pechstein U, Schramm J (2007) Motor tract monitoring during insular glioma surgery. J Neurosurg 106:582–592
Neuloh G, Bogucki J, Schramm J (2009) Intraoperative preservation of corticospinal function in the brainstem. J Neurol Neurosurg Psychiatry 80:417–422
Neuloh G, Schramm J (2009) Are there false-negative results of motor evoked potential monitoring in brain surgery? Cen Eur Neurosurg 70:171–175
Quinones-Hinojosa A, Alam M, Lyon R, Yingling CD, Lawton MT (2004) Transcranial motor evoked potentials during basilar artery aneurysm surgery: technique application for 30 consecutive patients. Neurosurgery 54:916–924, discussion 924
Sala F, Palandri G, Basso E, Lanteri P, Deletis V, Faccioli F, Bricolo A (2006) Motor evoked potential monitoring improves outcome after surgery for intramedullary spinal cord tumors: a historical control study. Neurosurgery 58:1129–1143, discussion 1129–1143
Sutter M, Eggspühler A, Grob D, Jeszenszky D, Benini A, Porchet F, Mueller A, Dvorak J (2007) The diagnostic value of multimodal intraoperative monitoring (MIOM) during spine surgery: a prospective study of 1,017 patients. Eur Spine J 16(Suppl 2):S162–S170
Szelenyi A, Langer D, Kothbauer K, De Camargo AB, Flamm ES, Deletis V (2006) Monitoring of muscle motor evoked potentials during cerebral aneurysm surgery: intraoperative changes and postoperative outcome. J Neurosurg 105:675–681
Szelenyi A, Kothbauer KF, Deletis V (2007) Transcranial electric stimulation for intraoperative motor evoked potential monitoring: Stimulation parameters and electrode montages. Clin Neurophysiol 118:1586–1595
Szelenyi A, Hattingen E, Weidauer S, Seifert V, Ziemann U (2010) Intraoperative motor evoked potential alteration in intracranial tumor surgery and its relation to signal alteration in postoperative magnetic resonance imaging. Neurosurgery 67:302–313
Weinzierl MR, Reinacher P, Gilsbach JM, Rohde V (2007) Combined motor and somatosensory evoked potentials for intraoperative monitoring: intra- and postoperative data in a series of 69 operations. Neurosurg Rev 30:109–116, discussion 116
Acknowledgements
We thank Dr. M. Bjeljac and E. Ciessynna for their help with MEP recordings in this case series.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comment
In this article the authors report their experience with the use of IOM with MEPs in the resection of brainstem (BS) lesions. Surgery of brainstem lesions is certainly not free of potential ominous consequences, which makes the use of any intra-operative real time monitoring of nervous function located within the stem all the more important. The authors are therefore to be commended for their effort in trying to come up with clearer and more objective clinical rules to be pursued during these operations. The series is significant, although it includes a wide mixture of lesions differently affecting the BS.
The distinction between extra- and intra-axial lesions follows criteria that are not strictly related to the intrinsic nature of the lesion itself (i.e., ependymoma in the extra-axial group), but also according to the topography of the pathological growth to be excised.
As expected, lesions that grow outside the BS evoke fewer intra-operative MEP changes than those intimately arising from the cellular patrimony of the stem.
Reasons for neuroelectric MEP changes are several. The latency period between the initial aggression and the establishment of the predictable changes in MEPs is variable, as is the mechanism of the insult. Also, some changes may be severe but reversible, whereas others are not.
As mentioned in the text, mechanical causes may tend to evoke more immediate changes, whereas vascular (especially venous) insult or 'edema' may have a significant delay despite the fact that the consequences may end up being worse. The authors clearly demonstrate that they are well aware of the current limitations and caveats involved with the translation of the neurophysiological information into intraoperative surgical decisions.
The heart of the matter is that this technology is no longer dispensable given the possible adverse effects of the surgical manipulation of the BS and the need to minimize it. On the other hand we need clearer indications of what the intraoperative neurophsysiologic changes really mean in terms of determining transient or permanent morbidity so that we can act accordingly, either continuing to pursue the resection of the lesion or stopping short of doing so. The third alternative is to alter the surgical strategy, which is what the authors allude to in their text.
This issue is not without importance because there is little one can change in a pristine microsurgical technique itself; what can be altered is, essentially, the location of the dissection or the degree of the resection.
The results are very clearly documented. All patients who deteriorated postoperatively had intra-operative changes signaled to the surgeon. This means that despite the warning and the eventual change in strategy, not all consequences could be avoided.
What advice is there from the surgeon's standpoint taking into consideration the fact that in only 41% of cases did the deterioration of the warning signs predict a new motor deficit? This in fact is the bottom line: Should these warnings forbid us from pursuing a more radical resection or should one still carry on with it?
Of course, experience is foremost and the key to the question, albeit subjective, before we can come up with absolute boundaries for these IOM changes (MEP or others) more independent from the eye and soul of the surgeon, and the monitoring equipment as well.
Manuel Cunha e Sa
Almada, Portugal
Rights and permissions
About this article
Cite this article
Sarnthein, J., Bozinov, O., Melone, A.G. et al. Motor-evoked potentials (MEP) during brainstem surgery to preserve corticospinal function. Acta Neurochir 153, 1753–1759 (2011). https://doi.org/10.1007/s00701-011-1065-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-011-1065-7