Abstract
The development of cost-effective, portable, and ease-of-use sensing system for on-site genetic diagnostics is highly desirable for pathogen screening and infectious disease diagnosis. This study develops (1) a paper-based biochip which is able to integrate the loop-mediated isothermal amplification (LAMP) protocols for simultaneous detection of Escherichia coli O157:H7, Salmonella spp., and Staphylococcus aureus, and (2) a stand-alone smartphone-based portable device which can control exactly 65 °C for isothermal amplification as well as collect and analyze the thus generated fluorescence signals. The reported sensing system has been successfully demonstrated for foodborne pathogen detection with a limit of detection of 2.8 × 10−5 ng μL−1. Spiked milk samples with concentration as low as 10 CFU mL−1 were successfully determined within 4 h, demonstrating the practicality of the reported sensing system in the fields. The reported sensing system featuring simplicity and reliability is ideally suited for genetic diagnostics in low resource settings.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Foodborne illness, mostly caused by biological contaminants such as bacteria, viruses, and parasites, constitute a global health threat. As reported by the World Health Organization (WHO), over 400,000 deaths annually are caused by foodborne illness worldwide [1,2,3]. Escherichia coli O157:H7 (E. coli O157:H7), Salmonella spp., and Staphylococcus aureus (S. aureus) are considered to be the most common foodborne pathogens causing most of food-related human illnesses worldwide [3]. In order to effectively control the spread of foodborne illness and decrease their severity, it is crucial to develop rapid and simple methods to determine foodborne pathogens at the points of contamination and/or consumption [4,5,6,7,8,9,10]. At present, culture-based protocols, immunoassays, as well as nucleic acid amplification tests, are the extensively used methods for foodborne pathogen determination [8,9,10]. Among them, the nucleic acid amplification test is becoming the golden standard, since they can directly detect DNA/RNA of pathogens with high sensitivity and specificity.
In a conventional polymerase chain reaction (PCR) test, a specific genetic locus can be exponentially amplified to trillions of copies via thermal recombination of nucleic acids under thermal cycle operations. However, this sophisticated thermocyclers and multiple temperature controls of conventional PCR limit their applications in point-of-care testing (POCT) [11, 12]. To address this critical issue, various isothermal amplification approaches which eliminate thermal cyclers have been discovered, including enzyme-assisted amplification strategies such as loop-mediated isothermal amplification (LAMP) [13,14,15], rolling circle amplification (RCA) [16], recombinase polymerase amplification (RPA) [17], helicase-dependent amplification (HDA) [18], nucleic acid sequence–based amplification (NASBA) [19], strand displacement amplification (SDA) [20], rolling circle transcription (RCT) [21], and enzyme-free amplification strategies such as hybridization chain reaction (HCR) [22] and catalytic hairpin assembly (CHA) [23].
Especially, due to its advantages such as one-step reactions, excellent specificity, amplification at a relatively low temperature, and high resistance to possible inhibitors in clinical samples, LAMP is becoming an ideal isothermal amplification technique for POCT applications. Especially, LAMP has been intensively used to develop sample-in-answer-out microdevices [4, 5, 11,12,13,14,15, 24,25,26]. For example, LAMP technique has been well integrated with microfluidic chip to develop internet of things (IoT)–based POCT device for simultaneous analysis of As1e, N, and E genes of SARS-CoV-2 [14].
However, to realize the determination of foodborne pathogens at the points of need, the challenge still exists in the lack of portable devices which can provide accurate temperature control for isothermal amplification and precisely collect detection signals generated by amplification reaction. Recently, smartphones can be readily conditioned to develop easy-to-use portable devices for POCT applications, by taking advantages of their powerful built-in sensors, advanced computing capability, as well as user-friendly operation interface. Smartphone-based sensing devices can facilitate point-of-need detection in resource-constrained environments, because smartphone can simplify the instrument design by serving as detector, monitor, as well as laptop computers simultaneously [14, 15, 24, 27,28,29,30,31,32,33,34,35].
Herein, a portable device was developed for on-site amplification and detection of nucleic acids in elementary conditions through integrating a smartphone with specifically designed peripheral accessories: a 3D-printed imaging dark box integrated with optical elements, a heating plate connected with the temperature control circuit module, and a chip interface. In order to achieve on-site high-throughput analysis, a paper-based biochip was designed for the integration of LAMP protocols and subsequent fluorometric detection of multiple foodborne pathogens. An open-source Android APP was used for extracting RGB value of fluorescence images of biochips for data analysis. The smartphone-based portable device integrated with paper-based biochips is successfully applied to multiplexed detection of E. coli O157:H7, Salmonella spp., and S. aureus in milk (Scheme 1). Notably, the following distinctive features highlight the advantages of this study: (1) accurate temperature control guarantees the successful amplification of DNA/RNA, (2) uniform excitation of the fluorophores on the chip guarantees the precise detection, and (3) simultaneous detection of three analytes with minimal manual operation as well as reagent consumption.
Schematic illustration of the on-site detection of foodborne pathogens using a paper-based biochip which integrate the LAMP protocols and a smartphone-based portable device which can control the exact 65 °C for isothermal amplification as well as collect and analyze the thus generated fluorescence signals
Experimental
Materials
The LAMP reagent containing Bst 2.0 WarmStart DNA polymerase, 10 × isothermal amplification buffer, 100 mM MgSO4 and dNTPs, was purchased from New England BioLabs (Ipswich, MA, USA). Primers, plasmid DNA (pDNA) of E. coli O157:H7, Salmonella spp. and S. aureus, and agarose powder were obtained from Sangon (Shanghai, China). MnCl2 and Calcein (CAS No.: 154071–48-4, C30H26N2O13, 2,2′,2″,2″′-[(3′,6′-dihydroxy-3-oxo-3H-spiro[2-benzofuran-1,9′-xanthene]-2′,7′-diyl)bis (methanediylnitrilo)] tetraacetic acid) were purchased from Macklin (Shanghai, China) and Sigma-Aldrich (St. Louis, MO, USA), respectively. PDMS prepolymer (Sylgard 184) and curing agent were obtained from Dow Corning. Whatman filter paper grade 1 and Gel-Red was purchased from Beyotime Biotechnology (Shanghai, China). The Wizard genomic DNA purification kit was obtained from Promega (Madison, WI, USA). S. aureus real-time PCR kit was purchased from Zeye Biotechnology (Shanghai, China). A 100 bp DNA size marker was obtained from Sparkjade Biotechnology (Shandong, China). Loading buffer was purchased from Dingguo Biotechnology (Beijing, China). 50 × TAE buffer was purchased from YuanYe Biotechnology (Shanghai, China). Clinx Gel imaging system (Shanghai, China) was used to detect the target bands.
LAMP protocols for detection of E. coli O157:H7, Salmonella spp. and S. aureus
The eaeA gene of E. coli O157:H7, the invA gene of Salmonella spp., and the nuc gene of S. aureus are selected as target genes, according to previous reports [4]. PrimerExplorer V5 (http://primerexplorer.jp/e/) is used to design primers, and BLAST search is performed to verify the primers [6]. Table S1 and Table S2 list all the primer sequences and experimental details for LAMP reactions which are performed at 65 °C for 30 min, respectively. The combination of calcein and Mn2+ is used as the fluorescent indicator of successful amplification, due to its low cost, field applicability as well as insignificant inhibition on LAMP process [36, 37].
Fabrication of the paper-based isothermal amplification chip
To fabricate the isothermal amplification biochip, Whatman filter paper (grade 1) is used as the substrate [21, 38]. The whole fabrication process is illustrated in Fig. 1a and Video S1. In brief, the paper-based biochip consists of two separate functional zones: one reaction zone (30 × 30 mm) and one detection zone (30 × 30 mm). Each functional zone contains eight identical circular reaction chambers (6 mm in diameter) which are created on paper substrates by compressing a set of 3D-printed molds with complementary shapes (step 1). To prevent possible leakage and/or evaporation of reagents during isothermal amplification, PDMS was used as sealing material. The paper with embossed pattern was immersed in a mixture of PDMS prepolymer and curing agent (w/w, 10:1) for 5 min (step 2). Then, a PDMS layer (1 mm thick) with eight holes (6 mm in diameter) was attached onto the paper-based biochip by being aligned with the chambers created on the paper (step 3). After being baked in the oven at 80 °C overnight, the reaction zone of paper-based biochip was sealed with another PDMS layer (1 mm thick), followed by being baked in the oven at 80 °C for 2 days (step 4). Finally, eight paper discs (6 mm in diameter) were prepared and fixed onto the eight chambers created on the detection zone of paper-based biochip (step 5).
a Schematic images illustrating the step-by-step fabrication process of the paper-based biochip; b–c SEM images of the paper-based biochip before (b) and after (c) PDMS modification. The upper right inset in each image presents its water contact angles, whereas the lower left inset shows the photograph of red ink droplets dripped on paper.
Finally, the LAMP reagents are pre-loaded into the reaction chambers on the reaction zone to prepare the paper-based biochips which are stored at 4 °C refrigerator before usage. Specifically, to fabricate the paper-based biochips for simultaneous detection of multiple pathogens, each two chambers are loaded with one kind of primer for duplicated detections, and the remaining two chambers are used as the negative control. For example, as illustrated in Figure S1, primers for E. coli O157:H7, Salmonella spp. as well as S. aureus are pre-loaded to prepare a typical biochip to demonstrate multiplexed analysis of E. coli O157:H7, Salmonella spp., and S. aureus.
Fabrication of the smartphone-based portable device
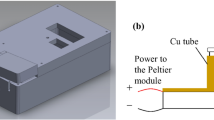
As illustrated in Fig. 2, the smartphone-based portable device consists of the following main parts: (1) an adaptor (Fig. 2b, 118.7 mm × 81.0 mm × 18.6 mm) for smartphone assembly; (2) a mini image dark box (Fig. 2b, 65.2 mm × 72.4 mm × 93.8 mm) contains (3) two UV lamp beads (300–310 nm, 10–15 mW) serving as the excitation light source, (4) a heating plate (Fig. 2b, 35.0 mm × 35.0 mm), and (5) a temperature control module (Fig. 2b, 40.5 mm × 48.5 mm). The whole device is fabricated by a HP Jet Fusion 3D 3200 printer, and Multi-Jet Fusion Nylon is used as the printing material. In this study, a Redmi K40 smartphone which equips a 48-megapixel backside-illuminated IMX582 sensor (ISO 800; f: 1.79), was used for the fluorescence image capture.
a Schematic illustration of main components of the smartphone-based portable device, including a heating plate connected with a temperature control circuit module, a 3D-printed imaging dark box integrated with optical elements, a chip interface and an adaptor. b Detailed size information are displayed in photograph of the actual smartphone-based portable device. c A block diagram of the temperature control circuit module. d Photograph of the actual temperature control circuit module. e Real-time temperature change curve of the heating plate connected with the temperature control circuit module.
Multiplexed detection of foodborne pathogens
The genomic DNA (gDNA) of Salmonella spp. was used to determine the sensitivity and selectivity of paper-based biochip for pathogen detection. To determine the sensitivity of paper-based biochip, 5 μL of Salmonella spp. gDNA with different concentrations (2.8 × 10−7, 2.8 × 10−6, 2.8 × 10−5, 2.8 × 10−4, 2.8 × 10−3 and 2.8 × 10−2 ng μL−1) was added into the chambers in reaction zone of the biochip. To evaluate the selectivity of paper-based biochip, 5 μL of Salmonella spp. gDNA (2.8 × 10−5 ng μL−1) was added into three different chambers in reaction zone of the biochip which were pre-loaded with primers for E. coli O157:H7, Salmonella spp., and S. aureus, respectively. Then, the biochip was inserted into the smartphone-based portable device for amplification at 65 °C for 30 min. To validate the device for the successful amplification of nucleic acid, the products were subjected to gel electrophoresis, and the obtained gels were analyzed in Clinx Gel imaging system (Shanghai Qinxiang, China). In addition, to validate the device as a stand-alone device, the products were also transferred to the discs fixed on the detection zone of the biochip and thereafter subjected to the device for fluorescence image capture and further analysis. Figure S2 illustrated the key steps involved in the fabrication of the paper-based isothermal amplification chip, and using the smartphone-based portable device for amplification and thereafter collection of detection signals.
Multiplexed detection of E. coli O157:H7, Salmonella spp., and S. aureus were demonstrated using the paper-based isothermal amplification chip and the smartphone-based portable device (Video S1). In brief, a mixed solution containing gDNA with different combination was added to the isothermal amplification chip. Then, the biochip was inserted into the smartphone-based portable device for amplification at 65 °C for 30 min. At last, gel electrophoresis and the smartphone-based portable device were used to collect and analyze the results.
Spiked sample analysis
To validate its practicability, the reported system was used to analyze the artificially contaminated milk samples. In brief, 1.0 mL S. aureus solution (1.5 × 108 CFU mL−1) was added into 0.5 mL milk to prepare stock solution, followed by stepwise dilution using milk to obtain the spiked samples with different concentrations (100, 101, 102, 103, 104 CFU mL−1). Then, following the standard protocol provided by the manufacturer (please refer to Supplementary Information for more details), 1 mL of the spiked milk was used for gDNA extraction via DNA purification kit at the Clinical Laboratory of the Seventh Affiliated Hospital of Sun Yat-sen University. Finally, the purified gDNA was added to the paper-based biochip and subjected to the smartphone-based portable device for isothermal amplification and data collection.
Results and discussion
LAMP protocols for E. coli O157:H7, Salmonella spp., and S. aureus
Due to the elimination of sophisticated thermocyclers and multiple temperature controls, LAMP can substantially simplify portable device design for POCT applications. Herein, LAMP protocols for the detection of E. coli O157:H7, Salmonella spp., and S. aureus were established in this study. Figure S3 demonstrated the detection of LAMP amplicons after a 30-min reaction inside the tube heated at 65 °C. Obvious gel bands (Figure S3a–S3c) and green fluorescence (Figure S3d–S3f) can only be observed when the concentration of pDNA reaches to 6.4 × 10−7 ng μL−1, suggesting the limit of detection (LOD) for E. coli O157:H7, Salmonella spp., and S. aureus using this LAMP protocols inside the tube is 6.4 × 10−7 ng μL−1.
LAMP mainly depends on three sets of specially designed primers and polymerase with high strand displacement activity to amplify six gene regions of target DNA, ensuring high specificity. As anticipated, only LAMP amplicons of E. coli O157:H7 can be detected in the presence of E. coli O157:H7 primers (lane 1 of Figure S4a and tube 1 of Figure S4d). Similarly, only LAMP amplicons of Salmonella spp. and S. aureus can be detected in the presence of Salmonella spp. primers (lane 1 of Figure S4b and tube 1 of Figure S4e) and S. aureus primers (lane 1 of Figure S4c and tube 1 of Figure S4f), respectively. These results validate good specificity of the established LAMP protocols for detection of E. coli O157:H7, Salmonella spp., and S. aureus.
The paper-based isothermal amplification chip
To achieve on-site high-throughput analysis, the established LAMP protocols are integrated into a paper-based biochip. Figure 1a and Figure S5 illustrated the whole fabrication process of the paper-based isothermal amplification chip. PDMS is used as sealing material to prevent possible leakage of LAMP reagents as well as aerosol pollution by immersing the paper with embossed pattern into a mixture of PDMS prepolymer and curing agent [26]. As shown in Fig. 1b, before PDMS modification, the scanning electron microscopy (SEM) image of filter paper revealed a highly porous matrix formed by the overlapping cellulose fiber networks. However, after PDMS modification, the SEM image of filter paper exhibited a planar surface (Fig. 1c). The water contact angle of the filter paper surface changed from < 3° to 94 ± 2.5°, suggesting the hydrophilicity-to-hydrophobicity change of the chip surface after PDMS modification. These results correlated well with observation that red ink completely penetrated into the filter paper before PDMS modification (inset of Fig. 1b), while formed a droplet after PDMS modification (inset of Fig. 1c). All the above results verified the successful modification of the filter paper with PDMS, laying a solid foundation for the fabrication of isothermal amplification chip.
To well integrate the established LAMP protocols into paper-based biochips, a series of key parameters, such as the ratio of calcein/Mn2+ and the excitation resource, are carefully optimized. In this study, the combination of calcein and Mn2+ is used as the fluorescent indicator for the LAMP reaction, because the fluorescence of calcein is quenched by Mn2+ but will be restored by pyrophosphate ions (PPi) produced by the successful amplification of nucleic acids [36, 37]. As shown in Figure S6 and Figure S7, the optimal ratio of calcein/Mn2+ is 0.05 M/0.6 M, while 302 nm is the optimal wavelength for the excitation of calcein on the paper-based biochips.
The smartphone-based portable device
To realize on-site amplification and detection of nucleic acids in elementary conditions, peripheral accessories are designed and attached to a smartphone to assemble a portable device. As shown in Figs. 2a, b and S8, the smartphone-based portable device consists of the following main components are (1) a heating plate connected with a temperature control circuit module to provide proper temperature for isothermal amplification, (2) a 3D-printed imaging dark box (Figure S8a) integrated with optical elements for uniform excitation and precise collection of fluorescent signals generated by amplification reaction, (3) a chip interface (Figure S8b) for loading the paper-based isothermal amplification chip, and (4) an adaptor (Figure S8c) for assembling a smartphone which is used for signal collection and further analysis.
For a typical LAMP reaction, the temperature should be fixed at 65 °C to ensure the successful amplification of nucleic acids. Therefore, in this study, the classical proportion-integral–differential (PID) closed-loop controller is used for temperature control. Figure 2c illustrated the block diagram of the temperature control circuit module which is mainly consisted of a microcontroller unit (MCU), a relay, a temperature sensor, a regulator IC and a three-bit LED display. In this design, the temperature sensor detects the real-time temperature of the heating plate which is displayed on the three-bit LED display, the regulator IC connected with biasing resistors outputs proper working voltage for the relay and MCU, and the relay decides the on-and-off of the power supply of the heating plate (Fig. 2d). While the system is operating, the MCU, which has a built-in pulse width modulation (PWM) and analog to digital converter (ADC), is responsible to collect the temperature information from the temperature sensor and send instructions to the relay. Specifically, the power of the relay is controlled by the pulse exported from MCU to execute the automatic temperature control instruction, while the frequency and duty ratio of the pulse is generated according to the control law based on the temperature sensor’s feedback. As designed, the temperature of the heating plate could be fixed in the range of 64.7–65.5 °C, ensuring proper temperature for the LAMP reaction (Fig. 2e). It is noteworthy that the whole device can work continuously for more than 8 h under the support of a 20,000 mAh mobile power supply, suggesting the low energy consumption.
Although LAMP is resilient to small shifts in temperature, it is has been well-documented that LAMP amplification cannot be successfully realized at 60 °C [25]. Therefore, the accurate control of temperature still plays a crucial role in ensuring the successful LAMP amplification. More importantly, using the smartphone-based portable device, the temperature of the heating plate could also be fixed in the range of 36.9–37.7 °C (Figure S9a), 40.9–41.7 °C (Figure S9b), and 59.7–60.6 °C (Figure S9c). These results suggested that the reported smartphone-based portable device could also be used for other isothermal amplifications such as RPA, NASBA, and EXPAR, because their favorite amplification temperatures are 37 °C, 41 °C, and 60 °C, respectively.
The second main function of the device is to excite and thereafter collect the detection signals generated by LAMP reaction. Following our previous design [21], in order to guarantee the uniform excitation of the fluorophores on chips, two parallel excitation light beams are designed to avoid the possible systematic error caused by the excitation light. Since this study intends to develop a universal device which can excite most of extensively used fluorescent dyes, two UV lamps are selected as the excitation light source (Fig. 2a), although biomatters always display strong background UV absorption and fluorescence. In addition, the interference of ambient light and the possible specular reflection are substantially reduced by spraying the inner and outer surface of the device with black paint (Fig. 2b). The peripheral accessories can be fabricated with a cost of approximately $120 per set, and its total weight is ~ 300 g, validating its cost-effectiveness and portability.
To provide the end-user a stand-alone device, an open-source and user-friendly Android App, Color Picker, is used to extract the RGB values from fluorescence images of the paper-based biochips. As shown in Figure S10, only two function buttons are used in this APP: “select a picture” and “select a specific area”. For a typical analysis procedure, the button of “select a picture” is pressed to select a picture for data analysis. Then, press the button of “select a specific area” to select the area of interest from the picture, and its RGB value will immediately appear at the bottom of the screen.
Analytical performance
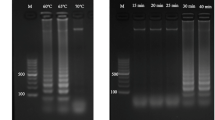
Firstly, the smartphone-based portable device integrated with the paper-based isothermal amplification chip was evaluated its sensitivity at first using the gDNA of Salmonella spp. Figure 3a and b demonstrated the detection of LAMP amplicons after a 30-min reaction inside the chambers of the biochip and heated at 65 °C by the portable device. Obvious green fluorescence (from chamber 3 to chamber 6 of Fig. 3a) and gel bands (from lane 3 to lane 6 of Fig. 3b) can only be observed when the concentration of gDNA reaches to 2.8 × 10−5 ng μL−1, suggesting the LOD for Salmonella spp. using the reported method is 2.8 × 10−5 ng μL−1. Compared with previously reported on-chip LAMP protocols, the reported method exhibited a comparable sensitivity (Table 1) [25, 39,40,41,42,43,44,45], and non-negligible advantages of ease-of-use and cost-effectiveness. Correlated well with LAMP reaction performed inside tube, LAMP reaction performed on chip still exhibits good specificity. As shown in Fig. 3c and d, only LAMP amplicons of Salmonella spp. can only be detected in the presence of Salmonella spp. primers (chamber 1 of Fig. 3c and lane 1 of Fig. 3d).
Sensitivity and specificity results of Salmonella spp. detection using the smartphone-based portable device integrated with the paper-based bi
ochip. a, b Sensitivity experiment. In chambers 1–6, the added gDNA is in increasing concentrations from 2.8 × 10−7 ng μL−1 up to 2.8 × 10−2 ng μL−.1. Chamber N is set as the negative control where no gDNA is added. c, d Specificity experiment. In chambers 1–3, the pre-loaded primers are designed for Salmonella spp., E. coli O157:H7, and S. aureus, respectively. Chamber N is set as the negative control where no primer is added. Photographs showing the reaction and detection zones of the paper-based biochips (a, c) and agarose gel electrophoresis result (b, d)
The reactivity of LAMP reagent pre-loaded onto the paper-based isothermal amplification chip using trehalose is also evaluated. Correlating well with previous reports [13], after being stored inside trehalose for 40 days, the pre-loaded LAMP reagents can still be successfully used for the amplification of target pathogenic gDNA, suggesting excellent long-term storage stability of the paper-based biochip (Figure S11). In addition, 7 pieces of biochips pre-loaded with LAMP reagents for the detection of E. coli O157:H7 were stored at 4 °C refrigerator and used to evaluate their reactivity over time using smartphone-based portable device. Results confirmed that target pathogenic DNA can be successfully amplified (Figure S12b) and E. coli O157:H7 can still be successfully detected using smartphone-based portable device integrated with the biochips (Figure S12a), after being stored at 4 °C refrigerator for 7 days.
The smartphone-based portable device integrated with the paper-based isothermal amplification chip is demonstrated for multiplexed detection of E. coli O157:H7, Salmonella spp., and S. aureus. To validate the practicality of the reported method, eight different samples were prepared as follows: three samples contain only one kind of target pathogenic gDNA, three samples contain any two kinds of target pathogenic gDNA, one sample contains no target pathogenic gDNA, and one sample contain all three kinds of target pathogenic gDNA. Due to the high specificity of the established LAMP protocols (Figure S4), no non-specific response was observed (Fig. 4), validating the excellent anti-interference capability of the reported chip and portable device for practical applications.
Spiked sample analysis
The reported method is also used to determine S. aureus in spiked milk samples to demonstrate its feasibility for actual applications. To this end, different amount of S. aureus were spiked into liquid milk to prepare a series of contaminated milk samples (0, 100, 101, 102, 103, 104 CFU mL−1). After DNA extraction, the obtained gDNA were determined using the reported method and real-time PCR in parallel. As shown in Figure S13 and Table 2, the reported method could identify spiked sample with concentration ≥ 10 CFU mL−1. Since pathogenic bacteria are not allowed in food at most countries and regions, the sensitivity of the reported method should be further improved, for example, by integration with pre-enrichment culture of bacteria. Although the real-time PCR method exhibited higher sensitivity, the reported method highlights its advantages of rapid and ease-of-use detection in a cost-effective manner. Remarkably, starting from gDNA extraction, the whole process of on-site detection of E. coli O157:H7, Salmonella spp., and S. aureus can be completed within 4 h (including 3.0–3.5 h for gDNA extraction, 30 min for LAMP reaction, and ~ 1 min for data analysis). Notably, in this study, the simultaneous detection of three pathogens can be realized at ~ $9.0 per assay without the use of any expensive equipment except for a smartphone.
Conclusion
In conclusion, this study presents a cost-effective, ease-of-use, and portable sensing system which is composed of a smartphone-based portable device and a paper-based isothermal amplification chip. The LAMP reagents have been pre-loaded onto the paper-based isothermal amplification chips, ensuring portability and long-term storage of the amplification reagents. The smartphone-based portable device can provide accurate temperature control for isothermal amplification and precisely collect fluorescent signals generated by amplification reaction for point-of-care nucleic acid detections. This study develops a universal platform for sensing any nucleic acid markers which can be amplified using LAMP technique. Through only changing the primers used in the LAMP protocol, the reported biochips can be used to detect any other pathogens. The reported sensing system has been successfully demonstrated for on-site detection of E. coli O157:H7, Salmonella spp., and S. aureus, highlighting its potential as an appropriate screening method for genetic diagnostics anywhere, anytime, and by anyone.
References
Pereiro I, Bendali A, Tabnaoui S, Alexandre L, Srbova J, Bilkova Z, Deegan S, Joshi L, Viovy JL, Malaquin L, Dupuy B, Descroix S (2017) A new microfluidic approach for the one-step capture, amplification and label-free quantification of bacteria from raw samples. Chem Sci 8(2):1329 1336
World Health Organization, Food safety (2020). https://www.who.int/news-room/fact-sheets/detail/food-safety. Accessed 15 Feb 2022
World Health Organization, Foodborne diseases (2020). https://www.who.int/health-topics/foodborne-diseases. Accessed 15 Feb 2022
Trinh TND, Lee NY (2019) A foldable isothermal amplification microdevice for fuchsin-based colorimetric detection of multiple foodborne pathogens. Lab Chip 19(8):1397-1405
Trinh TND, La HC, Lee NY (2019) Fully integrated and foldable microdevice encapsulated with agarose for long-term storage potential for point-of-care testing of multiplex foodborne pathogens. Acs Sensors 4(10):2754-2762
Zhang H, Zhang YL, Lin YK, Liang TW, Chen ZH, Li JF, Yue ZF, Lv JZ, Jiang Q, Yi CQ (2015) Ultrasensitive detection and rapid identification of multiple foodborne pathogens with the naked eyes. Biosens Bioelectron 71:186-193
Zhang H, Shi YP, Lan F, Pan Y, Lin YK, Lv JZ, Zhu ZH, Jiang Q, Yi CQ (2014) Detection of single-digit foodborne pathogens with the naked eye using carbon nanotube-based multiple cycle signal amplification. Chem Commun 50(15):1848-1850
Gupta R, Raza N, Bhardwaj SK, Vikrant K, Kim KH, Bhardwaj N (2021) Advances in nanomaterial-based electrochemical biosensors for the detection of microbial toxins, pathogenic bacteria in food matrices. J Hazard Mater 401:123379
Jagadeesan B, Gerner-Smidt P, Allard MW, Leuillet S, Winkler A, Xiao YH, Chaffron S, Van der Vossen J, Tang SL, Katase M, McClure P, Kimura B, Chai LC, Chapman J, Grant K (2019) The use of next generation sequencing for improving food safety: Translation into practice. Food Microbiol 79:96-115
Dietrich R, Jessberger N, Ehling-Schulz M, Martlbauer E, Granum PE (2021) The Food Poisoning Toxins of Bacillus cereus. Toxins 13(2):98
Hu YX, Lu XN (2020) Rapid pomegranate juice authentication using a simple sample-to-answer hybrid paper/polymer-based lab-on-a-chip device. Acs Sensors 5(7):2168-2176
Trinh KTL, Trinh TND, Lee NY (2019) Fully integrated and slidable paper-embedded plastic microdevice for point-of-care testing of multiple foodborne pathogens. Biosens Bioelectron 135:120-128
Kaur N, Michael JS, Toley BJ (2019) A modular paper-and-plastic device for tuberculosis nucleic acid amplification testing in limited-resource settings. Sci Rep-Uk 9:15367
Nguyen HQ, Bui HK, Phan VM, Seo TS (2022) An internet of things-based point-of-care device for direct reverse-transcription-loop mediated isothermal amplification to identify SARS-CoV-2. Biosens Bioelectron 195:113655
Berger J, Aydin MY, Stavins R, Heredia J, Mostafa A, Ganguli A, Valera E, Bashir R, King WP (2021) Portable pathogen diagnostics using microfluidic cartridges made from continuous liquid interface production additive manufacturing. Anal Chem 93(29):10048-10055
Ali MM, Li F, Zhang ZQ, Zhang KX, Kang DK, Ankrum JA, Le XC, Zhao WA (2014) Rolling circle amplification: a versatile tool for chemical biology, materials science and medicine. Chem Soc Rev 43(10):3324-3341
Piepenburg O, Williams CH, Stemple DL, Armes NA (2006) DNA detection using recombination proteins. Plos Biol 4(7):1115-1121
Vincent M, Xu Y, Kong HM (2004) Helicase-dependent isothermal DNA amplification. Embo Rep 5(8):795-800
Yan L, Zhou J, Zheng Y, Gamson AS, Roembke BT, Nakayama S, Sintim HO (2014) Isothermal amplified detection of DNA and RNA. Mol Biosyst 10(5):970-1003
Walker GT, Fraiser MS, Schram JL, Little MC, Nadeau JG, Malinowski DP (1992) Strand displacement amplification--an isothermal, in vitro DNA amplification technique. Nucleic Acids Res 20(7):1691-1696
Yue SZ, Li YW, Qiao ZJ, Song WL, Bi S (2021) Rolling circle replication for biosensing, bioimaging, and biomedicine. Trends Biotechnol 39(11):1160-1172
Bi S, Yue SZ, Zhang SS (2017) Hybridization chain reaction: a versatile molecular tool for biosensing, bioimaging, and biomedicine. Chem Soc Rev 46(14):4281-4298
Yue SZ, Song XY, Song WL, Bi S (2019) An enzyme-free molecular catalytic device: dynamically self-assembled DNA dendrimers for in situ imaging of microRNAs in live cells. Chem Sci 10(6):1651-1658
Xiao M, Liu ZG, Xu NX, Jiang LL, Yang MS, Yi CQ (2020) A smartphone-based sensing system for on-site quantitation of multiple heavy metal ions using fluorescent carbon nanodots-based microarrays. Acs Sensors 5(3):870-878
Trinh TND, Lee NY (2018) A rapid and eco-friendly isothermal amplification microdevice for multiplex detection of foodborne pathogens. Lab Chip 18(16):2369-2377
Trieu PT, Lee NY (2019) Paper-based all-in-one origami microdevice for nucleic acid amplification testing for rapid colorimetric identification of live cells for point-of-care testing. Anal Chem 91(17):11013-11022
Zhang DM, Liu QJ (2016) Biosensors and bioelectronics on smartphone for portable biochemical detection. Biosens Bioelectron 75:273-284
Xu ZZ, Liu ZJ, Xiao M, Jiang LL, Yi CQ (2020) A smartphone-based quantitative point-of-care testing (POCT) system for simultaneous detection of multiple heavy metal ions. Chem Eng J 394:124966
Liu ZG, Zhang YL, Xu SJ, Zhang H, Tan YX, Ma CM, Song R, Jiang LL, Yi CQ (2017) A 3D printed smartphone optosensing platform for point-of-need food safety inspection. Anal Chim Acta 966:81-89
Li L, Liu ZG, Zhang H, Yue WQ, Li CW, Yi CQ (2018) A point-of-need enzyme linked aptamer assay for Mycobacterium tuberculosis detection using a smartphone. Sensor Actuat B-Chem 254:337-346
Xiao M, Zhou Q, Zhang H, Zhou L, Ma J, Yi C (2021) Logic gate design using multicolor fluorescent carbon nanodots for smartphone-based information extraction. ACS Applied Nano Materials 4(8):8184-8191
Liu JJ, Geng ZX, Fan ZY, Liu J, Chen HD (2019) Point-of-care testing based on smartphone: The current state-of-the-art (2017-2018). Biosens Bioelectron 132:17-37
Chan HN, Tan MJA, Wu HK (2017) Point-of-care testing: applications of 3D printing. Lab Chip 17(16):2713-2739
Zhang QQ, Chen ZT, Shi ZH, Li YR, An ZJ, Li X, Shan JZ, Lu YL, Liu QJ (2021) Smartphone-based photoelectrochemical biosensing system with graphitic carbon nitride/gold nanoparticles modified electrodes for matrix metalloproteinase-2 detection. Biosens Bioelectron 193:113572
Low SS, Pan YX, Ji DZ, Li YR, Lu YL, He Y, Chen QM, Liu QJ (2020) Smartphone-based portable electrochemical biosensing system for detection of circulating microRNA-21 in saliva as a proof-ofconcept. Sensor Actuat B-Chem 308:127718
Fischbach J, Xander NC, Frohme M, Glokler JF (2015) Shining a light on LAMP assays-a comparison of LAMP visualization methods including the novel use of berberine. Biotechniques 58(4):189-194
Wang H, Ma Z, Qin JX, Shen Z, Liu Q, Chen XY, Wang HL, An ZH, Liu W, Li M (2019) A versatile loop-mediated isothermal amplification microchip platform for Streptococcus pneumoniae and Mycoplasma pneumoniae testing at the point of care. Biosens Bioelectron 126:373-380
Lopez-Ruiz N, Curto VF, Erenas MM, Benito-Lopez F, Diamond D, Palma AJ, Capitan-Vallvey LF (2014) Smartphone-based simultaneous pH and nitrite colorimetric determination for paper microfluidic devices. Anal Chem 86(19):9554-9562
Zhang MM, Liu JF, Shen ZQ, Liu YX, Song Y, Liang Y, Li ZD, Nie LM, Fang YJ, Zhao YQ (2021) A newly developed paper embedded microchip based on LAMP for rapid multiple detections of foodborne pathogens. Bmc Microbiol 21(1):197
Nguyen HA, Lee NY (2021) Polydopamine aggregation: A novel strategy for power-free readout of loop-mediated isothermal amplification integrated into a paper device for multiplex pathogens detection. Biosens Bioelectron 189:113353
Uddin SM, Ibrahim F, Sayad AA, Thiha A, Pei KX, Mohktar MS, Hashim U, Cho J, Thong KL (2015) A portable automatic endpoint detection system for amplicons of loop mediated isothermal amplification on microfluidic compact disk platform. Sensors-Basel 15(3):5376-5389
Santiago-Felipe S, Tortajada-Genaro LA, Carrascosa J, Puchades R, Maquieira A (2016) Real-time loop-mediated isothermal DNA amplification in compact disc micro-reactors. Biosens Bioelectron 79:300-306
Sayad A, Ibrahim F, Uddin SM, Cho J, Madou M, Thong KL (2018) A microdevice for rapid, monoplex and colorimetric detection of foodborne pathogens using a centrifugal microfluidic platform. Biosens Bioelectron 100:96-104
Wang CH, Lien KY, Wu JJ, Lee GB (2011) A magnetic bead-based assay for the rapid detection of methicillin-resistant Staphylococcus aureus by using a microfluidic system with integrated loop-mediated isothermal amplification. Lab Chip 11(8):1521-1531
Kim J-H, Yoo IS, An JH, Kim S (2018) A novel paper-plastic hybrid device for the simultaneous loop-mediated isothermal amplification and detection of DNA. Materials Letters 214:243-246
Funding
This work was supported by the National Key Research and Development Program of China (2022YFE0201800), Shenzhen-Hong Kong-Macao Science and Technology Plan Project (SGDX2020110309260000), Guangdong Natural Science Foundation (2021A1515220020), and Shenzhen Science and Technology Innovation Commission (JCYJ20210324140004013 and GJHZ20210705142200001).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file2 (MP4 12563 KB)
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhou, Q., Pan, J., Mo, L. et al. Fluorescent on-site detection of multiple pathogens using smartphone-based portable device with paper-based isothermal amplification chip. Microchim Acta 189, 333 (2022). https://doi.org/10.1007/s00604-022-05419-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00604-022-05419-x