Abstract
Purpose
The efficiency and safety of routine intravenous administration of acetaminophen after highly invasive hepatobiliary pancreatic surgery remain unclear. In particular, there have been no studies focusing on pancreatoduodenectomy. The present study clarified its clinical utility for patients undergoing pancreatoduodenectomy.
Methods
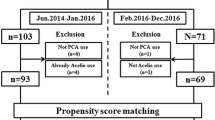
We retrospectively collected 179 patients who underwent open pancreatoduodenectomy from 2015 to 2020. The analgesic effects and adverse events in patients with scheduled intravenous administration of acetaminophen were evaluated using propensity score matching.
Results
After 40 patients from each group were selected by propensity score matching, the postoperative liver function tests were not significantly different between the control and acetaminophen groups. No significant differences were found in the self-reported pain intensity score or postoperative nausea and vomiting; however, the rate of pentazocine use and the total number of additional analgesics were significantly lower in the acetaminophen group than in the control group (p = 0.003 and 0.002, respectively).
Conclusion
The scheduled intravenous administration of acetaminophen did not affect the postoperative liver function and had a good analgesic effect after pancreatoduodenectomy.



Similar content being viewed by others
Data availability
No data was used for the research described in the article.
References
Melloul E, Lassen K, Roulin D, Grass F, Perinel J, Adham M, et al. Guidelines for perioperative care for pancreatoduodenectomy: enhanced recovery after surgery (ERAS) recommendations 2019. World J Surg. 2020;44:2056–84.
Beverly A, Kaye AD, Ljungqvist O, Urman RD. Essential elements of multimodal analgesia in enhanced recovery after surgery (ERAS) guidelines. Anesthesiol Clin. 2017;35:e115–43.
Macario A, Royal MA. A literature review of randomized clinical trials of intravenous acetaminophen (paracetamol) for acute postoperative pain. Pain Pract. 2011;11:290–6.
Ohkura Y, Haruta S, Shindoh J, Tanaka T, Ueno M, Udagawa H. Effectiveness of postoperative intravenous acetaminophen (Acelio) after gastrectomy: a propensity score-matched analysis. Medicine. 2016;95(44): e5352.
Hidaka M, Ohyama K, Hara T, Soyama A, Adachi T, Kamada N, et al. The feasibility and safety in using acetaminophen with fentanyl for pain control after liver resection with regards to liver function: a prospective single-center pilot study in Japan. J Hepatobiliary Pancreat Sci. 2021;28:297–303.
Choi M, Hwang HK, Rho SY, Lee WJ, Kang CM. Comparing laparoscopic and open pancreaticoduodenectomy in patients with pancreatic head cancer: oncologic outcomes and inflammatory scores. J Hepatobiliary Pancreat Sci. 2020;27:124–31.
Chun LJ, Tong MJ, Busuttil RW, Hiatt JR. Acetaminophen hepatotoxicity and acute liver failure. J Clin Gastroenterol. 2009;43:342–9.
Fujii T, Nakao A, Yamada S, Suenaga M, Hattori M, Takami H, et al. Vein resections >3 cm during pancreatectomy are associated with poor 1-year patency rates. Surgery. 2015;157:708–15.
Nishijima M, Baba H, Murotani K, Tokai R, Watanabe T, Hirano K, et al. Early ambulation after general and digestive surgery: a retrospective single-center study. Langenbecks Arch Surg. 2020;405:613–22.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, et al. International study group on pancreatic surgery (ISGPS). the 2016 update of the International study group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery. 2017;161:584–91.
Owens WD, Felts JA, Spitznagel EL Jr. ASA physical status classifications: a study of consistency of ratings. Anesthesiology. 1978;49:239–43.
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, et al. Toxicity and response criteria of the Eastern cooperative oncology group. Am J Clin Oncol. 1982;5:649–55.
Werawatganon T, Charuluxanun S. Patient controlled intravenous opioid analgesia versus continuous epidural analgesia for pain after intra-abdominal surgery. Cochrane Database Syst Rev. 2005. https://doi.org/10.1002/14651858.CD004088.pub2.
Salicath JH, Yeoh EC, Bennett MH. Epidural analgesia versus patient-controlled intravenous analgesia for pain following intra-abdominal surgery in adults. Cochrane Database Syst Rev. 2018;8:010434.
Fotiadis RJ, Badvie S, Weston MD, Allen-Mersh TG. Epidural analgesia in gastrointestinal surgery. Br J Surg. 2004;91:828–41.
Moraca RJ, Sheldon DG, Thirlby RC. The role of epidural anesthesia and analgesia in surgical practice. Ann Surg. 2003;238:663–73.
Clemente A, Carli F. The physiological effects of thoracic epidural anesthesia and analgesia on the cardiovascular, respiratory and gastrointestinal systems. Minerva Anestesiol. 2008;74:549–63.
Block BM, Liu SS, Rowlingson AJ, Cowan AR, Cowan JA Jr, Wu CL. Efficacy of postoperative epidural analgesia: a meta-analysis. JAMA. 2003;290:2455–63.
Pratt WB, Steinbrook RA, Maithel SK, Vanounou T, Callery MP, Vollmer CM Jr. Epidural analgesia for pancreatoduodenectomy: a critical appraisal. J Gastrointest Surg. 2008;12:1207–20.
Gan TJ, Diemunsch P, Habib AS, Kovac A, Kranke P, Meyer TA, et al. Society for ambulatory anesthesia consensus guidelines for the management of postoperative nausea and vomiting. Anesth Analg. 2014;118:85–113.
Roberts GW, Bekker TB, Carlsen HH, Moffatt CH, Slattery PJ, McClure AF. Postoperative nausea and vomiting are strongly influenced by postoperative opioid use in a dose-related manner. Anesth Analg. 2005;101:1343–8.
McNicol ED, Ferguson MC, Haroutounian S, Carr DB, Schumann R. Single dose intravenous paracetamol or intravenous propacetamol for postoperative pain. Cochrane Database Syst Rev. 2016. https://doi.org/10.1002/14651858.CD007126.pub3.
Yamagata Y, Yoshikawa T, Yura M, Otsuki S, Morita S, Katai H, et al. Current status of the “enhanced recovery after surgery” program in gastric cancer surgery. Ann Gastroenterol Surg. 2019;3:231–8.
Hidaka M, Ohyama K, Hara T, Soyama A, Adachi Y, Kamada N, et al. The feasibility and sagety in using acetaminophen with fentanyl for pain control after liver resection with regard to live function: a prospective single-center pilot study in Japan. JHBPS. 2021;28:297–303.
Akashi M, Nagakawa Y, Hosowaka Y, Takishita C, Osakabe H, Nishino H, et al. Preoperative cholangitis is associated with increased surgical site infection following pancreatoduodenectomy. JHBPS. 2020;27:640–7.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335:806–8.
Itoyama R, Okabe H, Yamashita YI, Kitamura F, Uemura N, Nakao Y, et al. Intraoperative bile culture helps choosing antibiotics in pancreaticoduodenectomy: mechanistic profiling study of complex rink between bacterobilia and postoperative complications. J Hepatobiliary Pancreat Sci. 2021;28:1107–14.
Acknowledgements
This research was funded by JSPS KAKENHI, grant number 18H02878. The authors thank American Journal Experts (https://www.aje.com) for editing a draft of this manuscript.
Author information
Authors and Affiliations
Contributions
KH, TI, KM, NT, TM, TW, KS, IY, and TF were involved in the study design. KH, TI, NT, and TS collected the data. KH, TI, NT and KM were involved in the data analysis. KH, TI, KM, NT, TF were involved in the data interpretation. All authors revised the report and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no conflicts of interest related to this article. It is the responsibility of the corresponding author to review this policy with all authors.
Ethical approval
The study was reviewed and approved (Ref. No. R2020200) by the institutional review board and complied with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines [27]. All procedures in this study were performed in accordance with the guidelines of the Declaration of Helsinki. Written informed consent for treatment was obtained from each patient prior to the start of treatment, and consent for the use of data for research was obtained on an opt-out basis.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hirano, K., Igarashi, T., Murotani, K. et al. Efficacy and feasibility of scheduled intravenous acetaminophen administration after pancreatoduodenectomy: a propensity score-matched study. Surg Today 53, 1047–1056 (2023). https://doi.org/10.1007/s00595-023-02647-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-023-02647-3