Abstract
Purpose
We investigated the preoperative assessment of coronary artery calcification using computed tomography for appropriate intraoperative management to reduce the risk of perioperative cardiac complications during pulmonary resection.
Methods
Patients (n = 665) who underwent anatomical lung resection were examined. The extent of preoperative asymptomatic coronary artery stenosis or cardiac complications in patients with coronary artery calcification was assessed. In addition, the risk factors for perioperative cardiac complications were determined.
Results
Coronary artery calcification was detected in 233 (35.0%) asymptomatic patients. Nineteen (8.2%) patients with coronary artery calcification had coronary artery stenosis ≥ 75%. Percutaneous coronary intervention was performed preoperatively (n = 3) and postoperatively (n = 10), and preoperative drug intervention was performed in 10 cases. One case of severe postoperative cardiac complications and 20 cases of mild postoperative cardiac complications, including those without coronary artery calcification, occurred. Patients with calcified coronary arteries were at risk of cardiovascular complications in the perioperative period. However, patients with coronary artery calcification who underwent preoperative cardiology intervention had no significant perioperative cardiovascular complications.
Conclusions
Coronary artery calcification detected on preoperative computed tomography is a risk factor for perioperative cardiovascular complications. Early intervention may reduce the risk of such complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recently, the number of patients with asymptomatic ischemic heart disease has increased with the increasing number of older adults eligible for surgery. A 2009 study by the Japanese Association of Thoracic Surgery showed that ischemic cardiac diseases occurred in 1350 of 31,301 patients who underwent thoracic surgery in Japan. Furthermore, ischemic heart diseases were identified as the second-most common risk factor for preoperative comorbidity in patients who underwent resection of primary lung cancer caused by smoking [1]. In addition, a 2015 study by the Japanese Association of Thoracic Surgery stated that cardiovascular diseases were the cause of 21 (6.6%) of 318 hospital deaths among 40,302 patients who underwent pulmonary resection for lung cancer [2].
The results of the ISCHEMIA clinical trial showed that there was no significant difference in the incidence of adverse events, such as ischemic cardiovascular events or death from any cause, over a median of 3.2 years between patients that received invasive and conservative treatment for stable coronary disease and moderate or severe ischemia [3]. Therefore, with appropriate intervention, stable ischemia may be managed non-invasively. In contrast, pulmonary resection may affect tt hemodynamics and induce cardiac disease.
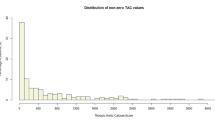
Given the above, we hypothesized that perioperative mortality and morbidity could be reduced if we could detect and start treating asymptomatic ischemic heart disease in the preoperative period. Tt evaluation of coronary artery stenosis using coronary artery computed tomography (CT) or coronary angiography (CAG) is just an indication and cannot be applied in all patients undergoing surgery. Interventionalists recently attempted to evaluate the risk of asymptomatic coronary disease by evaluating coronary artery calcification (CAC) using chest CT [4]. The CAC score is calculated as the area and weight of the CAC multiplied by the score on CT images with a 3-mm slice thickness. This score indicates the level of accumulating arteriosclerosis non-invasively, which was reported to increase with the incidence of heart accidents in asymptomatic patients [4]. In a pooled analysis, an increasing CAC score demonstrated a higher perioperative risk, with a CAC score ≥ 1000 conferring the highest risk in non-cardiac surgery cases [5].
As chest CT is essential prior to thoracic surgery, we investigated the clinical significance of preoperatively assessing CAC using plain chest CT and considered appropriate perioperative and intraoperative risk-aversive approaches to manage patients with indications for thoracic surgery.
Methods
Study design
This study was approved by the Research Review Board of the National Hospital Organization Nagasaki Medical Center in accordance with the Declaration of Helsinki (approval no.: 2020135, approved on January 4, 2021). Written informed consent for the publication of this report and use of the accompanying images was obtained from all the patients.
Between April 2010 and March 2020, a total of 770 patients underwent anatomical pulmonary resection at our hospital. Extended surgeries, such as combined resection of adjacent organs, bi-lobectomy, and pneumonectomy, were not included in this study. Among the total patients, 105 who had been treated by a cardiologist or presented circulatory symptoms at the time of the first medical examination were introduced to a cardiologist before surgery as usual. The remaining 665 patients who had neither symptoms nor a history of cardiac disease without hypertension underwent resting electrocardiography before surgery. CAC was defined as high-concentration changes in the coronary arteries, ranging from spot-like to segmental changes, judged to be calcifications on plain chest CT with the mediastinal window. The presence or absence of calcification was determined by the attending physician. Patients in whom CAC was detected using plain chest CT underwent echocardiography and exercise stress electrocardiography along with resting electrocardiography. Among these patients, those who had significant echocardiography or exercise stress electrocardiography findings had consultations with a cardiologist and underwent close examinations. Patients who had significant findings on close inspections by a cardiologist started undergoing treatments preoperatively (Fig. 1).
Analyses of separated patients
First, the data of patients who had already undergone cardiovascular intervention and those who had some cardiovascular symptoms at the first visit (105 patients) were analyzed separately.
Analyses of patients with CAC detected using plain chest CT
Second, the participants, excluding those who had already undergone cardiovascular intervention and those who had some cardiovascular symptoms at the first visit (665 patients), were divided into 2 groups according to previously detected CAC using plain chest CT: the calcification (+) (233 patients) and calcification (−) (432 patients) groups. Subsequently, their age, sex, and medical history (hypertension, diabetes mellitus, hyperlipidemia, smoking, and antithrombotic therapy for ischemic diseases, such as cerebral infarction but excepting ischemic heart disease) were compared, and the presence of risk factors for CAC was examined.
Echocardiography and exercise stress electrocardiography
Third, the 233 patients with CAC underwent echocardiography and exercise stress electrocardiography. Among them, 95 patients with significant findings were referred to a cardiologist and underwent close examinations, if required, as judged by the cardiologist. Among the 95 patients, 63 had abnormalities on echocardiography and exercise stress electrocardiography and 32 were unable to undergo exercise stress electrocardiography because of lower-limb paralysis caused by cerebrovascular disorders or lower-limb muscle weakness were considered to have significant findings and were referred to a cardiologist for consultation.
Perioperative treatment and risk factors for perioperative cardiovascular complications
Finally, all patients (665 patients) with or without CAC were divided into 2 groups: those with cardiovascular complications during the perioperative period (21 patients) and those without such complications (644 patients). The age, sex, and medical history (hypertension, diabetes mellitus, hyperlipidemia, smoking, and antithrombotic therapy), as well as CAC detected on plain chest CT were compared between the two groups, and risk factors for perioperative cardiovascular complications were investigated. In addition, perioperative treatment for patients with significant coronary stenosis was investigated.
Statistical analyses
Continuous variables are presented as the median value with 25th and 75th percentiles. Categorical data are presented as the percentage of patient numbers. We used the Mann–Whitney U test to compare the non-normally distributed continuous variables and the chi-square or Fisher’s exact test to compare the proportions of categorical variables between the two groups. To determine risk factors for CAC and cardiovascular accidents, a multivariate analysis was performed using multiple logistic regression. Continuous variables (age) were dichotomized with respect to the median value in the multivariate analysis. A p value < 0.05 was considered statistically significant. The JMP software program, version 15 (SAS Institute Inc., Cary, NC, USA), was used to perform all statistical analyses.
Results
Characteristics of the excluded patients
In total, 105 patients had been treated by a cardiologist previously (85 cases) or had circulatory symptoms at the time of the first medical examination (20 cases) (Table 1). Concerning the type of disease treated by the cardiologist (ischemic heart diseases, arrhythmia, and other various cases), 38 (44.7%) patients were treated for ischemic heart diseases. Among those who had a history or symptoms of heart disease, 79 (75.2%) patients had CAC. Of the patients with a history of ischemic heart disease, 34 (89.5%) had CAC. Among these patients, new or additional treatments were initiated preoperatively in 11 patients.
Characteristics of patients with CAC detected on plain chest CT
In this study, 432 patients did not have calcified coronary arteries on plain chest CT, and they underwent pulmonary resection with only electrocardiography at rest without close inspection before surgery. In contrast, 233 patients had calcified coronary arteries on plain chest CT, and they underwent echocardiography and exercise stress electrocardiography before surgery. The patient characteristics are presented in Table 2. The calcification (+) group had a higher number of older patients (≥ 75 years); male patients; and patients with hypertension, diabetes mellitus, anticoagulant use, and a history of smoking than the calcification (−) group in the univariate analysis (Table 3). In the multivariate analysis, study factors, except for sex, diabetes mellitus, hyperlypidemia, and smokers, were significantly higher in the calcification (+) than in the calcification (−) group (Table 3).
Echocardiography and exercise stress electrocardiography
In this study, 138 of the 233 patients with CAC had no significant echocardiography or exercise stress electrocardiography findings, and they underwent pulmonary resection without close inspection before surgery. The remaining 95 patients, including 63 who had significant echocardiography findings (pericardial fluid, 2 patients; local hypokinesis, 9 patients) or exercise stress electrocardiography findings (pseudo-positive findings, 7 patients; ST change, 35 patients; ventricular premature contraction, 6 patients; abnormal Q wave, 2 patients; symptoms, 4 patients) (there was some overlap), or 32 patients with non-cardiac vascular disease who were unable to exercise as a result of lower-limb paralysis due to cerebrovascular disease or lower-limb muscle weakness associated with an impaired lower limb blood flow, thus suggesting the presence of asymptomatic ischemic heart disease. These patients were referred to a cardiologist who performed a closer examination, if required, before surgery.
Treatment by a cardiologist in the perioperative period
In total, 95 patients were referred to a cardiologist. Of them, 29 did not require close inspection, 7 underwent myocardial scintigraphy, 48 underwent coronary CT angiography, and 22 underwent CAG (there was some overlap). Nineteen (20.0%) of the 95 patients showed significant stenosis of the coronary arteries (≥ 75%), accounting for 8.2% of all 233 patients with CAC. The sites of CAC and the actual coronary artery stenosis were the same in 14 patients; however, in a few patients, stenosis was observed in sites without calcification (patients 1 and 2 had complete mismatch; patients 9, 15, and 17 had some mismatch; Table 4).
In total, 13 of 19 patients (68.4%) with significant stenosis of the coronary arteries underwent preoperative treatment by cardiologists; 10 patients started taking medications, whereas 3 underwent percutaneous coronary intervention (PCI). One patient underwent plain old balloon angioplasty (POBA), one received drug-eluting stents (DESs), and one received both POBA and DESs. In addition, among those without significant coronary artery stenosis, six patients initiated new drug therapy, according to their symptoms.
In the intraoperative period, four patients received vasodilators to avoid coronary occlusions. The median time from cardiovascular intervention to surgery was 27.5 (4–56) days, and the patients with DESs underwent surgery 51 and 56 days later with simultaneous anticoagulant therapy in the perioperative period. In the postoperative period, observation was continued in 5 patients (1 patient was followed up with CAG), 3 patients continued taking medication only, and 10 underwent PCI (Table 4).
Perioperative cardiovascular complications
Among the 665 patients with or without CAC, 1 patient (0.15%) had Grade IIIa cardiovascular complications based on the Clavien–Dindo classification (Grade IIIa atrial fibrillation [AF] requiring ablation). Twenty patients (3.0%) had mild cardiovascular complications below Grade II based on the Clavien–Dindo classification (Table 5). Overall, 57.1% of patients who developed perioperative complications had CAC, whereas 66.7% of patients who developed AF had CAC (Table 5). Patients with CAC were significantly more likely to develop postoperative AF than those without CAC (p = 0.02). No coronary accidents were recorded, and no perioperative cardiovascular complications were observed in the 25 patients in whom preoperative therapeutic intervention was performed or coronary artery stenosis was identified before surgery.
The 665 patients were divided into the cardiovascular complication (+) group (21 patients) and the cardiovascular complication (−) group (644 patients). The patient characteristics according to the two groups are presented in Table 6. In the univariate analysis, the cardiovascular complication (+) group had a higher proportion of calcified coronary arteries on plain CT than those in the cardiovascular complication (−) group (Table 7). In the multivariate analysis, the proportion of patients who showed a higher tendency to have calcified coronary arteries detected on plain CT was significantly higher in the cardiovascular complication (+) group than in the cardiovascular complication (−) group (Table 7).
Discussion
In this study, we revealed that patients with CAC detected on plain chest CT have many risk factors for cardiovascular disease and have a high risk of perioperative cardiac complications despite having no symptoms in the preoperative period. However, asymptomatic patients with significant stenosis of the coronary arteries who underwent appropriate preoperative intervention had no perioperative complications. Selective scrutiny of patients with CAC using preoperative plain chest CT and appropriate preoperative intervention may reduce the risk of perioperative cardiac complications.
The United States (US) Preventive Task Force suggests that the current evidence regarding CAC is insufficient to weigh the benefits and risks of adding it to traditional risk assessment measures for heart attack and stroke prevention in people without symptoms because of the lack of access to original data [6]. In addition, a review of CAC in lung cancer screening suggests that CAC is a less accurate test for cardiovascular risk than extra-coronary thoracic arterial calcifications (ECC) and that the measurement of ECC may be a better indicator of cardiovascular risk [7]. However, compared with ECC, CAC is more strongly associated with coronary heart disease [7], and the presence of CAC on plain chest CT may be a predictor of a high risk of chronic coronary artery stenosis [8]. Our study also showed that patients with a history of ischemic heart disease had a higher rate of CAC than those without such a history.
In addition, CAC is independently associated with an increased risk of AF [9], and even patients without coronary artery disease (CAD) have an increased risk of stroke and death if they have AF and incidental CAC detected on chest CT [10]. Although arrhythmias, including AF, are common complications after pulmonary resection, it is important to know preoperatively which asymptomatic patients are at an increased risk of developing a cardiac disease. According to our study, patients with asymptomatic CAC had a significantly higher tendency to have many of the risk factors for coronary artery stenosis presented by the US Preventive Services Task Force [6] than those without asymptomatic CAC. In addition, only CAC was identified as a risk factor for perioperative complications, while among the patients who developed perioperative complications, those with AF were likely to have CAC. Even when the risk factors appear to be controlled, each risk accumulated over time may be reflected in CAC. Thus, CAC may be the most reliable factor to consider when evaluating patients referred for surgical treatment at tertiary medical institutions.
In addition, in this study, CAC was not scored, but all cases of CAC, from spot calcifications to segmental calcifications, were included. Although all cases with significant coronary artery stenosis detected at CAG had segmental CAC in this study, in some cases, the site of CAC did not match the actual site of coronary artery stenosis. In studies using coronary arteriography, intracoronary ultrasonography, and autopsy findings, the CAC scores were correlated well with atherosclerotic plaque burden; however, there was no association with the luminal cross-sectional area. The presence of calcification detected by chest CT does not imply significant coronary stenoses [11]. However, to identify cases with a high risk of cardiovascular complications, scrutinizing patients with CAC detected on plain chest CT is important.
The sensitivity and specificity of exercise stress electrocardiography when searching for coronary artery stenosis are approximately 70% and 75%, respectively [12,13,14]. In addition, in the present study, patients with lower-limb movement disorders due to medical issues, such as arthropathy, arteriosclerosis obliterans, and cerebrovascular disorders, who did not undergo exercise stress electrocardiography were considered as high-risk patients and selected for a close examination by cardiologists. In fact, 5 of the 32 patients who could not undergo stress electrocardiography had significant stenosis in the coronary arteries. In contrast, resting echocardiography is useful for patients with chronic CAD, especially for those with hypertension or valvular disease [15, 16]. Cardiac expansion or a decreased cardiac function detected on resting echocardiography in cases of chronic CAD is associated with the prognosis [17, 18].
Patients with CAD in pulmonary surgery are more likely to have perioperative complications, including coronary vascular events than patients without CAD, although this does not affect long-term outcomes after pulmonary resection [19]. Furthermore, in the LIFE-Heart Study, coronary atherosclerosis (CAS) without CAD (stenosis of the coronary arteries < 75%) was associated with an increased risk of AF [20]. In the present study, perioperative complications did not occur in patients with CAC in whom preoperative scrutiny was performed and led to appropriate therapeutic intervention. Identification and therapeutic intervention in patients with CAC who had asymptomatic CAD or CAS may have reduced perioperative complications.
Rather than scoring CAC, screening patients with CAC by echocardiography and exercise stress electrocardiography and using the results to perform a cardiological examination even if the patient is asymptomatic would allow us to intervene preoperatively in patients with cardiovascular risk, even without access to special equipment to quantify and score CAC. This could potentially reduce perioperative complications.
In patients with a DES, dual antiplatelet therapy for more than one year is recommended [21, 22], and its discontinuation for non-cardiac surgery prior to this time point is associated with an increased risk of major adverse cardiac events [23, 24]. However, surgery in the presence of dual antiplatelet therapy may increase the risk of perioperative bleeding and its associated complications [25, 26]. Therefore, surgery for lung disease must be delayed for an extended period. In our department, after consultation with a cardiologist, balloon dilatation and drug treatment are generally initiated before surgery with consideration of the degree of pulmonary lesion progression, degree of stenosis of the coronary artery, and site of stenosis; preoperative coronary stenting is performed only in patients with severe coronary artery stenosis. Patients who underwent preoperative stenting received surgery while maintaining anticoagulation in the perioperative period. High-risk patients who did not undergo preoperative stenting received surgery under intraoperative coronary vasodilation after consultation with the anesthesiologist. The DES was then implanted when patients had stabilized after surgery. For the maintenance of anesthesia, it was useful for the anesthesiologist to be aware of the presence of coronary stenosis. Perioperative coronary complications did not occur in this study. By preoperatively identifying patients with significant coronary artery stenosis, it may be possible to prevent cardiovascular complications through appropriate preoperative and perioperative management, including intraoperative anesthesia management, even in patients with risk factors for cardiovascular complications.
Limitations
Several limitations associated with the present study warrant mention. In this study, no instances of serious perioperative coronary complications were observed. However, we did not perform perioperative troponin T measurement or postoperative electrocardiography retesting, which might have concealed potential coronary complications in the perioperative period. It is also possible that patients with potential asymptomatic CAD were present in the CAC (−) group, as a close examination was not performed in this group. In addition, our study’s results deviated from those previously proposed by the US Preventive Task Force, where the current evidence regarding CAC was insufficient to weigh the benefits and risks of adding it to traditional risk assessment measures for heart attack and stroke prevention in asymptomatic patients. Considering the difference in findings between the present and previous studies, it is reasonable to assume that this cohort exhibits a selection bias, possibly because of the involvement of tertiary medical institutions, surgical referrals, and the single-center setting. Patients who might have been deemed unfit for surgery because of the presence of risk factors, such as elderly persons, hypertension, diabetes, antithrombotic therapy, or smoker, might have already been excluded. However, CAC was confirmed as a clear risk factor in the present study. Future studies should include patients with CAC without scrutiny or those without CAC with scrutiny who underwent lung surgery. However, based on the present findings, we believe that not performing a thorough examination on patients with CAC may be ethically problematic and requires careful consideration.
In conclusion, patients with CAC are more likely to have cardiac risk factors than those without CAC. CAC is a risk factor for perioperative cardiac complications, and the selective evaluation of and intervention for patients with CAC using preoperative chest CT may reduce the risk of perioperative cardiac complications.
References
Committee for Scientific Affairs, Sakata R, Fujii Y, Kuwano H. Thoracic and cardiovascular surgery in Japan during 2009: annual report by the Japanese Association for Thoracic Surgery. Gen Thorac Cardiovasc Surg. 2011;59:636–67. https://doi.org/10.1007/s11748-011-0838-5.
Committee for Scientific Affairs, The Japanese Association for Thoracic Surgery, Masuda M, Endo S, Natsugoe S, Shimizu H, Doki Y, et al. Thoracic and cardiovascular surgery in Japan during 2015: annual report by the Japanese Association for Thoracic Surgery. Gen Thorac Cardiovasc Surg. 2018;66:581–615. https://doi.org/10.1007/s11748-018-0968-0.
Maron DJ, Hochman JS, Reynolds HR, Bangalore S, O’Brien SM, Boden WE, et al. Initial invasive or conservative strategy for stable coronary disease. N Engl J Med. 2020;382:1395–407. https://doi.org/10.1056/NEJMoa1915922.
Greenland P, Bonow RO, Brundage BH, Budoff MJ, Eisenberg MJ, Grundy SM, et al. ACCF/AHA 2007 clinical expert consensus document on coronary artery calcium scoring by computed tomography in global cardiovascular risk assessment and in evaluation of patients with chest pain: a report of the American College of Cardiology Foundation Clinical Expert Consensus Task Force (ACCF/AHA Writing Committee to Update the 2000 Expert Consensus Document on Electron Beam Computed Tomography). J Am Coll Cardiol. 2007;115:402–26.
Koshy AN, Ha FJ, Gow PJ, Han HC, Amirul-Islam FM, Lim HS, et al. Computed tomographic coronary angiography in risk stratification prior to non-cardiac surgery: a systematic review and meta-analysis. Heart. 2019;105:1335–42. https://doi.org/10.1136/heartjnl-2018-314649.
Helfand M, Buckley DI, Freeman M, Fu R, Rogers K, Fleming C, et al. Emerging risk factors for coronary heart disease: a summary of systematic reviews conducted for the US Preventive Services Task Force. Ann Intern Med. 2009;151:496–507. https://doi.org/10.7326/0003-4819-151-7-200910060-00010.
Dirrichs T, Penzkofer T, Reinartz SD, Kraus T, Mahnken AH, Kuhl CK. Extracoronary thoracic and coronary artery calcifications on chest CT for lung cancer screening: association with established cardiovascular risk factors - the “CT-Risk” trial. Acad Radiol. 2015;22:880–9. https://doi.org/10.1016/j.acra.2015.03.005.
Bittner V, Bertolet M, Barraza Felix RB, Farkouh ME, Goldberg S, Ramanathan KB, et al. Comprehensive cardiovascular risk factor control improves survival: the BARI 2D trial. J Am Coll Cardiol. 2015;66:765–73. https://doi.org/10.1016/j.jacc.2015.06.019.
Oneal WT, Efird J, Dawood FZ, Yoboah J, Alonso A, Heckbert SR, et al. Coronary artery calcium and risk of atrial fibrillation (from the multi-ethnic study of atherosclerosis). Am J Cardiol. 2014;114:1707–12. https://doi.org/10.1016/j.amjcard.2014.09.005.
Hillerson D, Wool T, Ogunbayo GO, Sorrell V, Leung SW. Incidental coronary artery calcification and stroke risk in patients with atrial fibrillation. AJR Am J Roentgenol. 2020;215:344–50. https://doi.org/10.2214/AJR.19.22298.
Greenland P, Blaha MJ, Budoff MJ, Erbel R, Watson KE. Coronary calcium score and cardiovascular risk. J Am Coll Cardiol. 2018;72:434–47. https://doi.org/10.1016/j.jacc.2018.05.027.
Gibbons RJ, Balady GJ, Beasley JW, Bricker JT, Duvernoy WF, Froelicher VF, et al. ACC/AHA Guidelines for Exercise Testing. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines Committee on Exercise Testing. J Am Coll Cardiol. 1997;30:260–311. https://doi.org/10.1016/s0735-1097(97)00150-2.
Gianrossi R, Detrano R, Mulvihill D, Lehmann K, Dubach P, Colombo A, et al. Exercise-induced ST depression in the diagnosis of coronary artery disease. A meta-analysis. Circulation. 1989;80:87–98. https://doi.org/10.1161/01.cir.80.1.87.
Pearson TA. New tools for coronary risk assessment: what are their advantages and limitations? Circulation. 2002;105:886–92. https://doi.org/10.1161/hc0702.103727.
Yamashina A, Ueshima K, Kimura K, Kuribayashi Y, Sakuma H, Tamaki N, et al. Guidelines for noninvasive diagnosis of coronary artery lesions (JCS 2009). Circ J. 2009;73:1019–114.
Ogawa S, Fujii I, Yoshino H, Tani M, Ohnishi S, Nagata M, et al. Values of electrocardiography and two-dimensional echocardiography to identify myocardial infarction due to left circumflex and right coronary artery disease. Clin Cardiol. 1985;8:269–75. https://doi.org/10.1002/clc.4960080506.
Daly C, Norrie J, Murdoch DL, Ford I, Dargie HJ, Fox K, et al. The value of routine non-invasive tests to predict clinical outcome in stable angina. Eur Heart J. 2003;24:532–40. https://doi.org/10.1016/s0195-668x(02)00820-5.
Daly CA, De Stavola B, Sendon JLL, Tavazzi L, Boersma E, Clemens F, et al. Predicting prognosis in stable angina–results from the euro heart survey of stable angina: prospective observational study. BMJ. 2006;332:262–7. https://doi.org/10.1136/bmj.38695.605440.AE.
Kanzaki R, Inoue M, Minami M, Shintani Y, Funaki S, Kawamura T, et al. Outcomes of lung cancer surgery in patients with coronary artery disease: a decade of experience at a single institution. Surg Today. 2017;47:27–34. https://doi.org/10.1007/s00595-016-1355-z.
Kornej J, Henger S, See Seewöster T, Teran A, Burkhardt R, Thiele H, et al. Prevalence of atrial fibrillation dependent on coronary artery status: Insights from the LIFE-Heart Study. Clin Cardiol. 2020;43:1616–23. https://doi.org/10.1002/clc.23490.
Serruys PW, Daemen J. Are drug-eluting stents associated with a higher rate of late thrombosis than bare metal stents? Late stent thrombosis: a nuisance in both bare metal and drug-eluting stents. Circulation. 2007;115:1433–9. https://doi.org/10.1161/CIRCULATIONAHA.106.666826 (discussion 1439).
Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, et al. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation. 2011;124:e574-651. https://doi.org/10.1161/CIR.0b013e31823ba622.
Eisenberg MJ, Richard PR, Libersan D, Filion KB. Safety of short-term discontinuation of antiplatelet therapy in patients with drug-eluting stents. Circulation. 2009;119:1634–42. https://doi.org/10.1161/CIRCULATIONAHA.108.813667.
McFadden EP, Stabile E, Regar E, Cheneau E, Ong ATL, Kinnaird T, et al. Late thrombosis in drug-eluting coronary stents after discontinuation of antiplatelet therapy. Lancet. 2004;364:1519–21. https://doi.org/10.1016/S0140-6736(04)17275-9.
Leon MB, Baim DS, Popma JJ, Gordon PC, Cutlip DE, Ho KK, et al. A clinical trial comparing three antithrombotic-drug regimens after coronary-artery stenting. Stent Anticoagulation restenosis Study Investigators. N Engl J Med. 1998;339:1665–71. https://doi.org/10.1056/NEJM199812033392303.
Kunadian B, Thornley AR, Tanos M, Dunning J. Should clopidogrel be stopped prior to urgent cardiac surgery? Interact Cardiovasc Thorac Surg. 2006;5:630–6. https://doi.org/10.1510/icvts.2006.140038.
Acknowledgements
This study was supported by an in-hospital clinical research grant at Nagasaki Medical Center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Machino, R., Shimoyama, K., Oku, K. et al. Prevalence of coronary calcification on preoperative computed tomography and its management in thoracic surgery. Surg Today 53, 62–72 (2023). https://doi.org/10.1007/s00595-022-02532-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-022-02532-5