Abstract
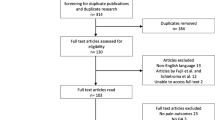
Postoperative pain is the main reason for delayed recovery after herniorrhaphy. Preoperative glucocorticoid administration may improve postoperative recovery. The present study assessed the efficacy of preoperative glucocorticoids in facilitating recovery after herniorrhaphy. Randomized controlled trials (RCTs) conducted up to January 2021 were searched in electronic databases and trial registries. Meta-analyses were performed using random effects models. The Grading of Recommendations, Assessment, Development, and Evaluation approach was used to assess the certainty of evidence. Seven RCTs (744 patients) were included in the meta-analysis. Preoperative glucocorticoid administration reduced patients’ pain on postoperative day 0 (standard mean difference [SMD] = − 0.73, 95% confidence interval [CI] − 1.45 to − 0.01; I2 = 94%). However, there was no marked difference in rescue analgesic use (risk ratio [RR] = − 0.06, 95% CI − 0.28 to − 0.16; I2 = 0%) or vomiting (RR = 0.78, 95% CI 0.50–1.20; I2 = 30%) between preoperative glucocorticoid administration and control. The certainty of evidence was moderate because of inconsistencies or imprecision. No serious adverse effects were observed. Preoperative glucocorticoid administration reduced pain in patients following herniorrhaphy without increasing the occurrence of adverse events. Further studies will be required to confirm the efficacy of preoperative glucocorticoids.



Similar content being viewed by others
Abbreviations
- CI:
-
Confidence interval
- NRS:
-
Numeric rating scale
- PONV:
-
Postoperative nausea and vomiting
- RCT:
-
Randomized controlled trials
- RR:
-
Risk ratio
- SMD:
-
Standard mean difference
- VAS:
-
Visual analog scale
References
HerniaSurge Group. International guidelines for groin hernia management. Hernia. 2018;22:1–165.
Fränneby U, Sandblom G, Nordin P, Nyrén O, Gunnarsson U. Risk factors for long-term pain after hernia surgery. Ann Surg. 2006;244:212–9.
Tolver MA, Rosenberg J, Bisgaard T. Early pain after laparoscopic inguinal hernia repair. A qualitative systematic review. Acta Anaesthesiol Scand. 2012;56:549–57.
Nir RR, Nahman-Averbuch H, Moont R, Sprecher E, Yarnitsky D. Preoperative preemptive drug administration for acute postoperative pain: a systematic review and meta-analysis. Eur J Pain. 2016;20:1025–43.
National Institute for Health and Care Excellence (2016) NICE technology appraisal guidance no. 83: laparoscopic surgery for inguinal hernia repair. https://www.nice.org.uk/guidance/ta83. Accessed 16 May 2021.
Holte K, Kehlet H. Perioperative single-dose glucocorticoids administration: pathophysiologic effects and clinical implications. J Am Coll Surg. 2002;195:694–712.
Corcoran TB, Edwards T. A survey of antiemetic dexamethasone administration-frequency of use and perceptions of benefits and risks. Anaesth Intensive Care. 2015;43:167–74.
Polderman JA, Farhang-Razi V, Van Dieren S, Kranke P, DeVries JH, Hollmann MW, et al. Adverse side effects of dexamethasone in surgical patients. Cochrane Database Syst Rev. 2018;8:CD011940.
Chen CC, Siddiqui FJ, Chen TL, Chan ES, Tam KW. Dexamethasone for prevention of postoperative nausea and vomiting in patients undergoing thyroidectomy: meta-analysis of randomized controlled trials. World J Surg. 2012;36:61–8.
Yang Q, Zhang Z, Xin W, Li A. Preoperative intravenous glucocorticoids can decrease acute pain and postoperative nausea and vomiting after total hip arthroplasty: a PRISMA-compliant meta-analysis. Medicine (Baltimore). 2017;96:e8804.
Tolska HK, Hamunen K, Takala A, Kontinen VK. Systematic review of analgesics and dexamethasone for post-tonsillectomy pain in adults. Br J Anaesth. 2019;123:e397–411.
Wu H, Wang H, Liu Y, Wu Z. Can preoperative intravenous corticosteroids administration reduce postoperative pain scores following spinal fusion?: A meta-analysis. J Invest Surg. 2020;33:307–16.
Jacobs A, Lemoine A, Joshi GP, Van de Velde M, Bonnet F, PROSPECT Working Group collaborators. PROSPECT guideline for oncological breast surgery: a systematic review and procedure-specific postoperative pain management recommendations. Anaesthesia. 2020;75:664–73.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Sokratous A, Österberg J, Sandblom G. The impact of groin surgery during childhood on the incidence of inguinal hernia repair and its postoperative complications in adult life. Eur J Pediatr Surg. 2019;29:271–5.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;2019:l4898.
Higgins JPT, Thomas J. Cochrane Handbook for Systematic Reviews of Interventions Version 6. 2. 2021. Available online: https://training.cochrane.org/handbook/current Accessed 16 May 2021.
Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64:383–94.
Shafa A. A comparative study on the efficacy of intravenous dexamethasone and lidocaine in reducing respiratory complications after general anesthesia in children with a history of reactive airways. Iranian Registry of Clinical Trials. 2018. https://www.irct.ir/trial/32002. Accessed 16 May 2021.
Srinivasan B, Karnawat R, Mohammed S, Chaudhary B, Ratnawat A, Kothari SK. Comparison of caudal and intravenous dexamethasone as adjuvants for caudal epidural block: a double blinded randomised controlled trial. Indian J Anaesth. 2016;60:948–54.
Ghazi A. Effect of intravenous dexamethasone on prevention of complications of laryngeal mask airway (LMA) in inguinal region surgeries. Iranian Registry of Clinical Trials. 2020. https://www.irct.ir/trial/50074. Accessed 16 May, 2021.
Kavyannejad R. A comparative study of dexamethasone and metoclopramide in prevention of post nausea and vomiting after hernia inguinal surgery. Iranian Registry of Clinical Trials. 2020. https://www.irct.ir/trial/4807. Accessed 16 May 2021.
Gupta D, Agrawal M. Comparative study of preoperative oral pregabalin alone, pregabalin with dexamethasone and pregabalin with vitamin B complex for postoperative analgesic requirement in open inguinal hernia repair under subarachanoids block. CTRI. 2018. http://www.ctri.nic.in/Clinicaltrials/pmaindet2.php?trialid=24371. Accessed 16 May 2021.
Tan PH, Liu K, Peng CH, Yang LC, Lin CR, Lu CY. The effect of dexamethasone on postoperative pain and emesis after intrathecal neostigmine. Anesth Analg. 2001;92:228–32.
Galinski SF, Pereira JA, Maestre Y, Francés S, Escolano F, Puig MM. The combination of intravenous dexamethasone and ketamine does not improve postoperative analgesia when compared to each drug individually. The Pain Clinic. 2007;19:223–9.
Movafegh A, Soroush AR, Navi A, Sadeghi M, Esfehani F, Akbarian-Tefaghi N. The effect of intravenous administration of dexamethasone on postoperative pain, nausea, and vomiting after intrathecal injection of meperidine. Anesth Analg. 2007;104:987–9.
Tolver MA, Strandfelt P, Bryld EB, Rosenberg J, Bisgaard T. Randomized clinical trial of dexamethasone versus placebo in laparoscopic inguinal hernia repair. Br J Surg. 2012;99:1374–80.
Simsa J, Magnusson N, Hedberg M, Lorentz T, Gunnarsson U, Sandblom G. Betamethasone in hernia surgery: a randomized controlled trial. Eur J Pain. 2013;17:1511–6.
Asad MV, Khan FA. Effect of a single bolus of dexamethasone on intraoperative and postoperative pain in unilateral inguinal hernia surgery. J Anaesthesiol Clin Pharmacol. 2015;31:339–43.
Jensen KK, Brøndum TL, Leerhøy B, Belhage B, Hensler M, Arnesen RB, et al. Preoperative, single, high-dose glucocorticoids administration in abdominal wall reconstruction: a randomized, double-blinded clinical trial. Surgery. 2020;167:757–64.
Thammasitboon S, Thammasitboon S. A critical appraisal of a systematic review: Sokol J, Jacob SE, Bohn D: Inhaled nitric oxide for acute hypoxemic respiratory failure in children and adults. Cochrane Database Syst Rev. 2003;6:CD002787.
Cohen J. Statistical power analysis for the behavioral sciences. New Jersey: L. Hillsdale, Erlbaum Associates; 1988.
Monteiro B, Steagall PV. Antiinflammatory drugs. Vet Clin North Am Small Anim Pract. 2019;49:993–1011.
Karcioglu O, Topacoglu H, Dikme O, Dikme O. A systematic review of the pain scales in adults: Which to use? Am J Emerg Med. 2018;36:707–14.
Farrar JT, Young JP Jr, LaMoreaux L, Werth JL, Poole MR. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94:149–58.
Sansonnens J, Taffé P, Burnand B. ADS study group Higher occurrence of nausea and vomiting after total hip arthroplasty using general versus spinal anesthesia: an observational study. BMC Anesthesiol. 2016;16:44.
Jensen KK. Recovery after abdominal wall reconstruction. Dan Med J. 2017;64:B5349.
Acknowledgements
We thank Dr. Toshihide Izumida and Ms. Chisato Fujiwara for providing us with the CENTRAL and ICTRP search data, respectively.
Funding
This research received no external funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
595_2021_2431_MOESM1_ESM.docx
Supplementary Supplementary 1: The electronic database search strategy. Supplementary 2: The trial registry search strategy. Supplementary 3: Risk of bias for the eligible studies (DOCX 22 KB)
595_2021_2431_MOESM2_ESM.pptx
Supplementary Supplementary Fig. 1: Forest plot of patients’ pain on postoperative day 0. A) Hernia types (inguinal vs. ventral incisional hernia), B) surgical approach (laparoscopy vs. open), and C) steroid types (dexamethasone vs. betamethasone vs. methylprednisolone). Supplementary Fig. 2: Forest plot of patients’ pain on postoperative day 1. A) Hernia types (inguinal vs. ventral incisional hernia), B) surgical approach (laparoscopy vs. open), and C) steroid types (dexamethasone vs. betamethasone vs. methylprednisolone) (PPTX 312 KB)
Rights and permissions
About this article
Cite this article
Watanabe, J., Rifu, K., Kagaya, T. et al. The efficacy and safety of preoperative glucocorticoids in herniorrhaphy: a systematic review and meta-analysis. Surg Today 52, 1237–1245 (2022). https://doi.org/10.1007/s00595-021-02431-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-021-02431-1