Abstract
Purpose
To evaluate the long-term efficacy of large gastric pouch surgery and revisional surgery in patients with a body mass index (BMI) < 35 kg/m2 and type 2 diabetes mellitus (T2DM).
Methods
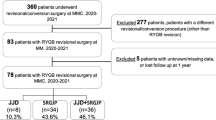
We conducted a retrospective review of patients who underwent laparoscopic Roux-en-Y gastrojejunostomy with a large gastric pouch in our hospital. The clinical pre- and post-surgery data, including BMI, waist circumference, fasting plasma glucose (FPG), glycated hemoglobin (HbA1c), lipid metabolism-related indicators, homoeostatic model assessment of insulin resistance (HOMA-IR), and major complications, were recorded and analyzed.
Results
Twenty-four patients were included in the analysis, 12 of whom underwent revisional surgery. At their 5-year-follow-up after the primary surgery, the BMI and waist circumference of the patients with T2DM were lower than their baseline values. The BMI, HbA1c, HOMA-IR, FPG and waist circumference also decreased after the revisional surgery. The rates of remission of diabetes after the primary vs. after the revisional surgery were 4.17% vs. 41.70%, respectively (P < 0.05).
Conclusion
Roux-en-Y gastrojejunostomy with a large gastric pouch is not effective in the long term and, therefore, is unsuitable for Chinese patients with T2DM and a BMI < 35 kg/m2. Conversely, revisional surgery has a definite effect on these patients.
Similar content being viewed by others
References
Yang WY, Lu JM, Weng JP, Jia WP, Ji LN, Xiao JZ, et al. Prevalence of diabetes among men and women in China. New Engl J Med. 2010;362(12):1090–101.
Xu Y, Wang L, He J, Bi Y, Li M, Wang T, et al. Prevalence and control of diabetes in Chinese adults. JAMA. 2013;310(9):948–59.
Bommer C, Heesemann E, Sagalova V, Manne-Goehler J, Atun R, Barnighausen T, et al. The global economic burden of diabetes in adults aged 20–79 years: a cost-of-illness study. Lancet Diabetes Endocrinol. 2017;5(6):423–30.
Avogaro A, Fadini GP. Microvascular complications in diabetes: a growing concern for cardiologists. Int J Cardiol. 2019;291:29–35.
Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2011. Obes Surg. 2013;23(4):427–36.
Baker MT. The history and evolution of bariatric surgical procedures. Surg Clin North Am. 2011;91(6):1181–201.
Consultation WE. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. The Lancet. 2004;363(9403):157–63.
Dixon JB, Zimmet P, Alberti KG, Rubino F. Bariatric surgery: an IDF statement for obese Type 2 diabetes. Diabet Med. 2011;28(6):628–42.
Kasama K, Mui W, Lee WJ, Lakdawala M, Naitoh T, Seki Y, et al. IFSO-APC consensus statements 2011. Obes Surg. 2012;22(5):677–84.
Chang CJ, Wu CH, Chang CS, Yao WJ, Yang YC, Wu JS, et al. Low body mass index but high percent body fat in Taiwanese subjects: implications of obesity cutoffs. Int J Obes. 2003;27(2):253–9.
Yi B, Jiang J, Zhu L, Li P, Im I, Zhu S. Comparison of the effects of Roux-en-Y gastrojejunostomy and LRYGB with small stomach pouch on type 2 diabetes mellitus in patients with BMI<35 kg/m(2). Surg Obes Relat Dis. 2015;11(5):1061–8.
Elshaer M, Hamaoui K, Rezai P, Ahmed K, Mothojakan N, Al-Taan O. Secondary bariatric procedures in a high-volume centre: prevalence, indications and outcomes. Obes Surg. 2019;29(7):2255–62.
Lee WJ, Hur KY, Lakadawala M, Kasama K, Wong SK, Chen SC, et al. Predicting success of metabolic surgery: age, body mass index, C-peptide, and duration score. Surg Obes Relat Dis. 2013;9(3):379–84.
Aminian A, Brethauer SA, Andalib A, Nowacki AS, Jimenez A, Corcelles R, et al. Individualized metabolic surgery score: procedure selection based on diabetes severity. Ann Surg. 2017;266(4):650–7.
Matsuda M, DeFronzo RA. Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp. Diabetes Care. 1999;22(9):1462–70.
Patel P, Abate N. Body fat distribution and insulin resistance. Nutrients. 2013;5(6):2019–27.
Naslund I, Wickbom G, Christoffersson E, Agren G. A prospective randomized comparison of gastric bypass and gastroplasty Complications and early results. Acta Chir Scand. 1986;152:681–9.
Naslund I. Gastric bypass versus gastroplasty. A prospective study of differences in two surgical procedures for morbid obesity. Acta Chir Scand Suppl. 1987;536:1–60.
Pareek M, Schauer PR, Kaplan LM, Leiter LA, Rubino F, Bhatt DL. Metabolic surgery: weight loss, diabetes, and beyond. J Am Coll Cardiol. 2018;71(6):670–87.
Drucker DJ. Mechanisms of action and therapeutic application of glucagon-like peptide-1. Cell Metab. 2018;27(4):740–56.
Goh YM, Toumi Z, Date RS. Surgical cure for type 2 diabetes by foregut or hindgut operations: a myth or reality? A systematic review. Surg Endosc. 2017;31(1):25–37.
Cummings DE, Arterburn DE, Westbrook EO, Kuzma JN, Stewart SD, Chan CP, et al. Gastric bypass surgery vs intensive lifestyle and medical intervention for type 2 diabetes: the CROSSROADS randomised controlled trial. Diabetologia. 2016;59(5):945–53.
Chen JC, Hsu NY, Lee WJ, Chen SC, Ser KH, Lee YC. Prediction of type 2 diabetes remission after metabolic surgery: a comparison of the individualized metabolic surgery score and the ABCD score. Surg Obes Relat Dis. 2018;14(5):640–5.
Dolo PR, Shao Y, Li C, Zhu X, Yao L, Wang H. The effect of gastric bypass with a distal gastric pouch on glucose tolerance and diabetes remission in type 2 diabetes Sprague-Dawley rat model. Obes Surg. 2019;29(6):1889–900.
Riccioppo D, Santo MA, Rocha M, Buchpiguel CA, Diniz MA, Pajecki D, et al. Small-volume, fast-emptying gastric pouch leads to better long-term weight loss and food tolerance after Roux-en-Y gastric bypass. Obes Surg. 2018;28(3):693–701.
Mullally JA, Febres GJ, Bessler M, Korner J. Sleeve gastrectomy and Roux-en-Y gastric bypass achieve similar early improvements in beta-cell function in obese patients with type 2 diabetes. Sci Rep. 2019;9(1):1880.
Ciovica R, Takata M, Vittinghoff E, Lin F, Posselt AM, Rabl C, et al. The impact of Roux limb length on weight loss after gastric bypass. Obes Surg. 2008;18(1):5–10.
Orci L, Chilcott M, Huber O. Short versus long roux-limb length in Roux-en-Y gastric bypass surgery for the treatment of morbid and super obesity: a systematic review of the literature. Obes Surg. 2011;21(6):797–804.
Evers SS, Sandoval DA, Seeley RJ. The physiology and molecular underpinnings of the effects of bariatric surgery on obesity and diabetes. Annu Rev Physiol. 2017;10(79):313–34.
Radtka JF 3rd, Puleo FJ, Wang L, Cooney RN. Revisional bariatric surgery: who, what, where, and when? Surg Obes Relat Dis. 2010;6(6):635–42.
Kassir R, Blanc P, Lointier P, Tiffet O, Breton C, Ben Amor I, et al. An analysis of surgical anatomy of the gastric fundus in bariatric surgery: why the gastric pouch expands? A point of technique. Int J Surg. 2014;12(11):1151–6.
Coblijn UK, Goucham AB, Lagarde SM, Kuiken SD, van Wagensveld BA. Development of ulcer disease after Roux-en-Y gastric bypass, incidence, risk factors, and patient presentation: a systematic review. Obes Surg. 2014;24(2):299–309.
Sverden E, Mattsson F, Sonden A, Leinskold T, Tao W, Lu Y, et al. Risk factors for marginal ulcer after gastric bypass surgery for obesity: a population-based cohort study. Ann Surg. 2016;263(4):733–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gao, X., Zhu, L., Li, W. et al. Revisional large gastric pouch with Roux-en-Y gastric bypass for patients with type 2 diabetes and a body mass index less than 35 kg/m2: a cause and effect analysis. Surg Today 52, 287–293 (2022). https://doi.org/10.1007/s00595-021-02317-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-021-02317-2