Abstract
Aims
Glargine 300 U/mL (Gla-300) has been recently approved for use in children and adolescents with type 1 diabetes (T1D). However, real-world effectiveness data are scarce, and aim of this analysis was to assess clinical outcomes in young patients with T1D switching from 1st generation basal insulin (1BI) to Gla-300.
Methods
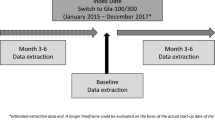
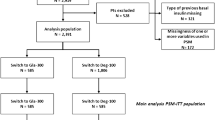
ISPED CARD is a retrospective, multicenter study, based on data anonymously extracted from Electronic Medical Records. The study involved a network of 20 pediatric diabetes centers. Data on all patients aged < 18 years with T1D switching from 1BI to Gla-300 were analyzed to assess clinical characteristics at the switch and changes after 6 and 12 months in glycated hemoglobin (HbA1c), fasting blood glucose (FBG), and standardized body mass index (BMI/SDS). Titration of basal and short-acting insulin doses was also evaluated.
Results
Overall, 200 patients were identified. The mean age at the switch to Gla-300 was 13 years, and mean duration of diabetes was 3.9 years. Average HbA1c levels at switch were 8.8%. After 6 months, HbA1c levels decreased by − 0.88% (95% CI − 1.28; − 0.48; p < 0.0001). The benefit was maintained after 12 months from the switch (mean reduction of HbA1c levels − 0.80%, 95% CI − 1.25; − 0.35, p = 0.0006). Trends of reduction in FBG levels were also evidenced both at 6 months and 12 months. No significant changes in short-acting and basal insulin doses were documented.
Conclusions
The study provides the first real-world evidence of the effectiveness of Gla-300 in children and adolescents with T1D previously treated with 1BI. The benefits in terms of HbA1c levels reduction were substantial, and sustained after 12 months. Additional benefits can be expected by improving the titration of insulin doses.


Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request. Qualified researchers may request access to patient-level data and related documents (including, e.g., the clinical study report, study protocol with any amendments, blank case report form, statistical analysis plan, and dataset specifications). Patient-level data will be anonymized, and study documents will be redacted to protect the privacy of trial participants.
Abbreviations
- 95% CI:
-
95% Confidence interval
- ATC:
-
Anatomical therapeutic chemical codes
- 1BI:
-
First generation basal insulin
- 2BI:
-
Second-generation basal insulins
- BI:
-
Basal insulin
- BMI:
-
Body mass index
- BMI/SDS:
-
Standardized BMI
- CSII:
-
Continuous subcutaneous insulin infusion (Insulin Pump)
- CGM:
-
Continuous glucose monitoring
- Deg-100:
-
Degludec 100 U/mL
- EMR:
-
Electronic medical records
- FBG:
-
Fasting blood glucose
- Gla-300:
-
Glargine 300 U/mL
- GP:
-
General practitioner
- HbA1c:
-
Glycated hemoglobin
- ISPED CARD:
-
Italian society of paediatric endocrinology diabetology continuous clinical monitoring of diabetes
- LDL:
-
Low-density lipoproteins
- MDI:
-
Multiple daily injections of insulin
- NPH:
-
Neutral protamine hagedorn insulin
- OR:
-
Odds Ratio
- PDOC:
-
Pediatric diabetes outpatient clinics
- RWE:
-
Real-world evidence
- SIEDP:
-
Italian society of pediatric endocrinology and diabetology
- T1D:
-
Type 1 diabetes
- T2D:
-
Type 2 diabetes
- T0:
-
Baseline
- T6:
-
Follow-up at 6 months
- T12:
-
Follow-up at 12 months
- QoL:
-
Quality of life
References
de Bock M, Codner E, Craig ME et al (2022) ISPAD Clinical Practice Consensus Guidelines 2022: glycemic targets and glucose monitoring for children, adolescents, and young people with diabetes. Pediatr Diabetes 23:1270–1276. https://doi.org/10.1111/pedi.13455
Cengiz E, Danne T, Ahmad T et al (2022) ISPAD clinical practice consensus guidelines 2022: insulin treatment in children and adolescents with diabetes. Pediatr Diabetes 23:1277–1296. https://doi.org/10.1111/pedi.13442
Limbert C, Tinti D, Malik F et al (2022) ISPAD clinical practice consensus guidelines 2022: the delivery of ambulatory diabetes care to children and adolescents with diabetes. Pediatr Diabetes 23:1243–1269. https://doi.org/10.1111/pedi.13417
Anderson BJ, Laffel LM, Domenger C et al (2017) Factors associated with diabetes-specific health-related quality of life in youth with type 1 diabetes: the global TEENs study. Diabetes Care 40:1002–1009
Driscoll KA, Raymond J, Naranjo D, Patton SR (2016) Fear of hypoglycemia in children and adolescents and their parents with type 1 diabetes. Curr Diab Rep 16:77
Foster NC, Beck RW, Miller KM et al (2019) State of type 1 diabetes management and outcomes from the T1D exchange in 2016–2018. Diabetes Technol Ther 21:66–72. https://doi.org/10.1089/dia.2018.0384
Witsch M, Kosteria I, Kordonouri O et al (2016) Possibilities and challenges of a large international benchmarking in pediatric diabetology-The SWEET experience. Pediatr Diabetes 17(Suppl 23):7–15. https://doi.org/10.1111/pedi.12432
Van Loocke M, Battelino T, Tittel SR et al (2021) Lower HbA1c targets are associated with better metabolic control. Eur J Pediatr 180:1513–1520. https://doi.org/10.1007/s00431-020-03891-2
Bailey TS, Pettus J, Roussel R et al (2018) Morning administration of 0.4U/kg/day insulin glargine 300U/mL provides less fluctuating 24-hour pharmacodynamics and more even pharmacokinetic profiles compared with insulin degludec 100 U/mL in type 1 diabetes. Diabetes Metab 44:15–21
Heise T, Hovelmann U, Nosek L, Hermanski L, Bottcher SG, Haahr H (2015) Comparison of the pharmacokinetic and pharmacodynamic profiles of insulin degludec and insulin glargine. Expert Opin Drug Metab Toxicol 11:1193–1201
Tumini S, Carinci S (2017) Unmet needs in children with diabetes: the role of basal insulin. Minerva Pediatr 69:513–530. https://doi.org/10.23736/S0026-4946.17.05112-X
Roussel R, Ritzel R, Boëlle-Le Corfec E, Balkau B, Rosenstock J (2018) Clinical perspectives from the BEGIN and EDITION programmes Trial-level meta-analyses outcomes with either degludec or glargine 300U/mL vs glargine 100U/mL in T2DM. Diabetes Metab 44:402–409
Danne T, Tamborlane WV, Malievsky OA et al (2020) Efficacy and safety of insulin glargine 300 Units/mL (Gla-300) versus insulin glargine 100 Units/mL (Gla-100) in children and adolescents (6–17 years) with type 1 diabetes: results of the EDITION JUNIOR randomized controlled trial. Diabetes Care 43:1512–1519
Urakami T, Mine Y, Aoki M, Okuno M, Suzuki J (2017) A randomized crossover study of the efficacy and safety of switching from insulin glargine to insulin degludec in children with type 1 diabetes. Endocr J 64:133–140
Maffeis C, Rabbone I (2022) Insulin glargine 300 U/mL therapy in children and adolescents with type 1 diabetes. Paediatr Drugs 24:499–512
Berger ML, Sox H, Willke RJ et al (2017) Good practices for real-world data studies of treatment and/or comparative effectiveness: recommendations from the joint ISPOR-ISPE special task force on real-world evidence in health care decision making. Value Health 20:1003–1008. https://doi.org/10.1016/j.jval.2017.08.3019
Thalange N, Deeb L, Iotova V et al (2015) Insulin degludec in combination with bolus insulin aspart is safe and effective in children and adolescents with type 1 diabetes. Pediatr Diabetes 16:164–176. https://doi.org/10.1111/pedi.12263
Predieri B, Suprani T, Maltoni G et al (2018) Switching from glargine to degludec: the effect on metabolic control and safety during 1-year of real clinical practice in children and adolescents with type 1 diabetes. Front Endocrinol (Lausanne) 9:462. https://doi.org/10.3389/fendo.2018.00462
Kochar IS, Sethi A (2018) Real-world efficacy and safety of insulin degludec with mealtime rapid-acting insulin in type 1 diabetes in Indian pediatric population. Int J Pediatr Endocrinol 2018:6. https://doi.org/10.1186/s13633-018-0059-0
Urakami T, Kuwabara R, Aoki M, Okuno M, Suzuki J (2016) Efficacy and safety of switching from insulin glargine to insulin degludec in young people with type 1 diabetes. Endocr J 63:159–167. https://doi.org/10.1507/endocrj.EJ15-0245
Schmitt J, Scott ML (2019) Insulin degludec in adolescents with Type 1 diabetes: Is newer better? - A retrospective self-control case series in adolescents with a history of diabetic ketoacidosis. Horm Res Paediatr 92:179–185. https://doi.org/10.1159/000504707
Elahi S, Patel AD, Guandalini C et al (2019) Impact of switching youth with diabetes to insulin degludec in clinical practice. Endocr Pract 25:226–229. https://doi.org/10.4158/EP-2018-0417
Rabbone I, Pozzi E, Savastio S et al (2022) A comparison of the effectiveness and safety of insulin glargine 300 U/ml versus 100 U/ml in children and adolescents with newly diagnosed type 1 diabetes: a retrospective, observational, short-term study. Diabetes Obes Metab 24:2474–2477. https://doi.org/10.1111/dom.14839
Laviola L, Porcellati F, Bruttomesso D et al (2021) Comparative effectiveness of switching from first-generation basal insulin to glargine 300 U/ml or degludec 100 U/ml in Type 1 diabetes: the RESTORE-1 study. Diabetes Ther 12:509–525. https://doi.org/10.1007/s13300-020-00982-z
Conget I, Mangas MÁ, Morales C et al (2021) Effectiveness and safety of insulin glargine 300 U/ml in comparison with insulin degludec 100 U/ml evaluated with continuous glucose monitoring in adults with type 1 diabetes and suboptimal glycemic control in routine clinical practice: the OneCARE study. Diabetes Ther 12:2993–3009. https://doi.org/10.1007/s13300-021-01153-4
Nicolucci A, Graziano G, Lombardo F et al (2024) ISPED CARD Study Group Continuous improvement of quality of care in pediatric diabetes: the ISPED CARD clinical registry. Acta Diabetol 61:599–607. https://doi.org/10.1007/s00592-023-02233-6
Rossi MC, Nicolucci A, Arcangeli A et al (2008) Baseline quality-of-care data from a quality-improvement program implemented by a network of diabetes outpatient clinics. Diabetes Care 31:2166–2168. https://doi.org/10.2337/dc08-0469
Rossi MC, Candido R, Ceriello A et al (2015) Trends over 8 years in quality of diabetes care: results of the AMD Annals continuous quality improvement initiative. Acta Diabetol 52:557–571. https://doi.org/10.1007/s00592-014-0688-6
Stahl-Pehe A, Kamrath C, Prinz N et al (2022) Prevalence of type 1 and type 2 diabetes in children and adolescents in Germany from 2002 to 2020: A study based on electronic health record data from the DPV registry. J Diabetes 14:840–850. https://doi.org/10.1111/1753-0407.13339
Beck RW, Tamborlane WV, Bergenstal RM et al (2012) The T1D exchange clinic registry. J Clin Endocrinol Metab 97:4383–4389. https://doi.org/10.1210/jc.2012-1561
Joshi SR, Singh G, Marwah A, Mittra S, Suvarna VR, Athalye SN (2023) Comparative clinical efficacy and safety of insulin glargine 300 U/ml (Toujeo) versus insulin glargine 100 U/ml in type 2 diabetes and type 1 diabetes: a systematic literature review and meta-analysis. Diabetes Obes Metab 25:1589–1606. https://doi.org/10.1111/dom.15007
Bratke H, Margeirsdottir HD, Assmus J, Njølstad PR, Skrivarhaug T (2021) Does current diabetes technology improve metabolic control? A cross-sectional study on the use of insulin pumps and continuous glucose monitoring devices in a nationwide pediatric population. Diabetes Ther 12:2571–2583. https://doi.org/10.1007/s13300-021-01127-6
Laffel LM, Kanapka LG, Beck RW et al (2020) Effect of continuous glucose monitoring on glycemic control in adolescents and young adults with type 1 diabetes: a randomized clinical trial. JAMA 323:2388–2396. https://doi.org/10.1001/jama.2020.6940
Acknowledgements
The authors thank the participating centers and all the collaborators from SANOFI, CORESEARCH and METEDA involved in the study. Additional Assistance: CORESEARCH (Pescara, Italy) was the Clinical Research Organization involved in the data management and statistical analysis (Giuseppe Lucisano, Giusi Graziano), medical writing (Maria Chiara Rossi, Antonio Nicolucci) and regulatory activities (Rosalia Di Lallo, Clara Santavenere) of the study. Meteda (San Benedetto, Italy) developed the software for the data extraction.
The ISPED CARD Study Group: Participating centers—year 2022 (in alphabetic order by town):
Bracciolini GP, Alessandria; Cherubini V, Ancona ; Bobbio A, Aosta; Zucchini S, Bologna; Suprani T, Cesena; De Donno V, Cuneo; Lombardo F, Messina; Bonfanti R, Milano; Franzese A, Napoli; Rabbone I, Novara; Graziani V, Ravenna; Zampolli M, San Fermo Della Battaglia (CO); Rutigliano I, San Giovanni Rotondo (FG); de Sanctis L, Torino; Guerraggio LP, Tradate (VA); Franceschi R, Trento; Tornese G, Trieste; Franco F, Udine; Maffeis C, Verona; Arnaldi C, Viterbo.
Funding
Statistical analysis and medical writing assistance was funded by Sanofi S.r.l., Milan, Italy.
Author information
Authors and Affiliations
Consortia
Contributions
All authors made substantial contributions to the conception and design of the work. Riccardo Bonfanti, Fortunato Lombardo, Ivana Rabbone, and Stefano Zucchini contributed to the data collection. Giusi Graziano conducted the statistical analyses. Maria Chiara Rossi and Antonio Nicolucci drafted the article. All authors revised the article critically for important intellectual content. All authors approved the final version to be published. All authors agreed all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Corresponding author
Ethics declarations
Conflict of interest
Maria Chiara Rossi and Antonio Nicolucci have received funding for research from Sanofi, NovoNordisk, Alfasigma, Pikdare, AstraZeneca, Shionogi, SOBI, and Theras. Riccardo Bonfanti has served on advisory board panels for Sanofi, Novonordisk, Lilly, Medtronic, Abbott, Movi and has received speaker’s fees by Novonordisk, Sanofi, Lilly, Movi, Medtronic, Theras and financial support for research by Movi and Lilly. Giusi Graziano has nothing to disclose. Monica Larosa is an employee of Sanofi and may hold shares and/or stock options in the company. Fortunato Lombardo has received consultancy fees from Movi. Stefano Zucchini has served on advisory board panels for Sanofi and Movi. Giacomo Vespasiani is medical consultant of Meteda. Ivana Rabbone has received honoraria for participating in the speaker bureau and consulting fees as a member of Eli Lilly, Menarini, Medtronic, Theras, Novo Nordisk and Sanofi advisory boards.
Ethical approval
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. The study protocol was approved by all local ethics committees of the participating centers.
Informed consent
Due to the study design and the anonymous by design database, based on Italian regulations, the signature of patient informed consent was not requested.
Additional information
Managed By Massimo Federici.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rossi, M.C., Bonfanti, R., Graziano, G. et al. Effectiveness of switching from first-generation basal insulin to Glargine 300 U/mL in children and adolescents with type 1 diabetes: results from the ISPED CARD database. Acta Diabetol (2024). https://doi.org/10.1007/s00592-024-02304-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00592-024-02304-2