Abstract
Aims
This study aimed to determine the minimum frequency of flash glucose monitoring (FGM) scans necessary for optimal glycemic control in patients with type 1 diabetes (T1D).
Methods
Data were collected from 692 patients (47.5% female, with a median age of 47.4 years) who used FGM systems daily and recorded their clinical variables and device data.
Results
Logistic regression models showed that performing more than 12 scans per day was associated with improved T1D control (OR = 4.22, p < 0.001) and a reduction in HbA1c (7.6 vs 7.0%, 60–53 mmol/mol p < 0.001). However, those performing less than 6 scans showed no improvement in HbA1c (7.9 vs 7.8%, 63–61 mmol/mol p = 0.514). Thirteen daily scans were determined as the optimal cutoff point for predicting optimal glycemic control using a maximally selected rank algorithm. Significant reductions were observed in mean glucose (< 0.001), coefficient of variation (< 0.001), HbA1c (< 0.001), and an increase in TIR (< 0.001) in patients who performed more than 12 daily scans.
Conclusions
The results suggest that a higher frequency of daily scans by T1D patients using FGM systems leads to improved chronic glycemic control. The minimum recommended frequency for optimal control is 13 scans per day, and more than 6 daily scans are needed to improve HbA1c.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Type 1 diabetes mellitus (T1D) requires accurate and frequent glucose measurements for proper metabolic control and prevention of complications [1]. Nowadays, the development and advances in continuous glucose monitoring (CGM) systems have been a substantial step forward in the monitoring and treatment of diabetes mellitus (DM) due to the simplicity of self-testing and the quality of the information, which has eventually led to improved disease management [2,3,4]. In this sense, the widespread access of patients with T1D to CGM devices can provide new insights into the determinants of disease control, given the large number of patients using these systems, particularly flash glucose monitoring (FGM) systems, and the enormous amount of data they provide.
The assessment of chronic control using glycated hemoglobin (HbA1c) is considered a less accurate measure than continuous interstitial glucose monitoring, either real-time (rt-CGM) or flash (FGM), to determine the optimal approach for patient management [5,6,7]. In addition, HbA1c does not allow an appropriate assessment of glycemic variability, time spent in hypoglycemia or within the glucose range, which are becoming increasingly important in clinical practice [8, 9].
Although capillary blood glucose self-testing provides very useful information, one of its main limitations [10] is its highly variable adherence [11, 12]. Regarding CGM, one of the issues that remain to be elucidated is the impact of daily scanning frequency. The International Consensus on Time in Range indicates that at least 70% of sensor usage time is necessary for reproducible data and clinical benefit from the use of this monitoring [13], although some studies have recently suggested that more time is probably needed to obtain the best performance from these sensors [14, 15]. Nonetheless, the importance of the frequency of scanning has been evaluated in children [16, 17] but remains to be assessed in adults.
Thus, this study aimed to assess the influence of daily FGM scanning on the chronic control of T1D as measured by both HbA1c and glycemic parameters provided by FGM systems and to estimate a cutoff point of number of daily scans for clinical benefits. Moreover, we aimed to validate the performance of this cutoff point by testing whether patients who are above this cutoff point have clinically significant improvements in glycemic control parameters.
Materials and methods
This is a retrospective follow-up study including 1135 patients who were regular users of the FreeStyle Libre® (Abbott) FGM system between July and August 2022 at two hospitals in Madrid, Spain. Patients diagnosed with T1D, cystic fibrosis-related diabetes (CFRD), and pancreatic diabetes were included. Patients with a diagnosis of type 2 diabetes (T2D) or MODY, those with a usage time of less than 70%, and those who did not have a download of sensor data in the 30 days before data collection were excluded. The final sample consisted of 692 patients. FGM data of these patients were retrieved from days 14 and 90 of follow-up.
Procedures
Prior to starting to use the FreeStyle monitor, all patients received a training session on the use of the monitor according to international recommendations [13]. The system consists of a glucose oxidase–based electrochemical sensor, which is placed subcutaneously and replaced every 14 days, along with a receiver to which interstitial glucose measurements are sent wirelessly and stored in the cloud using the Libreview platform. All patients were provided with written instructions on how to use the data provided by FGM to make real-time adjustments of insulin doses and on the use of Libreview cloud to retrospectively review the glucose data to adjust future insulin doses. All patients were instructed to modify their insulin doses and treatment of hypoglycemia based on their glucose trend.
Data collection
Data including sociodemographic and clinical details, as well as laboratory tests and pharmacologic medication for T1D, were obtained from electronic health records. Glucometric information cloud downloads from the Libreview platform using the FreeStyle 2 device (FreeStyle Libre 2®, Abbott) were retrieved at 14 and 90 days. We collected the following variables: time in range (TIR), time below and above range (glycemia < 70 mg/dL or > 180 mg/dL, respectively), number of daily readings, sensor usage, hypoglycemia events, coefficient of variation (CV) and standard deviation (SD). In addition, sociodemographic and clinical data were collected, including sex, age, duration of diabetes mellitus, type of diabetes, body mass index (BMI), smoking, continuous subcutaneous insulin infusion (CSII) carrier, baseline HbA1c (immediately before the sensor was placed), last available HbA1c, FGM usage time, time of disease evolution, age at disease onset, insulin dose, and retinopathy. Glycated hemoglobin was routinely determined using liquid chromatography (ADAMS A1c HA8180 V ARKRAY®).
All patients included in the study were informed of its objectives and accepted the use of their medical history data for research purposes. The Research Ethics Committee of Hospital de La Princesa, Madrid approved this study (Study number: 2022-4997-17/22).
Statistical analysis
The statistical analysis was performed using R version 4.0.3 [18] and STATA 17.0 statistical software. After checking the plausibility of outliers, the fitting to a normal distribution was examined using both statistical (Kolmogorov‒Smirnov test) and graphical (normal probability plot) procedures. Those variables with extreme values for which their authenticity was questionable were winsorized using the 99th and 1st percentiles of the distribution. Continuous variables are presented as the mean and standard deviation (SD), and categorical variables are presented as numbers and percentages of the samples. We calculated a dichotomous optimal glycemic control variable as time in range > 70% and time below range (< 70 mg/dL) < 4%, as recommended [13].
Bivariate differences were tested using Student’s t test and the Mann‒Whitney U test, depending on their adjustment to a normal distribution. Logistic regression models were estimated using HbA1c < 7% (53 mmol/mol) and optimal glycemic control as dependent variables, glycemic control variables (time in range, time spent in hypo- and hyperglycemia, hypoglycemia events), number of daily readings and sensor usage as independent variables, and sociodemographic and clinical variables as covariates. The MaxStat package of R was selected using maximally selected rank algorithm to identified the optimal cutoff point for the number of scans/days to achieve optimal glycemic control [19]. To validate the use of this cutoff point, we examined its influence on the chronic control of patients with T1D by testing mean differences in glycemic control parameters between those above and below this cutoff point. Moreover, analysis of variance was used to test the effect of daily scans frequency categories (3–6, 7–9, 10–12 and > 12) on pre/post HbA1c changes.
Results
Characteristics of the patients
Table 1 describes the characteristics of the study sample. After removing the 443 individuals who did not meet the inclusion criteria, data from 692 patients (47.5% females) aged between 18 and 89 years (mean 47.4, SD 15.5) were analyzed. Type 1 diabetes was the most frequent diagnosis (94.1% of the users), followed by pancreatic diabetes (4.43%) and cystic fibrosis-related diabetes (1.48%). The mean age at disease onset was 25.7 (SD 16.6) years, and the mean time of disease duration was 21.7 (SD 13.6) years. The mean duration of FGM FreeStyle Libre® usage (years) was 1.8 (SD 1.1). Of the study sample, 94.7% of patients were users of multiple doses of insulin in a bolus-basal strategy, and 5.4% were users of open loop CSII. HbA1c prior to FGM placement was 7.7 (± 1.29) % (61 ± 14.4 mmol/mol).
Glycemic control
Number of scans (> 12) OR = 4.22 (p < 0.001), smoking OR = 0.48 (p = 0.013), male sex OR = 1.63 (p = 0.022), age OR = 1.03 (p < 0.001), time of disease progression OR = 0.98 (p = 0.009), BMI OR = 1.07 (p = 0.03), use of open loop CSII OR = 0.20 (p = 0.033) and total daily insulin dose (TDD) OR = 0.97 (p < 0.001) were significant predictors of optimal glycemic control in a logistic regression model using the FGM data. Time as device user and type of DM were not independent predictors of good control (Fig. 1A).
Predictors of optimal glycemic control (A) and HbA1c < 7% (B) BMI: body mass index CFRD: cystic fibrosis-related diabetes DM3c: diabetes mellitus secondary to chronic pancreatitis and pancreatic cancer. More than 12 scans per day was the strongest predictor of optimal control in flash glucose parameters OR = 4.22 (p < 0.001) and HbA1c OR = 3.13 (p < 0.001)
When HbA1c < 7% (53 mmol/mol) was used as the glycemic control variable, > 12 daily readings were also the strongest independent predictor of glycemic control, OR = 3.13 (p < 0.001). Both male sex (OR = 1.99, p < 0.001) and smoking (OR = 0.49, p = 0.003) were also predictors of glycemic control estimated with HbA1c (Fig. 1B).
In the analysis of the 90-day FGM data, a scanning frequency equal to or greater than 12 readings per day remained a strong predictor of optimal glycemic control (OR = 3.1, p < 0.001). Age (OR = 1.03, p < 0.001), BMI (OR = 1.09, p = 0.03), duration of diabetes (OR = 0.97, p < 0.001) and TDD (OR = 0.98, p = 0.006). However, sex and smoking were not statistically significant independent factors (p = 0.061 and p = 0.306, respectively). (Figure S1) (Supplementary Data S1).
Cutoff point
The assessment of the cutoff point of a minimal number of readings for optimal glycemic control in T1D is depicted in Figure S2 (Supplementary Data S2). After obtaining a cutoff point of 13 readings, differences in glycemic parameters were tested between those who read sensor data more than 12 times and those who did not. Table 2 shows a significant reduction in mean blood glucose 167.5 to 147.5 mg/dL (< 0.001), coefficient of variation 36.8 to 32.8% (< 0.001), and HbA1c 7.5 to 7.0% (58.5–53 mmol/mol)(< 0.001) and a significant increase in the TIR 59.0 to 71.5% (< 0.001) in patients with more than 12 daily readings. No statistically significant differences were observed in time below range (< 70 mg/dL) (TBR) (p = 0.134).
Impact of daily scans on HbA1c improvement
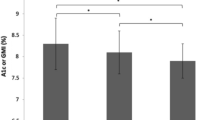
When studying the effect of daily readings on changes in HbA1c values by comparing pre/post sensor use HbA1c values (Fig. 2), an improvement of 0.6% (7 mmol/mol) (p < 0.001) in HbA1c was observed in the group with more than 12 daily scans. The groups of 7–9 and 10–12 daily scans also improved HbA1c by 0.4% (4 mmol/mol) (p = 0.005) and 0.3% (3 mmol/mol) (p = 0.002), respectively. However, no statistically significant improvement was observed in the group with fewer than six daily readings.
Influence of the number of sensor readings on HbA1c change after FGM placement. FGM: flash glucose monitoring. Patients who performed more than 12 daily scans per day showed an improvement of 0.65% (p < 0.001) in HbA1c. The groups of 6–9 and 9–12 daily scans also improved HbA1c by 0.36% (p = 0.005) and 0.39% (p = 0.002), respectively. However, no statistically significant improvement was observed in the group with fewer than six daily readings
Discussion
Our study aimed to examine the influence of FGM scanning frequency on chronic control of T1D and to estimate and validate a cutoff point for the minimum number of scans per day for optimal glycemic control. Our data support that thirteen is the minimum number of scans per day that provides better glycemic parameters and optimized glycemic control for these patients.
The usefulness of rt-CGM and FGM systems in the management of DM is currently unquestionable [20,21,22,23]. A reduction in up to 0.6% in HbA1c in patients with MDI (multiple insulin doses) using CGM compared to those using capillary blood glucose has been reported in randomized clinical trials [24, 25]. Moreover, improvements in other glycemic control parameters such as time in range or glycemic variability [15, 26], in both T1D [27] and T2D patients have been observed [28]. However, although most literature supports a beneficial effect on DM chronic control as assessed by HbA1c, issues such as the appropriate use of CGM have been rarely studied.
A potential association between the number of daily FGM scans and improvement of glycemic parameters was assessed by logistic regression. Controlling for other potential confounders, such as age, biological sex, BMI, smoking, age at onset and time from the diagnosis of T1D, our logistic regression model supports, in accordance with previous evidence [14, 29, 30], that the number of daily scans is directly associated with optimal glycemic control as assessed by both the sensor’s glycemic indicators and HbA1c value.
Moreover, data from these models, as well as ROC curves for determining the cutoff point for optimal glycemic control, estimated that more than twelve is the appropriate number of daily scans needed for better control of diabetes. This scanning frequency is greater than that recommended by the American Diabetes Association (up to one scan every 8 h) for the appropriate use of these devices. In addition, in our analyses, when comparing HbA1c data prior to device placement with the last HbA1c value available, patients who performed less than 6 daily scans did not improve their HbA1c control despite using the sensor within the international consensus recommendation of time in range (use > 70% with updated data) [13].
This cutoff point was further confirmed by two analysis strategies: the mean glycemic parameters were compared between those who met this mean number of scans/day and those who did not, and the change in HbA1c value at sensor placement was compared to the most recent one (median 1.8 years follow-up). Both the main glycemic parameter levels and HbA1c values were substantially better among those who performed more than 12 scans/day than among those who did not (Table 2). These results, together with cutoff curve analyses, support that optimal FGM use to improve glycemic control requires patients to scan FGM devices more than 12 times a day. However, it is difficult to assess the consistency of our estimates of the number of daily scans for optimal use of FGM devices because no similar study has been published thus far, with the exception of a study in children reporting an association between the number of scans per day and glycemic control [16, 17].
The observed beneficial effect of glucose readings on glycemic control may be attributed to an increased number of scans, indicating heightened awareness of blood glucose levels and enhanced quality and quantity of glycemic information. Nevertheless, the most crucial aspect of CGM lies in monitoring glucose trends and adjusting insulin dosages based on CGM data, facilitating better therapeutic decision-making and preventing hypoglycemia, a central objective in diabetes management [31].
In this context, our study did not observe any differences in TBR between the group with higher readings and the group with lower readings. One plausible explanation could be that the FreeStyle 2 system provides alarms to alert patients when they reach the TBR threshold, which might account for the low TBR rates in both groups (TBR 3.8 vs 4.4%). Consequently, this makes it challenging to identify statistically significant differences between the two groups.
Although in our study, the daily number of sensor scans was the variable most strongly associated with good glycemic control, associations have also been observed in non-smokers and males. The hyperglycemic effect of tobacco has been demonstrated in both T1D [32] and T2D [33] and appears to be mediated by the mTOR pathway [34]. On the other hand, in our study, female sex was associated with not achieving glycemic targets, which has been previously reported in studies with large patient samples [35, 36] However, none of these associations were observed in the sensor data analysis over 90 days.
Lastly, younger age, longer diabetes duration, and higher daily insulin requirements were consistently associated with poorer chronic control, as indicated by both glycated hemoglobin and sensor data at 14 and 90 days. These findings are consistent with results from a large cohort study conducted in 75 centers in our country [37], where similar outcomes were observed.
This study has certain limitations that should be acknowledged. First, it is an observational follow-up study that does not allow to compare the efficacy in improving glycemic control between patients with and without FGM devices. Moreover, although we controlled for numerous covariates in the analyses, some potential confounders that we were unable to control, such as dietary habits, level of diabetes education or socioeconomic status, could influence the validity of our results. Secondly, the inclusion criteria, where patients with a high usage time of FGM (> 70%) and regular download of sensor data were included, could potentially introduce bias in the scan frequency. Third, the two centers from which the patients were enrolled are located in different cities, within the same region, so our conclusions may not be completely extended to overall patients with T1D. Forth, the effect on long-term glycemic control was not evaluated; thus, prospective studies will be necessary to evaluate the long-term effect of daily scanning frequency on glycemic control parameters.
Another limitation of our study is not having analyzed the time in tight range, (the time when glucose readings are within 70–140 mg/dL or 3.9–7.8 mmol/L), which is an emerging variable as an informed measure of time in range, particularly for individuals with type 1 diabetes using automated insulin delivery systems or individuals with type 2 diabetes using glucose-lowering agents [13].
Last, glycemic parameters are commonly used because there is consistent evidence supporting that optimum control of these indicators delays the onset of diabetic complications. However, only long-term follow-up studies comparing the incidence of these complications in those who adequately use FGM devices and those who do not would be able to provide solid evidence as to whether the use of these devices could delay the onset of diabetic complications.
In conclusion, our study supports the notion that increased daily scanning frequency using FGM systems leads to improved glycemic control in individuals with T1D. Our findings suggest that a minimum of 13 scans per day could be necessary to achieve optimal control, while a frequency greater than 6 scans per day can result in improved HbA1c levels.
Data availability
F.S.-V and M.M. are the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
DCCT/EDIC Research Group (2015) Intensive diabetes therapy and ocular surgery in type 1 diabetes. N Engl J Med 372(18):1722–1733. https://doi.org/10.1056/NEJMoa1409463
Benkhadra K, Alahdab F, Tamhane S et al (2017) Real-time continuous glucose monitoring in type 1 diabetes: a systematic review and individual patient data meta-analysis. Clin Endocrinol 86(3):354–360. https://doi.org/10.1111/cen.13290
Olczuk D, Priefer R (2018) A history of continuous glucose monitors (CGMs) in self-monitoring of diabetes mellitus. Diabetes Metab Syndr 12(2):181–187. https://doi.org/10.1016/j.dsx.2017.09.005
Ampudia-Blasco FJ, Ugarte-Abasolo E, Chico A, García-Alemán J, Galan-Barroso M (2022) Spanish consensus on the Use of isCGM in the management of patients with insulin therapy: the MONITOR project. J Diabetes Sci Technol. https://doi.org/10.1177/19322968221087270
Beck RW, Connor CG, Mullen DM, Wesley DM, Bergenstal RM (2017) The fallacy of average: how using HbA1c alone to assess glycemic control can be misleading. Diabetes Care 40(8):994–999. https://doi.org/10.2337/dc17-0636
Vigersky RA, McMahon C (2019) The relationship of hemoglobin A1C to time-in-range in patients with diabetes. Diabetes Technol Ther 21(2):81–85. https://doi.org/10.1089/dia.2018.0310
Bellido V, Pinés-Corrales PJ, Villar-Taibo R, Ampudia-Blasco FJ (2021) Time-in-range for monitoring glucose control: is it time for a change? Diabetes Res Clin Pract. https://doi.org/10.1016/j.diabres.2021.108917
Charleer S, Mathieu C, Nobels F et al (2018) Effect of continuous glucose monitoring on glycemic control, acute admissions, and quality of life: a real-world study. J Clin Endocrinol Metab 103(3):1224–1232. https://doi.org/10.1210/jc.2017-02498
Klonoff DC, Buckingham B, Christiansen JS et al (2011) Continuous glucose monitoring: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 96(10):2968–2979. https://doi.org/10.1210/jc.2010-2756
Hortensius J, Kars MC, Wierenga WS, Kleefstra N, Bilo HJ, van der Bijl JJ (2012) Perspectives of patients with type 1 or insulin-treated type 2 diabetes on self-monitoring of blood glucose: a qualitative study. BMC Public Health 12(1):167. https://doi.org/10.1186/1471-2458-12-167
Mathur P, Leburu S, Kulothungan V (2022) Prevalence, awareness, treatment and control of diabetes in India from the countrywide national NCD monitoring survey. Front Public Health 10:748157. https://doi.org/10.3389/fpubh.2022.748157
Irazola V, Rubinstein A, Bazzano L et al (2017) Prevalence, awareness, treatment and control of diabetes and impaired fasting glucose in the Southern Cone of Latin America. PLoS One 12(9):e0183953. https://doi.org/10.1371/journal.pone.0183953
Battelino T, Alexander CM, Amiel SA et al (2023) Continuous glucose monitoring and metrics for clinical trials: an international consensus statement. Lancet Diabetes Endocrinol 11(1):42–57. https://doi.org/10.1016/S2213-8587(22)00319-9
Hohendorff J, Gumprecht J, Mysliwiec M, Zozulinska-Ziolkiewicz D, Malecki MT (2021) intermittently scanned continuous glucose monitoring data of polish patients from real-life conditions: more scanning and better glycemic control compared to worldwide data. Diabetes Technol Ther 23(8):577–585. https://doi.org/10.1089/dia.2021.0034
Reddy M, Oliver N (2020) Self-monitoring of blood glucose requirements with the use of intermittently scanned continuous glucose monitoring. Diabetes Technol Ther 22(3):235–238. https://doi.org/10.1089/dia.2019.0369
Suzuki J, Urakami T, Yoshida K et al (2021) Association between scanning frequency of flash glucose monitoring and continuous glucose monitoring-derived glycemic makers in children and adolescents with type 1 diabetes. Pediatr Int 63(2):154–159. https://doi.org/10.1111/ped.14412
Urakami T, Yoshida K, Kuwabara R et al (2022) Frequent scanning using flash glucose monitoring contributes to better glycemic control in children and adolescents with type 1 diabetes. J of Diabetes Invest 13(1):185–190. https://doi.org/10.1111/jdi.13618
Team R Core R: A language and environment for statistical computing. Published online 2013
Hothorn T, Hothorn MT, Suggests TH. Package ‘maxstat.’ Published online 2017
Deshmukh H, Wilmot EG, Gregory R et al (2020) Effect of flash glucose monitoring on glycemic control, hypoglycemia, diabetes-related distress, and resource utilization in the association of british clinical diabetologists (ABCD) nationwide audit. Diabetes Care 43(9):2153–2160. https://doi.org/10.2337/dc20-0738
Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group (2009) The effect of continuous glucose monitoring in well-controlled type 1 diabetes. Diabetes Care 32(8):1378–1383. https://doi.org/10.2337/dc09-0108
Bellido V, Aguilera E, Cardona-Hernandez R et al (2022) Expert recommendations for using time-in-range and other continuous glucose monitoring metrics to achieve patient-centered glycemic control in people with diabetes. J Diabetes Sci Technol. https://doi.org/10.1177/19322968221088601
Oyagüez I, Merino-Torres JF, Brito M et al (2020) Cost analysis of the flash monitoring system (FreeStyle Libre 2) in adults with type 1 diabetes mellitus. BMJ Open Diab Res Care 8(1):e001330. https://doi.org/10.1136/bmjdrc-2020-001330
Beck RW, Riddlesworth T, Ruedy K et al (2017) Effect of continuous glucose monitoring on glycemic control in adults with type 1 diabetes using insulin injections: the DIAMOND randomized clinical trial. JAMA 317(4):371. https://doi.org/10.1001/jama.2016.19975
Leelarathna L, Evans ML, Neupane S et al (2022) Intermittently scanned continuous glucose monitoring for type 1 diabetes. N Engl J Med 387(16):1477–1487. https://doi.org/10.1056/NEJMoa2205650
Xing D, Kollman C, Beck RW et al (2011) Optimal sampling intervals to assess long-term glycemic control using continuous glucose monitoring. Diabetes Technol Ther 13(3):351–358. https://doi.org/10.1089/dia.2010.0156
Dicembrini I, Cosentino C, Monami M, Mannucci E, Pala L (2021) Effects of real-time continuous glucose monitoring in type 1 diabetes: a meta-analysis of randomized controlled trials. Acta Diabetol 58(4):401–410. https://doi.org/10.1007/s00592-020-01589-3
Maiorino MI, Signoriello S, Maio A et al (2020) Effects of continuous glucose monitoring on metrics of glycemic control in diabetes: a systematic review with meta-analysis of randomized controlled trials. Diabetes Care 43(5):1146–1156. https://doi.org/10.2337/dc19-1459
Gomez-Peralta F, Dunn T, Landuyt K, Xu Y, Merino-Torres JF (2020) Flash glucose monitoring reduces glycemic variability and hypoglycemia: real-world data from Spain. BMJ Open Diab Res Care 8(1):e001052. https://doi.org/10.1136/bmjdrc-2019-001052
Dunn TC, Xu Y, Hayter G, Ajjan RA (2018) Real-world flash glucose monitoring patterns and associations between self-monitoring frequency and glycaemic measures: a European analysis of over 60 million glucose tests. Diabetes Res Clin Pract 137:37–46. https://doi.org/10.1016/j.diabres.2017.12.015
Urakami T (2022) Significance of the CGM metric of time in range in children and adolescents with type 1 diabetes. Endocr J 69(9):1035–1042. https://doi.org/10.1507/endocrj.EJ22-0257
Jensen MH, Cichosz SL, Hirsch IB, Vestergaard P, Hejlesen O, Seto E (2021) Smoking is associated with increased risk of not achieving glycemic target, increased glycemic variability, and increased risk of hypoglycemia for people with type 1 diabetes. J Diabetes Sci Technol 15(4):827–832. https://doi.org/10.1177/1932296820922254
Peng K, Chen G, Liu C et al (2018) Association between smoking and glycemic control in diabetic patients: results from the risk evaluation of cAncers in Chinese diabeTic individuals: a lONgitudinal (REACTION) study. J Diabetes 10(5):408–418. https://doi.org/10.1111/1753-0407.12625
Fraenkel M, Ketzinel-Gilad M, Ariav Y et al (2008) mTOR Inhibition by rapamycin prevents β-cell adaptation to hyperglycemia and exacerbates the metabolic state in type 2 diabetes. Diabetes 57(4):945–957. https://doi.org/10.2337/db07-0922
Dover AR, Strachan MWJ, McKnight JA et al (2021) Socioeconomic deprivation, technology use, C-peptide, smoking and other predictors of glycaemic control in adults with type 1 diabetes. Diabet Med 38(3):e14445. https://doi.org/10.1111/dme.14445
Manicardi V, Russo G, Napoli A et al (2016) Gender-disparities in adults with type 1 diabetes: more than a quality of care issue a cross-sectional observational study from the AMD annals initiative. PLOS One 11(10):e0162960. https://doi.org/10.1371/journal.pone.0162960
Gómez-Peralta F, Menéndez E, Conde S, Conget I, Novials A (2021) Características clínicas y manejo de la diabetes tipo 1 en España. Estudio SED1. Endocrinol Diabetes y Nutr 68(9):642–653. https://doi.org/10.1016/j.endinu.2020.11.002
Acknowledgements
We appreciate helpful comments made by Jose María Galván Román.
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
FS-V, JM-A, and VM-V were involved in the study design, researched data, contributed to discussion, and wrote/edited the article. MASN and IHA performed statistical analyses. JAA and MM wrote/edited the article. JJ-D, VNM, TAJ, MMFG, GLRG, LEL and PMI were involved in data collection and reviewed/edited the article.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Ethics approval
All the participants enrolled in this study provided their consent prior to their inclusion, explicitly granting permission for the utilization of their medical history data for research purposes. No animals were used in this study. Furthermore, the study protocol received formal approval from the local Research Ethics Committee and was meticulously conducted in strict accordance with the principles outlined in the Declaration of Helsinki, which govern research involving human subjects (Study number: 2022-4997-17/22).
Informed consent
All patients included in the study were informed of its objectives and accepted the use of their medical history data for research purposes. The Research Ethics Committee of Hospital de La Princesa, Madrid approved this study (Study number: 2022-4997-17/22).
Additional information
Managed by Giovanni Sartore.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The results of this study have been presented as a short poster at the XXI SENDIMAD congress on 25-26 November 2022 in Aranjuez (Madrid, Spain).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sebastian-Valles, F., Martínez-Alfonso, J., Arranz Martin, J.A. et al. Scans per day as predictors of optimal glycemic control in people with type 1 diabetes mellitus using flash glucose monitoring: what number of scans per day should raise a red flag?. Acta Diabetol 61, 343–350 (2024). https://doi.org/10.1007/s00592-023-02204-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-023-02204-x