Abstract
Aims
To examine the association between COVID-19 Shutdown and within-subjects changes in body weight, body mass index (BMI), and glycemic parameters using electronic health record (EHR) data from 23,000 adults with type 2 diabetes (T2DM).
Methods
Patients with T2DM with outpatient visit data on body weight, BMI, hemoglobin A1c (HbA1c), and blood glucose (≥ 2 measures before and after 3/16/2020) recorded in the EHR at the University of Pittsburgh Medical Center were included. A within-subjects analysis compared average and clinically significant changes in weight, BMI, HbA1c, and blood glucose during the year POST-Shutdown (Time 2–3) compared to the same interval during the PRE-Shutdown year (Time 0–1) using paired samples t-tests and the McNemar-Bowker test.
Results
We studied 23,697 adults with T2DM (51% female; 89% White; mean age = 66 ± 13 years; mean BMI = 34 ± 7 kg/m2; mean HbA1c = 7 ± 2% [53 ± 21.9 mmol/mol]). Weight and BMI decreased during both the PRE- and POST-Shutdown intervals, but the changes were statistically smaller during the year POST-Shutdown relative to PRE (0.32 kg and 0.11 units, p < 0.0001). HbA1c showed statistically greater improvements during the POST-Shutdown interval compared to PRE (− 0.18% [−2 mmol/mol], p < 0.0001), but changes in glucose did not differ for the two intervals.
Conclusions
Despite widespread discussion of weight gain in association with the COVID-19 Shutdown, study data showed no evidence of adverse effects of Shutdown on body weight, BMI, HbA1C, or blood glucose in a large sample of adults with T2DM. This information may help to inform future public health decision-making.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In March 2020, the global spread of SARS-CoV-2 led to the implementation of stay-at-home orders across the U.S., causing abrupt changes to daily living. During and following this “Shutdown” period, reports of pandemic-related weight gain (popularly nicknamed “the Quarantine-15”) were widespread in the mass media [1], and data from several studies in the general population corroborated these reports [2,3,4]. For individuals with type 2 diabetes (T2DM), who are already at higher risk of COVID-19-related morbidity and mortality given their typical age, weight, and metabolic disease [5], weight gain may pose particular risks to health by impairing glycemic control and exacerbating diabetes-related health consequences [6]. Furthermore, Shutdown presented significant challenges to diabetes self-management, including physical activity restrictions, pandemic-related stress, changes in eating patterns, social isolation, and less access to in-person healthcare and metabolic testing [7, 8]. These barriers may contribute to increased caloric intake, reduced physical activity, and less consistent engagement in diabetes self-management behaviors [7, 9]. Thus, COVID-19 Shutdown may be associated with weight gain and poorer glycemic control among adults with T2DM.
However, research investigating effects of Shutdown on body weight and glycemic control among individuals with T2DM has found inconsistent results, even across meta-analyses [9,10,11]. Several studies link Shutdown to small weight gains [i.e., < 2 kg; 12, 13–16] and to increases in hemoglobin A1c (HbA1c) and blood glucose (e.g., 7–15 mg/dL) [12, 14, 16,17,18]. Yet other studies show no evidence of significant Shutdown-associated changes in weight [17, 19,20,21] or glycemic parameters [20,21,22], and some studies show POST-Shutdown improvements in HbA1c and blood glucose levels [13, 19, 23].
The mixed evidence on associations between Shutdown, weight, and metabolic health in adults with T2DM may be attributable to methodological limitations. Although several existing studies utilize electronic health record (EHR) data from patients with T2DM in clinical settings, most of these studies sampled less than 150 patients, with only a few studies including more than 300 participants [15, 17,18,19]. Most studies also used cross-sectional methods or simple pre-post designs that compared one measure taken POST-Shutdown to one taken PRE-Shutdown, approaches that may potentially misattribute weight gain to Shutdown instead of to the patients’ typical weight trajectory. Finally, existing research has mostly occurred outside the U.S. [9,10,11], and given differences in national healthcare systems and Shutdown restrictions, it may be difficult to generalize findings from prior work to U.S. samples.
Given that weight management and glycemic control are critical determinants of health in adults with T2DM [6], research using stronger methodology is needed to improve our understanding of the COVID-19 Shutdown’s effects on body weight and glycemic control in this population. To our knowledge, there are no previous studies in patients with T2DM that have used a within-subjects design to examine individuals’ changes in weight and metabolic parameters in the period following Shutdown compared to their changes in these parameters during the prior year. The current study aimed to fill this gap and enhance the rigor of prior work by using EHR data from adults with T2DM enrolled in a large healthcare organization to conduct a within-subjects analysis that examined the trajectory of change in body weight, body mass index (BMI), and glycemic control (i.e., HbA1c, blood glucose) that occurred during the year following COVID-Shutdown (“POST-Shutdown”) compared to the year prior to Shutdown (“PRE-Shutdown.”).
Research design and methods
Data source and timeline
This study used data from ambulatory visits (excluding emergency room or in-patient hospital visits) captured via the EHR at the University of Pittsburgh Medical Center (UPMC). UPMC is an integrated academic medical center that serves over 200,000 patients across Pennsylvania [24]. Data were drawn from outpatient visits from 22 UPMC hospitals that had been harmonized in the UPMC Clinical Data Warehouse. The beginning of the COVID-19 Shutdown period was defined as 3/16/2020. This date was used to define 4 timepoints for data extraction: two “PRE-Shutdown” timepoints (Time 0 and Time 1), which were used to determine changes in weight and glycemic control prior to Shutdown as a control period, and two “POST-Shutdown” timepoints (Time 2 and Time 3), which provided POST-Shutdown trajectories for comparison. Figure 1 depicts the precise timeline that defined these data collection intervals.
Study population
Data were extracted from the EHR for patients who met the following characteristics: (1) were adults who had been diagnosed with T2DM at least 1 year prior to 3/16/20; (2) had ≥ 2 BMI measurements prior to 3/16/20 that were at least 90 days apart, with the most recent being ≥ 90 days before 3/16/20; and (3) had ≥ 2 BMI measurements on or after 3/16/20 that were at least 90 days apart, with the first being ≥ 90 days after 3/16/20. The UPMC Ethics and Quality Improvement Review Committee granted formal ethics approval for study procedures as an exempt protocol (ID 2882) and data were de-identified.
Measures
EHR data obtained during outpatient medical visits was extracted for key outcome measures, including measures of body weight, BMI, HbA1c, and blood glucose (blood glucose measures likely included both fasting and random values, limiting their rigor.) Other data extracted from the EHR included patients’ currently prescribed diabetes medications, visit format (i.e., in-person or tele-medicine), and demographic data (e.g., age, biological sex, racial background). The Area Deprivation Index (ADI) was used to determine socioeconomic status, with individuals at or above the 85th percentile categorized as having greater disadvantage [25].
Analytic plan
Primary Analyses. Data values in the top and bottom 0.05 percentile of the range for each outcome were reviewed to identify biologically implausible values based on pre-defined criteria (i.e., weight < 36 or > 227 kg; BMI < 15 or > 65 units; HbA1c < 3 or > 15%; blood glucose < 30 or > 600 mg/dL) or implausible changes in values. Analyses were performed using SAS software Version 9.4 (SAS Institute, Inc., Cary, NC). Paired samples t-tests were used to compare POST-Shutdown changes in weight, BMI, and glycemic parameters to PRE-Shutdown changes. The McNemar-Bowker test was used to compare the proportion of patients who displayed clinically significant changes in weight, BMI, and glycemic outcomes during the POST-Shutdown interval (Time 2 to 3) versus PRE-Shutdown (Time 0 to 1). Clinically significant changes in study parameters were defined as 5% weight change, 2 BMI units, 0.5% change in HbA1c, and ≥ 30 mg/dL change in blood glucose [26, 27]. Two-tailed p-values were set at < 0.0001 due to the large sample size.
Sensitivity analyses. Sensitivity analyses were also performed to account for potential biases. To reduce concerns that visit format (i.e., in-person vs. telemedicine visit) or changes in T2DM medication during the study influenced results, sensitivity analyses were conducted using patients with only in-person visits and, separately, among patients with no changes in the class of medications prescribed during the study period. To reduce concerns that selecting patients with 2 visits PRE- and POST-Shutdown would disproportionately select compliant patients who were closely connected to care, sensitivity analyses were also conducted in patients with only 1 BMI measure collected during an in-person visit 5–7 months before the onset of COVID (3/16/2020) and 5–7 months after COVID onset, with the measure closest to 3/16/2020 selected.
Subgroup analyses. Descriptive statistics on change in weight during the PRE- and POST-Shutdown time intervals were examined for pre-specified subgroups defined by sex (male; female), ADI (0- < 85 percentile; ≥ 85 percentile), age (18–35; 36–50; 51–60; 61–70; ≥ 71 years), race (white; black; other), BMI category (< 18.5; 18.5- < 25; 25- < 30; 30- < 35; ≥ 35 kg/m2), and type 2 diabetes medication regimen (no medications; oral medications only; insulin) based on values reported at Time 0.
Results
Descriptive statistics
A total of 23,697 patients met eligibility criteria and had plausible outcome data (n = 86 screened out due to implausible values). Participant characteristics are outlined in Table 1.
On average, there were 11.6 ± 2.4 months between the first and final measures of the PRE-Shutdown period (Time 0–1), 11.3 ± 2.4 months between POST-Shutdown measures (Times 2–3), and 25.5 months between the first and final measures (Times 0–3).
Changes in weight and BMI POST- versus PRE-Shutdown
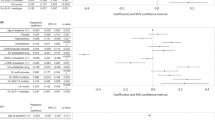
As seen in Table 2, on average patients lost a small amount of weight during both the PRE- and POST-Shutdown periods. The magnitude of weight loss was significantly smaller in the period POST-Shutdown (− 0.51 kg) versus PRE-Shutdown (− 0.83 kg), a statistical difference of 0.32 kg (p < 0.0001; 95% CI: 0.21–0.44 kg). Findings for BMI were similar (p < 0.0001).
The proportion of patients who displayed clinically meaningful changes in body weight (i.e., ≥ 5% weight loss/gain) and BMI (≥ 2 units) was also statistically different in the year POST- versus PRE-Shutdown principally (p < 0.0001; Fig. 2). Although over two-thirds of patients stayed within 5% of their initial weight during both time periods, slightly more patients gained a clinically significant amount of weight in the year POST-Shutdown (14.5%) versus PRE-Shutdown (12.2%), and slightly fewer patients lost a clinically significant amount of weight POST- (17.6%) versus PRE-Shutdown (18.1%). Over 70% of patients stayed within 2 BMI units in both years.
Changes in glycemic control POST- versus PRE-Shutdown
Table 2 shows that on average patients with T2DM (n = 19,099) showed statistically larger reductions in HbA1c in the year POST-Shutdown (− 0.19% [− 2.1 mmol/mol]) versus PRE- (− 0.01% [− 0.1 mmol/mol]), a difference of − 0.18% (− 2.0 mmol/mol; p < 0.0001; 95% CI − 0.21%, − 0.17%). There was no statistical difference between changes in blood glucose levels POST- versus PRE-Shutdown (− 0.30 mg/dL, p = 0.68; 95% CI − 1.72, 1.13).
The proportion of patients reporting clinically significant changes in HbA1C (≥ 0.5% more or less) and blood glucose (i.e., ≥ 30 mg/dL more or less) differed statistically comparing POST- to PRE-Shutdown (p < 0.0001; Fig. 2). During both periods, most patients showed no clinically significant changes in HbA1c or blood glucose levels, though during the POST-Shutdown period more patients reported clinically significant HbA1c improvements (30.5% POST vs. 24.8% PRE) and fewer reported worsening levels than in the prior year (18.9% POST vs. 26.0% PRE).
Sensitivity analyses
Changes in patients’ diabetes medication use during the year POST-Shutdown were comparable to changes observed PRE-Shutdown. A sensitivity analysis conducted only in patients with no medication changes from Times 0–3 (69.2% of total sample) confirmed results from the primary analysis that showed no meaningful differences between changes seen in weight, BMI, HbA1c, and blood glucose during the POST-Shutdown interval compared to PRE (Supp. Table 1A).
In a paired t-test that only examined changes in outcomes among patients with in-person visits (81.7% of total sample), results supported the primary analysis (Supp. Table 1B). A final sensitivity analysis (Supp. Table 1C) selected patients with at least one measurement in the 6 months PRE- and POST-Shutdown (versus the primary analysis requiring 2 PRE- and POST-Shutdown measures). There were 361 ± 198 average days between PRE/POST measures. Results of this sensitivity analysis showed no clinically significant changes in weight (− 0.1 kg), BMI (− 0.2 units), HbA1c (− 0.1% or − 1.1 mmol/mol), and blood glucose (+ 0.2 mg/dL) PRE- to POST-Shutdown.
Subgroup analyses
Trajectories of change in weight were stratified by sex, ADI, age, race, initial BMI category, and type 2 diabetes medication regimen (Supp. Table 2). There was no indication of meaningful differences in patterns of weight change based on sex, ADI, or race, with patients in nearly all subgroups losing slightly less weight (0.2–0.6 kg) in the year POST- versus PRE-Shutdown. Across age groups, all subgroups showed slightly less weight loss (0.2–1.0 kg) in the year POST- compared to PRE-Shutdown, with the smallest difference seen in older adults (≥ 71 years; 0.2 kg less weight loss) and the largest difference seen in younger adults (18–35 years; 1 kg less weight loss). Weight change patterns were similar for adults in most BMI categories, although the largest differences were seen in patients with a BMI < 18.5, who gained less weight POST-Shutdown (− 0.1 kg) versus PRE (+ 2.5 kg), and among those with a BMI ≥ 35 kg/m2, who lost less weight POST-Shutdown (− 0.9 kg) versus PRE (− 1.8 kg). Weight changes were also similar for individuals using different diabetes medication regimens.
Discussion
This study examined whether the COVID-19 Shutdown led to changes in body weight, BMI, and glycemic control in 23,000 adults with T2DM enrolled in a large healthcare system. In contrast to mass media reports and some prior studies [2, 12] suggesting possible weight gain in association with the COVID-19 Shutdown, our results showed that on average adults with T2DM had small weight losses and BMI reductions during the year following Shutdown. In addition, we found that HbA1c improved during the POST-Shutdown interval relative to PRE-Shutdown. Although these changes were statistically significant, the differences between the two time intervals were not clinically meaningful (e.g., weight loss of 0.51 kg in the year POST-Shutdown vs 0.83 kg PRE-Shutdown and HbA1c change of − 0.19% POST-Shutdown vs − 0.01% PRE are not clinically meaningful differences [26, 27]). Likewise, only a small proportion of patients had clinically significant improvements or worsening in weight or metabolic parameters during either year, with the majority of patients showing no clinically significant changes in weight or glycemic outcomes both PRE- and POST-Shutdown. Several sensitivity analyses confirmed the results of these primary analyses and suggest that these results were not due to selection of patients with more frequent medical visits, changes in diabetes medications, or to inclusion of telemedicine visits.
To our knowledge, this is the first study of adults with T2DM to use a within-subjects design to assess changes in a patients’ weight and glycemic outcomes during the year POST-Shutdown compared to their own changes in the year prior to the Shutdown as a control condition [9,10,11]. This approach allowed us to determine whether the changes in weight, BMI, and glycemic parameters that were observed following Shutdown differed from individuals’ typical changes during the PRE-Shutdown period. In addition, by studying the same person PRE- and POST-Shutdown, this design controlled for fixed factors (i.e., sex) that other studies only accounted for by including these factors as covariates.
Prior studies examining POST-Shutdown changes in weight and metabolic health in adults with T2DM show marked heterogeneity in outcomes, likely due to variability in study designs, assessment timelines, and sample size and characteristics [9,10,11]. Our findings showing no evidence of POST-Shutdown weight gain are consistent with results from the most rigorous prior studies on this topic [19, 21]. For example, one study [21] found that BMI remained stable in a cohort of 141 adults with T2DM during the year POST-Shutdown, and a comparable BMI trajectory was seen in 123 matched controls during the same time interval PRE-Shutdown. Beyond individuals with T2DM, results from this study align with those of a large within-subjects study [28] of over 100,000 adults from the general population showing no differences in weight changes observed among patients in the year PRE- and POST-Shutdown, with weight remaining stable (+ 0.2 kg) in both years. Finally, this study’s finding that Shutdown was not associated with worsened glycemic control in adults with T2DM is consistent with prior work [9, 11, 13, 19,20,21,22,23].
The current study’s large sample size also provided the statistical power needed to examine differences in POST-Shutdown weight change across subgroups based on age, sex, race, ADI, and initial BMI levels, differences that have been explored among adults in the general population [28,29,30,31] but only in a few studies of adults with T2DM [15, 16]. Descriptive data from this study showed no differences in POST-Shutdown weight change based on sex, ADI, or racial background, though results related to race and ADI should be interpreted cautiously given the lack of racial and socioeconomic diversity in this sample. Although there were no dramatic differences in weight change based on age or initial BMI, we did see that younger adults (18–35) and those with the highest starting BMIs lost less weight during the POST- versus PRE-Shutdown year. This finding is consistent with prior data from the general population showing that younger adults and those with higher BMIs are most likely to experience weight gain over time and especially during the pandemic [29,30,31,32].
These results provide no evidence that the COVID-19 Shutdown led on average to weight gain or worsening in glycemic control among adults with T2DM or that these negative effects were seen in a substantial proportion of individuals. This finding is important given that weight gain—particularly clinically significant weight gain—is known to impair metabolic health in this population [6, 7] and poor long-term glycemic control is robustly related to risk for macro-and microvascular disease and all-cause mortality in adults with T2DM [33, 34]. Taken together, the strong evidence from this study may alleviate concerns that Shutdown restrictions led to deteriorations in health among adults with T2DM.
Strengths and limitations
The current study advances prior research examining effects of Shutdown on weight in people with T2DM by drawing from a large representative sample, using EHR-assessed outcomes, and utilizing a within-subjects design that compared patients’ weight change trajectories POST-Shutdown with their own data from the prior year [9,10,11]. This is also one of the first studies in adults with T2DM with a large enough sample to examine differences in POST-Shutdown weight change across demographic subgroups. This study also enhances the rigor of prior work by including several sensitivity analyses, which showed that results from the primary analysis were robust to effects of potential confounding factors, analyses that few past studies have reported [9,10,11].
This study also has limitations. The retrospective design limits our ability to draw causal conclusions about associations between the COVID-19 Shutdown and weight change. Data were also collected using EHR records, so measures of weight, HbA1c, and blood glucose were not tightly controlled or standardized [35]. This was of particular concern for blood glucose measures, which likely included both fasting and random values, limiting the interpretability and generalizability of these findings. The EHR also did not reliably assess COVID-19 diagnoses for ambulatory visits, so we were unable to conduct sensitivity analyses to examine whether patterns of weight change differed for individuals with versus without a COVID-19 diagnosis during the POST-Shutdown interval. This is an important direction for future studies given links between more severe cases of COVID-19 and weight loss [36]. Additionally, it is also possible that co-morbid conditions (e.g., hypertension, cancer) or their associated treatment regimens influenced weight or glycemic change over time. However, given the limited feasibility of controlling for each possible condition, treatment, and their combinations, this analysis did not control for these factors.
Finally, the sample was composed of individuals from a large academic health center who were connected with regular healthcare and a minority of participants identified as people of color (11%) or met criteria for significant socioeconomic disadvantage (11%). T2DM disproportionately affects people of color and individuals with socioeconomic disadvantage [37], populations that have experienced high rates of COVID-19 infection, morbidity, and mortality [38], so it is possible that study findings do not adequately capture effects of COVID-19 Shutdown on metabolic health in two at-risk subgroups. However, it is notable that in a large sample of culturally diverse and under-insured patients in Massachusetts, patients with T2DM showed no evidence of average or clinically significant weight gain PRE- to POST-Shutdown [30].
Conclusions
Despite widespread discussion of weight gain in association with COVID-19 Shutdown [9,10,11], data from this within-subjects analysis showed no evidence of adverse effects of Shutdown on body weight, BMI, HbA1c, or blood glucose in over 23,000 adults with T2DM from a large healthcare system. This information may help to inform future public health decision-making regarding the risk:benefit ratio of pandemic-related shutdowns and their impact on metabolic health in adults with T2DM.
Data Availability
Deidentified participant data that includes primary study endpoints (weight, BMI, HbA1c, blood glucose) will be made available upon reasonable request (i.e., for the purpose of reproducing study findings) and pursuant to contractual agreements.
References
Pearl RL (2020) Weight stigma and the “Quarantine-15.” Obesity 28(7):1180. https://doi.org/10.1002/oby.22850
Bhutani S, vanDellen MR, Cooper JA (2021) Longitudinal weight gain and related risk behaviors during the COVID-19 pandemic in adults in the US. Nutrients 13(2):671. https://doi.org/10.3390/nu13020671
Glazer SA, Vallis M (2022) Weight gain, weight management and medical care for individuals living with overweight and obesity during the COVID-19 pandemic (EPOCH study). Obes Sci Pract. https://doi.org/10.1002/osp4.591
Dicken SJ, Mitchell JJ, Newberry Le Vay J, et al (2021) Impact of COVID-19 pandemic on weight and BMI among UK adults: a longitudinal analysis of data from the HEBECO study. Nutrients 13(9):2911. https://doi.org/10.3390/nu13092911
Huang I, Lim MA, Pranata R (2020) Diabetes mellitus is associated with increased mortality and severity of disease in COVID-19 pneumonia–a systematic review, meta-analysis, and meta-regression. Diabetes Metab Syndr 14(4):395–403. https://doi.org/10.1016/j.dsx.2020.04.018
Klein S, Sheard NF, Pi-Sunyer X et al (2004) Weight management through lifestyle modification for the prevention and management of type 2 diabetes: rationale and strategies. A statement of the American Diabetes Association, the North American Association for the Study of Obesity, and the American Society for Clinical Nutrition. Am J Clin Nutr 80(2):257–263.
Banerjee M, Chakraborty S, Pal R (2020) Diabetes self-management amid COVID-19 pandemic. Diabetes Metab Syndr 14(4):351–354. https://doi.org/10.1016/j.dsx.2020.04.013
American Psychological Association. Stress in America: one year later a new wave of pandemic health concerns, March 2021 [Available from: https://www.apa.org/news/press/releases/stress/2021/sia-pandemic-report.pdf.
Wafa IA, Pratama NR, Sofia NF et al (2022) Impact of COVID-19 lockdown on the metabolic control parameters in patients with diabetes mellitus: a systematic review and meta-analysis. Diabetes Metab J 46(2):260–272. https://doi.org/10.4093/dmj.2021.0125
Ojo O, Wang X-H, Ojo OO et al (2022) The effects of COVID-19 lockdown on glycaemic control and lipid profile in patients with type 2 diabetes: a systematic review and meta-analysis. Int J Environ Res Public Health 19(3):1095. https://doi.org/10.1177/1010539522110856
Silverii AG, Poggi CD, Dicembrini I, et al. (2021) Glucose control in diabetes during home confinement for the first pandemic wave of COVID-19: a meta-analysis of observational studies. Acta Diabetol, pp 1–9. https://doi.org/10.1007/s00592-021-01754-2
Biamonte E, Pegoraro F, Carrone F et al (2021) Weight change and glycemic control in type 2 diabetes patients during COVID-19 pandemic: the lockdown effect. Endocrine 72(3):604–610. https://doi.org/10.1007/s12020-021-02739-5
Ruissen MM, Regeer H, Landstra CP, et al (2021) Increased stress, weight gain and less exercise in relation to glycemic control in people with type 1 and type 2 diabetes during the COVID-19 pandemic. BMJ Open Diabetes Res Care 9(1):e002035. https://doi.org/10.1136/bmjdrc-2020-002035
Karatas S, Yesim T, Beysel S (2021) Impact of lockdown COVID-19 on metabolic control in type 2 diabetes mellitus and healthy people. Prim Care Diabetes 15(3):424–427. https://doi.org/10.1016/j.pcd.2021.01.003
Hansel B, Potier L, Chalopin S et al (2021) The COVID-19 lockdown as an opportunity to change lifestyle and body weight in overweight/obesity and diabetes: results from the national French COVIDIAB cohort. Nutrition, Metabolism Cardiovascular Dis. https://doi.org/10.1016/j.numecd.2021.05.031
Farhane H, Motrane M, Anaibar F-E, Motrane A, Abeid SN, Harich N (2021) COVID-19 pandemic: effects of national lockdown on the state of health of patients with type 2 diabetes mellitus in a Moroccan population. Prim Care Diabetes 15(5):772–777. https://doi.org/10.1016/j.pcd.2021.06.007
Khare J, Jindal S (2020) Observational study on effect of lockdown due to COVID 19 on glycemic control in patients with diabetes: experience from central India. Diabetes Metab Syndr 14(6):1571–1574. https://doi.org/10.1016/j.dsx.2020.08.012
Park S-D, Kim S-W, Moon JS et al (2021) Impact of social distancing due to coronavirus disease 2019 on the changes in glycosylated hemoglobin level in people with type 2 diabetes mellitus. Diabetes Metab J 45(1):109–114. https://doi.org/10.4093/dmj.2020.0226
Rastogi A, Hiteshi P, Bhansali A (2020) Improved glycemic control amongst people with long-standing diabetes during COVID-19 lockdown: a prospective, observational, nested cohort study. Int J Diabetes Dev Ctries 40(4):476–481. https://doi.org/10.1007/s13410-020-00880-x
Önmez A, Gamsızkan Z, Özdemir Ş et al (2020) The effect of COVID-19 lockdown on glycemic control in patients with type 2 diabetes mellitus in Turkey. Diabetes Metab Syndr 14(6):1963–1966. https://doi.org/10.1016/j.dsx.2020.10.007
D’Onofrio L, Pieralice S, Maddaloni E et al (2021) Effects of the COVID-19 lockdown on glycaemic control in subjects with type 2 diabetes: the glycalock study. Diabetes Obes Metab. https://doi.org/10.1111/dom.14380
Biancalana E, Parolini F, Mengozzi A, Solini A (2021) Short-term impact of COVID-19 lockdown on metabolic control of patients with well-controlled type 2 diabetes: a single-centre observational study. Acta Diabetol 58(4):431–436. https://doi.org/10.1007/s00592-020-01637-y
Ludwig L, Scheyer N, Remen T, Guerci B (2021) The impact of COVID-19 lockdown on metabolic control and access to healthcare in people with diabetes: The CONFI-DIAB cross-sectional study. Diabetes Ther 12(8):2207–2221. https://doi.org/10.1007/s13300-021-01105-y
Kip KE, Snyder G, Yealy DM, et al (2020) Temporal changes in clinical practice with COVID-19 hospitalized patients: Potential explanations for better in-hospital outcomes. medRxiv. https://doi.org/10.1101/2020.09.29.20203802
Kind AJ, Jencks S, Brock J et al (2014) Neighborhood socioeconomic disadvantage and 30-day rehospitalization: a retrospective cohort study. Ann Intern Med 161(11):765–774. https://doi.org/10.7326/M13-2946
Jensen MD, Ryan DH, Donato KA et al (2014) Executive summary: guidelines (2013) for the management of overweight and obesity in adults. Obesity 22(S2):S5–S39. https://doi.org/10.1002/oby.20821
American Diabetes Association (2010) Standards of medical care in diabetes—2010. Diabetes Care 33(Suppl 1):S11
Wing RR, Venkatakrishnan K, Panza E et al. (2022) Association of COVID-19 stay-at-home orders with 1-year weight changes. JAMA Netw Open 5(6):e2217313–e. https://doi.org/10.1001/jamanetworkopen.2022.17313
Fernandez-Rio J, Cecchini JA, Mendez-Gimenez A, Carriedo A (2020) Weight changes during the COVID-19 home confinement: effects on psychosocial variables. Obes Res Clin Pract 14(4):383–385. https://doi.org/10.1016/j.orcp.2020.07.006
Mulugeta W, Desalegn H, Solomon S (2021) Impact of the COVID‐19 pandemic lockdown on weight status and factors associated with weight gain among adults in Massachusetts. Clin Obes, e12453. https://doi.org/10.1111/cob.12453
Flanagan EW, Beyl RA, Fearnbach SN, Altazan AD, Martin CK, Redman LM (2021) The impact of COVID-19 stay-at-home orders on health behaviors in adults. Obesity 29(2):438–445. https://doi.org/10.1002/oby.23066
Williamson DF, Kahn HS, Remington PL, Anda RF (1990) The 10-year incidence of overweight and major weight gain in US adults. Arch Intern Med 150(3):665–672. https://doi.org/10.1001/archinte.1990.00390150135026
Martín-Timón I, Sevillano-Collantes C, Segura-Galindo A, del Cañizo-Gómez FJ (2014) Type 2 diabetes and cardiovascular disease: have all risk factors the same strength? World J Diabetes 5(4):444. https://doi.org/10.4239/wjd.v5.i4.444
Sherwani SI, Khan HA, Ekhzaimy A et al. (2016) Significance of HbA1c test in diagnosis and prognosis of diabetic patients. Biomark Insights 11:BMI. S38440. https://doi.org/10.4137/BMI.S38440
Gianfrancesco MA, Goldstein ND (2021) A narrative review on the validity of electronic health record-based research in epidemiology. BMC Med Res Methodol 21(1):1–10. https://doi.org/10.1186/s12874-021-01416-5
Anker MS, Landmesser U, von Haehling S, Butler J, Coats AJ, Anker SD (2021) Weight loss, malnutrition, and cachexia in COVID-19: facts and numbers. J Cachexia Sarcopenia Muscle 12(1):9–13
Golden SH, Yajnik C, Phatak S, Hanson RL, Knowler WC (2019) Racial/ethnic differences in the burden of type 2 diabetes over the life course: a focus on the USA and India. Diabetologia 62(10):1751–1760. https://doi.org/10.1007/s00125-019-4968-0
Abedi V, Olulana O, Avula V et al (2021) Racial, economic, and health inequality and COVID-19 infection in the United States. J Racial Ethn Health Disparities 8(3):732–742. https://doi.org/10.1101/2020.04.26.20079756
Acknowledgements
The authors report grants from the National Institute of Diabetes, Digestive, and Kidney Diseases, The National Heart, Lung, and Blood Institute, and the National Institute on Minority Health and Health Disparities (K23MD015092) during the conduct of the study. Dr. Wing reports personal fees from Noom Inc., outside the submitted work.
Author information
Authors and Affiliations
Contributions
EP and RW: concept and design; drafting of manuscript; critical revision of the manuscript for important intellectual content. KK and KV: concept and design; data acquisition and statistical analysis; critical revision of the manuscript for important intellectual content. OM: data acquisition; critical revision of the manuscript for important intellectual content; administrative, technical, or material support.
Corresponding author
Ethics declarations
Conflict of interest
The other authors have no conflicts of interest to declare.
Ethical Standard and Informed consent
Our ethics statement is provided in the “study population” section of the methods. This was not an animal study, so no animal rights disclosure is needed. This was an exempt protocol using de-identified data; it was deemed exempt by our IRB, who approved all study procedures.
Additional information
Managed by Massimo Federici .
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Panza, E., Kip, K.E., Venkatakrishnan, K. et al. Changes in body weight and glycemic control in association with COVID-19 Shutdown among 23,000 adults with type 2 diabetes. Acta Diabetol 60, 787–795 (2023). https://doi.org/10.1007/s00592-023-02056-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-023-02056-5