Abstract
Objective
This study aimed to examine the prevalence of stroke and associated factors of stroke in patients with type 2 diabetes(T2DM) in China.
Methods
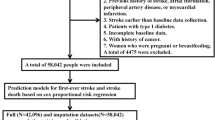
Participants were 18,013 T2DM patients recruited with stratified random cluster sampling method from December 2013 to January 2014 in China. Propensity score matching was used to eliminate confounding effects between groups and logistic regression analysis was used to examine factors associated with stroke among T2DM patients.
Results
Overall, the prevalence of stroke in the subjects with T2DM was 9.5%. After nearest neighbor matching, smoking (OR = 1.60, 95%CI: 1.26–2.03), hypertension (OR = 2.96, 95%CI: 2.55–3.43), dyslipidemia (OR = 2.00, 95%CI: 1.71–2.33), family history of stroke (OR = 2.02, 95%CI: 1.61–2.54), obesity (OR = 1.21, 95%CI: 1.01–1.45) and sleep duration < 6 h/day (OR = 1.44, 95%CI: 1.20–1.73) or > 8 h/day (OR = 1.22, 95%CI: 1.05–1.42) were positively associated with stroke, whereas drinking 1–3 days/week (OR = 0.64, 95%CI: 0.45–0.90) or daily (OR = 0.45, 95%CI: 0.33–0.60), effective exercise (OR = 0.65, 95%CI: 0.57–0.73) and underweight (OR = 0.30, 95%CI: 0.13–0.71) were negatively related to stroke. Besides, the risk of stroke increased substantially with accumulation of above seven modified risk factors. The odds ratio values of stroke in patients having ≥ 5 of the above seven risk factors was 14.39 (95% CI: 8.87–23.26).
Conclusions
The prevalence of stroke was high among T2DM in China. It is of great significance to strengthen comprehensive management of health-related behaviors including smoking cessation, moderate alcohol consumption, effective exercise, 6–8 h of sleep duration, keeping normal weight and the prevention of hypertension and dyslipidemia to have sustained beneficial effects on improvements of stroke risk factors.



Similar content being viewed by others
Data availability
Data supporting the results presented in the paper are available upon reasonable requests.
References
Wang L, Gao P, Zhang M et al (2017) Prevalence and ethnic pattern of diabetes and prediabetes in China in 2013. JAMA 317:2515–2523. https://doi.org/10.1001/jama.2017.7596
Ning GBloomgarden Z, (2013) Diabetes in China: prevalence, diagnosis, and control. J Diabetes 5:372. https://doi.org/10.1111/1753-0407.12088
Al-Rubeaan K, Al-Hussain F, Youssef AM et al (2016) Ischemic stroke and its risk factors in a registry-based large cross-sectional diabetic cohort in a country facing a diabetes epidemic. J Diabetes Res 2016:4132589. https://doi.org/10.1155/2016/4132589
Almobarak AO, Badi S, Elmadhoun WM et al (2020) The prevalence and risk factors of stroke among Sudanese individuals with diabetes: cross-sectional survey. Brain Circ 6:26–30. https://doi.org/10.4103/bc.bc_15_19
Munoz-Rivas N, Mendez-Bailon M, Hernandez-Barrera V et al (2016) Type 2 diabetes and hemorrhagic stroke: a population-based study in Spain from 2003 to 2012. J Stroke Cerebrovasc Dis 25:1431–1443. https://doi.org/10.1016/j.jstrokecerebrovasdis.2016.02.031
Khoury JC, Kleindorfer D, Alwell K et al (2013) Diabetes mellitus: a risk factor for ischemic stroke in a large biracial population. Stroke 44:1500–1504. https://doi.org/10.1161/STROKEAHA.113.001318
Zhang X, Mu Y, Yan W et al (2014) Prevalence of stroke and metabolic disorders in the middle-aged and elderly Chinese with type 2 diabetes. Chin Med J (Engl) 127:3537–3542
Guo L, Yu M, Zhong J et al (2016) Stroke risk among patients with type 2 diabetes mellitus in zhejiang: a population-based prospective study in China. Int J Endocrinol 2016:6380620. https://doi.org/10.1155/2016/6380620
Emerging Risk Factors C, Sarwar N, Gao P et al (2010) Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet 375:2215–2222. https://doi.org/10.1016/S0140-6736(10)60484-9
Low Wang CC, Hess CN, Hiatt WR et al (2016) clinical update: cardiovascular disease in diabetes mellitus: atherosclerotic cardiovascular disease and heart failure in type 2 diabetes mellitus - mechanisms, management, and clinical considerations. Circulation 133:2459–2502. https://doi.org/10.1161/CIRCULATIONAHA.116.022194
Huang Y, Li J, Zhu X et al (2017) Relationship between healthy lifestyle behaviors and cardiovascular risk factors in Chinese patients with type 2 diabetes mellitus: a subanalysis of the CCMR-3B STUDY. Acta Diabetol 54:569–579. https://doi.org/10.1007/s00592-017-0981-2
Feigin VL, Forouzanfar MH, Krishnamurthi R et al (2014) Global and regional burden of stroke during 1990–2010: findings from the global burden of disease study 2010. Lancet 383:245–254. https://doi.org/10.1016/s0140-6736(13)61953-4
Avan A, Digaleh H, Di Napoli M et al (2019) Socioeconomic status and stroke incidence, prevalence, mortality, and worldwide burden: an ecological analysis from the Global Burden of Disease Study 2017. BMC Med 17:191. https://doi.org/10.1186/s12916-019-1397-3
ChangGajasinghe TS, Arambepola C (2015) Prevalence of stroke and its risk factors in Urban Sri Lanka: population-based study. Stroke 46:2965–2968. https://doi.org/10.1161/STROKEAHA.115.010203
Norrving B, Kissela B (2013) The global burden of stroke and need for a continuum of care. Neurology 80:S5-12. https://doi.org/10.1212/WNL.0b013e3182762397
Wang W, Jiang B, Sun H et al (2017) Prevalence, incidence, and mortality of stroke in China: results from a nationwide population-based survey of 480 687 adults. Circulation 135:759–771. https://doi.org/10.1161/CIRCULATIONAHA.116.025250
Xia X, Yue W, Chao B et al (2019) Prevalence and risk factors of stroke in the elderly in Northern China: data from the national stroke screening survey. J Neurol 266:1449–1458. https://doi.org/10.1007/s00415-019-09281-5
Pan B, Jin X, Jun L et al (2019) The relationship between smoking and stroke: a meta-analysis. Medicine (Baltimore) 98:e14872. https://doi.org/10.1097/MD.0000000000014872
MacDonald CJ, Madika AL, Gomes R et al (2021) Physical activity and stroke among women - a non-linear relationship. Prev Med. https://doi.org/10.1016/j.ypmed.2021.106485
Shen Y, Shi L, Nauman E et al (2020) Association between body mass index and stroke risk among patients with type 2 diabetes. J Clin Endocrinol Metab. https://doi.org/10.1210/clinem/dgz032
Lyu Y, Luo Y, Li C et al (2018) Regional Differences in the abetes in China. J Clin Endocrinol Metab 103:3319–3330. https://doi.org/10.1210/jc.2018-00422
Kim MK, Han K, Cho JH et al (2020) A model to predict risk of stroke in middle-aged adults with type 2 diabetes generated from a nationwide population-based cohort study in Korea. Diabetes Res Clin Pract 163:108157. https://doi.org/10.1016/j.diabres.2020.108157
Kim JY, Kang K, Kang J et al (2019) Executive summary of stroke statistics in Korea 2018: a report from the epidemiology research council of the korean stroke society. J Stroke 21:42–59. https://doi.org/10.5853/jos.2018.03125
Yatsuya H, Iso H, Yamagishi K et al (2013) Development of a point-based prediction model for the incidence of total stroke: Japan public health center study. Stroke 44:1295–1302. https://doi.org/10.1161/STROKEAHA.111.677534
Gan Y, Jiang H, Room R et al (2020) Prevalence and risk factors associated with stroke in China: a nationwide survey of 726,451 adults. Eur J Prev Cardiol. https://doi.org/10.1177/2047487320902324
O’Donnell MJ, Chin SL, Rangarajan S et al (2016) Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case-control study. Lancet 388:761–775. https://doi.org/10.1016/S0140-6736(16)30506-2
Li W, Katzmarzyk PT, Horswell R et al (2015) Body mass index and stroke risk among patients with type 2 diabetes mellitus. Stroke 46:164–169. https://doi.org/10.1161/STROKEAHA.114.006718
Sone H, Tanaka S, Tanaka S et al (2013) Leisure-time physical activity is a significant predictor of stroke and total mortality in Japanese patients with type 2 diabetes: analysis from the Japan Diabetes Complications Study (JDCS). Diabetologia 56:1021–1030. https://doi.org/10.1007/s00125-012-2810-z
Hankey GJ, Anderson NE, Ting RD et al (2013) Rates and predictors of risk of stroke and its subtypes in diabetes: a prospective observational study. J Neurol Neurosurg Psychiatry 84:281–287. https://doi.org/10.1136/jnnp-2012-303365
Kiss Z, Rokszin G, Abonyi-Toth Z et al (2019) Different changes of risks for stroke and myocardial infarction in patients with type 2 diabetes in hungary between the two periods of 2001–2004 and 2010–2013. Front Endocrinol (Lausanne) 10:170. https://doi.org/10.3389/fendo.2019.00170
Wafa HA, Wolfe CDA, Emmett E et al (2020) Burden of stroke in Europe: thirty-year projections of incidence, prevalence, deaths, and disability-adjusted life years. Stroke 51:2418–2427. https://doi.org/10.1161/STROKEAHA.120.029606
Li Q, Wu H, Yue W et al (2017) Prevalence of stroke and vascular risk factors in china: a nationwide community-based study. Sci Rep 7:6402. https://doi.org/10.1038/s41598-017-06691-1
American Diabetes A (2013) Diagnosis and classification of diabetes mellitus. Diabetes Care 36(Suppl 1):S67-74. https://doi.org/10.2337/dc13-S067
Yang L, Yan J, Tang X et al (2016) Prevalence, awareness, treatment, control and risk factors associated with hypertension among adults in Southern China, 2013. PLoS ONE 11:e0146181. https://doi.org/10.1371/journal.pone.0146181
Liu J, Ren ZH, Qiang H et al (2020) Trends in the incidence of diabetes mellitus: results from the global burden of disease study 2017 and implications for diabetes mellitus prevention. BMC Public Health 20:1415. https://doi.org/10.1186/s12889-020-09502-x
Tan KW, Dickens BS, LCook AR (2020) Projected burden of type 2 diabetes mellitus-related complications in Singapore until 2050: a Bayesian evidence synthesis. BMJ Open Diabetes Res Care. https://doi.org/10.1136/bmjdrc-2019-000928
Katan MLuft A (2018) Global burden of stroke. Semin Neurol 38:208–211. https://doi.org/10.1055/s-0038-1649503
Guo J, Guan T, Shen Y et al (2018) Lifestyle factors and gender-specific risk of stroke in adults with diabetes mellitus: a case-control study. J Stroke Cerebrovasc Dis 27:1852–1860. https://doi.org/10.1016/j.jstrokecerebrovasdis.2018.02.022
Rissanen I, Oura P, Paananen M et al (2019) Smoking trajectories and risk of stroke until age of 50 years - The Northern Finland Birth Cohort 1966. PLoS ONE 14:e0225909. https://doi.org/10.1371/journal.pone.0225909
Yang D, Bian Y, Zeng Z et al (2020) Associations between intensity, frequency, duration, and volume of physical activity and the risk of stroke in middle- and older-aged chinese people: a cross-sectional study. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph17228628
Wu Q, Tang AJ, Zeng L et al (2021) Prognosis of neurological improvement in inpatient acute ischemic stroke survivors: a propensity score matching analysis. J Stroke Cerebrovasc Dis 30:105437. https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.105437
Al Rifai M, DeFilippis AP, McEvoy JW et al (2017) The relationship between smoking intensity and subclinical cardiovascular injury: the Multi-Ethnic Study of Atherosclerosis (MESA). Atherosclerosis 258:119–130. https://doi.org/10.1016/j.atherosclerosis.2017.01.021
Writing Group M, Mozaffarian D, Benjamin EJ et al (2016) Heart disease and stroke statistics-2016 update: a report from the American heart association. Circulation 133:e38-360. https://doi.org/10.1161/CIR.0000000000000350
Zhang X, Shu L, Si C et al (2015) Dietary patterns and risk of stroke in adults: a systematic review and meta-analysis of prospective cohort studies. J Stroke Cerebrovasc Dis 24:2173–2182. https://doi.org/10.1016/j.jstrokecerebrovasdis.2015.05.035
Larsson SC, Wallin A, Wolk A et al (2016) Differing association of alcohol consumption with different stroke types: a systematic review and meta-analysis. BMC Med 14:178. https://doi.org/10.1186/s12916-016-0721-4
Bardach AE, Caporale JE, Rubinstein AL et al (2017) Impact of level and patterns of alcohol drinking on coronary heart disease and stroke burden in Argentina. PLoS ONE 12:e0173704. https://doi.org/10.1371/journal.pone.0173704
Wakabayashi I (2011) Association between alcohol drinking and metabolic syndrome in Japanese male workers with diabetes mellitus. J Atheroscler Thromb 18:684–692. https://doi.org/10.5551/jat.7435
Rogers AJ, Kaplan I, Chung A et al (2020) obstructive sleep apnea risk and stroke among blacks with metabolic syndrome: results from metabolic syndrome outcome (MetSO) registry. Int J Clin Res Trials. https://doi.org/10.15344/2456-8007/2020/143
DeBoer MD, Filipp SL, Sims M et al (2020) Risk of ischemic stroke increases over the spectrum of metabolic syndrome severity. Stroke 51:2548–2552. https://doi.org/10.1161/STROKEAHA.120.028944
Fernandez-Sola J (2015) Cardiovascular risks and benefits of moderate and heavy alcohol consumption. Nat Rev Cardiol 12:576–587. https://doi.org/10.1038/nrcardio.2015.91
Stephan LS, Almeida ED, Markoski MM et al (2017) Red wine, resveratrol and atrial fibrillation. Nutrients. https://doi.org/10.3390/nu9111190
de Gaetano G, Costanzo S, Di Castelnuovo A et al (2016) Effects of moderate beer consumption on health and disease: a consensus document. Nutr Metab Cardiovasc Dis 26:443–467. https://doi.org/10.1016/j.numecd.2016.03.007
Schreuder TH, Maessen MF, Tack CJ et al (2014) Life-long physical activity restores metabolic and cardiovascular function in type 2 diabetes. Eur J Appl Physiol 114:619–627. https://doi.org/10.1007/s00421-013-2794-5
Soares-Miranda L, Siscovick DS, Psaty BM et al (2016) Physical activity and risk of coronary heart disease and stroke in older adults: the cardiovascular health study. Circulation 133:147–155. https://doi.org/10.1161/CIRCULATIONAHA.115.018323
Li W, Kondracki A, Gautam P et al (2020) The association between sleep duration, napping, and stroke stratified by self-health status among Chinese people over 65 years old from the China health and retirement longitudinal study. Sleep Breath. https://doi.org/10.1007/s11325-020-02214-x
Ji A, Lou H, Lou P et al (2020) Interactive effect of sleep duration and sleep quality on risk of stroke: an 8-year follow-up study in China. Sci Rep 10:8690. https://doi.org/10.1038/s41598-020-65611-y
He Q, Sun H, Wu X et al (2017) Sleep duration and risk of stroke: a dose-response meta-analysis of prospective cohort studies. Sleep Med 32:66–74. https://doi.org/10.1016/j.sleep.2016.12.012
Akinseye OA, Ojike NI, Akinseye LI et al (2016) Association of sleep duration with stroke in diabetic patients: analysis of the national health interview survey. J Stroke Cerebrovasc Dis 25:650–655. https://doi.org/10.1016/j.jstrokecerebrovasdis.2015.11.023
Ali I, Abuissa M, Alawneh A et al (2019) The prevalence of dyslipidemia and hyperglycemia among stroke patients: preliminary findings. Stroke Res Treat 2019:8194960. https://doi.org/10.1155/2019/8194960
AlloubaniSaleh AAbdelhafiz AI (2018) Hypertension and diabetes mellitus as a predictive risk factors for stroke. Diabetes Metab Syndr 12:577–584. https://doi.org/10.1016/j.dsx.2018.03.009
Chen R, Ovbiagele B, Feng W (2016) Diabetes and stroke: epidemiology, pathophysiology, pharmaceuticals and outcomes. Am J Med Sci 351:380–386. https://doi.org/10.1016/j.amjms.2016.01.011
Akinyemi RO, Ovbiagele B, Akpalu A et al (2015) Stroke genomics in people of African ancestry: charting new paths. Cardiovasc J Afr 26:S39-49. https://doi.org/10.5830/CVJA-2015-039
Pourasgari M, Mohamadkhani A (2020) Heritability for stroke: Essential for taking family history. Caspian J Intern Med 11:237–243. https://doi.org/10.22088/cjim.11.3.237
Larsson SC, Akesson AWolk A, (2014) Healthy diet and lifestyle and risk of stroke in a prospective cohort of women. Neurology 83:1699–1704. https://doi.org/10.1212/WNL.0000000000000954
Rist PM, Buring JE, Kase CS et al (2016) Healthy lifestyle and functional outcomes from stroke in women. Am J Med 129(715–724):e2. https://doi.org/10.1016/j.amjmed.2016.02.002
Tian X, Du H, Li L et al (2017) Fruit consumption and physical activity in relation to all-cause and cardiovascular mortality among 70,000 Chinese adults with pre-existing vascular disease. PLoS ONE 12:e0173054. https://doi.org/10.1371/journal.pone.0173054
Acknowledgements
The authors would like to thank all the participants involved in the survey. The authors would also like to thank the Huai´an Center for Disease Control and Prevention.
Funding
This work was supported by the National Natural Science Foundation of China [grant number [82003484] and Universities' philosophy and social science researches in Jiangsu Province [2020SJA1053], Natural Science Foundation for Colleges Universities in Jiangsu Province [20KJB330005].
Author information
Authors and Affiliations
Contributions
Wei Wang and Xunbao Zhang involved in conceptualization and methodology; Chenlu He participated in data curation and writing—original draft preparation; Peian Lou, Zhongming Sun and Enchun Pan supervised and validated the study; Wei Wang participated in writing—reviewing and editing.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflict competing interests.
Ethical approval
Approval was obtained from the ethics committee of the Huai´an Center for Disease Control and Prevention and Xuzhou Medical University. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Informed consent
All participants gave their written informed consent before their inclusion in the study.
Additional information
Managed By Massimo Porta.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
He, C., Wang, W., Chen, Q. et al. Factors associated with stroke among patients with type 2 diabetes mellitus in China: a propensity score matched study. Acta Diabetol 58, 1513–1523 (2021). https://doi.org/10.1007/s00592-021-01758-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-021-01758-y