Abstract
Background
Stroke is one of the leading causes of disability and mortality in patients with type 2 diabetes mellitus (T2DM). Risk models have been developed for predicting stroke and stroke-associated mortality among patients with T2DM. Here, we evaluated risk factors of stroke for individualized prevention measures in patients with T2DM in northern China.
Methods
In the community-based Tianjin Chronic Disease Cohort study, 58,042 patients were enrolled between January 2014 and December 2019. We used multiple imputation (MI) to impute missing variables and univariate and multivariate Cox’s proportional hazard regression to screen risk factors of stroke. Furthermore, we established and validated first-ever prediction models for stroke (Model 1 and Model 2) and death from stroke (Model 3) and evaluated their performance.
Results
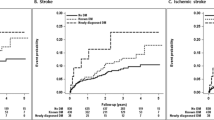
In the derivation and validation groups, the area under the curves (AUCs) of Models 1–3 was better at 5 years than at 8 years. The Harrell’s C-index for all models was above 0.7. All models had good calibration, discrimination, and clinical net benefit. Sensitivity analysis using the MI dataset indicated that all models had good and stable prediction performance.
Conclusion
In this study, we developed and validated first-ever risk prediction models for stroke and death from stroke in patients with T2DM, with good discrimination and calibration observed in all models. Based on lifestyle, demographic characteristics, and laboratory examination, these models could provide multidimensional management and individualized risk assessment. However, the models developed here may only be applicable to Han Chinese.




Similar content being viewed by others
Data availability
The raw data are not available. However, the data are available from the corresponding author upon reasonable individual request.
Code availability
Not applicable.
References
Rao Kondapally Seshasai S, Kaptoge S, Thompson A et al (2011) Diabetes mellitus, fasting glucose, and risk of cause-specific death. N Engl J Med 364:829–841. https://doi.org/10.1056/NEJMoa1008862
Chatterjee S, Khunti K, Davies MJ (2017) Type 2 diabetes. Lancet 389:2239–2251. https://doi.org/10.1016/s0140-6736(17)30058-2
Turin TC, Okamura T, Rumana N et al (2017) Diabetes and lifetime risk of stroke and subtypes in an urban middle-aged population. J Diabetes Complications 31:831–835. https://doi.org/10.1016/j.jdiacomp.2017.02.002
Feigin VL, Nguyen G, Cercy K et al (2018) Global, regional, and country-specific lifetime risks of stroke, 1990 and 2016. N Engl J Med 379:2429–2437. https://doi.org/10.1056/NEJMoa1804492
IDF (2019) IDF Diabetes Atlas, 9th edn. https://www.diabetesatlas.org/en/. Accessed 2 Dec 2020
O’Donnell MJ, Chin SL, Rangarajan S et al (2016) Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case-control study. Lancet 388:761–775. https://doi.org/10.1016/s0140-6736(16)30506-2
Bragg F, Holmes MV, Iona A et al (2017) Association between diabetes and cause-specific mortality in rural and urban areas of China. JAMA 317:280–289. https://doi.org/10.1001/jama.2016.19720
Emerging Risk Factors C, Sarwar N, Gao P et al (2010) Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet 375:2215–2222. https://doi.org/10.1016/S0140-6736(10)60484-9
Benjamin EJ, Muntner P, Alonso A et al (2019) Heart disease and stroke statistics-2019 update: a report from the American Heart Association. Circulation 139:e56–e528. https://doi.org/10.1161/CIR.0000000000000659
van Sloten TT, Sedaghat S, Carnethon MR et al (2020) Cerebral microvascular complications of type 2 diabetes: stroke, cognitive dysfunction, and depression. Lancet Diabetes Endocrinol 8:325–336. https://doi.org/10.1016/s2213-8587(19)30405-x
Collaborators GDaI (2020) Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396:1204–1222. https://doi.org/10.1016/S0140-6736(20)30925-9
Zhou M, Wang H, Zeng X et al (2019) Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 394:1145–1158. https://doi.org/10.1016/S0140-6736(19)30427-1
Stitziel NO, Kanter JE, Bornfeldt KE (2020) Emerging targets for cardiovascular disease prevention in diabetes. Trends Mol Med 26:744–757. https://doi.org/10.1016/j.molmed.2020.03.011
Jia X, Al Rifai M, Liu J et al (2020) Highlights of studies in cardiovascular disease prevention presented at the 2020 American college of cardiology annual scientific session. Curr Atheroscler Rep 22:32. https://doi.org/10.1007/s11883-020-00856-6
Arnett DK, Blumenthal RS, Albert MA et al (2019) 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: executive summary: a report of the American college of cardiology/American heart association task force on clinical practice guidelines. Circulation 140:e563–e595. https://doi.org/10.1161/CIR.0000000000000677
Kothari V, Stevens RJ, Adler AI et al (2002) UKPDS 60: risk of stroke in type 2 diabetes estimated by the UK Prospective Diabetes Study risk engine. Stroke 33:1776–1781. https://doi.org/10.1161/01.str.0000020091.07144.c7
Hippisley-Cox J, Coupland C, Vinogradova Y et al (2007) Derivation and validation of QRISK, a new cardiovascular disease risk score for the United Kingdom: prospective open cohort study. BMJ 335:136. https://doi.org/10.1136/bmj.39261.471806.55
Basu S, Sussman JB, Berkowitz SA et al (2017) Development and validation of risk equations for complications of type 2 diabetes (RECODe) using individual participant data from randomised trials. Lancet Diabetes Endocrinol 5:788–798. https://doi.org/10.1016/s2213-8587(17)30221-8
Yang X, So WY, Kong AP et al (2007) Development and validation of stroke risk equation for Hong Kong Chinese patients with type 2 diabetes: the Hong Kong Diabetes Registry. Diabetes Care 30:65–70. https://doi.org/10.2337/dc06-1273
Tanaka S, Tanaka S, Iimuro S et al (2013) Predicting macro- and microvascular complications in type 2 diabetes: the Japan Diabetes Complications Study/the Japanese Elderly Diabetes Intervention Trial risk engine. Diabetes Care 36:1193–1199. https://doi.org/10.2337/dc12-0958
Li TC, Wang HC, Li CI et al (2018) Establishment and validation of a prediction model for ischemic stroke risks in patients with type 2 diabetes. Diabetes Res Clin Pract 138:220–228. https://doi.org/10.1016/j.diabres.2018.01.034
Alberti KG, Zimmet PZ (1998) Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med 15:539–553. https://doi.org/10.1002/(SICI)1096-9136(199807)15:7%3c539::AID-DIA668%3e3.0.CO;2-S
Sacco RL, Kasner SE, Broderick JP et al (2013) An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 44:2064–2089. https://doi.org/10.1161/STR.0b013e318296aeca
Wilches JP, Fernandez-Mercado J, De la Hoz-Restrepo F et al (2018) Dissimilar impact of type 2 diabetes on cardiovascular outcomes according to age categories: a nationwide population study from Hungary. BMC Cardiovasc Disord 17:107. https://doi.org/10.1186/s12872-018-0993-z
Furukawa Y, Kokubo Y, Okamura T et al (2010) The relationship between waist circumference and the risk of stroke and myocardial infarction in a Japanese urban cohort: the Suita study. Stroke 41:550–553. https://doi.org/10.1161/STROKEAHA.109.569145
Cho JH, Rhee EJ, Park SE et al (2019) The risk of myocardial infarction and ischemic stroke according to waist circumference in 21,749,261 Korean adults: a nationwide population-based study. Diabetes Metab J 43:206–221. https://doi.org/10.4093/dmj.2018.0039
Zhang F, Liu L, Zhang C et al (2021) Association of metabolic syndrome and its components with risk of stroke recurrence and mortality: a meta-analysis. Neurology 97:e695–e705. https://doi.org/10.1212/WNL.0000000000012415
Komi R, Tanaka F, Omama S et al (2018) Burden of high blood pressure as a contributing factor to stroke in the Japanese community-based diabetic population. Hypertens Res 41:531–538. https://doi.org/10.1016/j.diabres.2019.03.014 (10.1038/s41440-018-0042-4)
Adamsson Eryd S, Gudbjörnsdottir S, Manhem K et al (2016) Blood pressure and complications in individuals with type 2 diabetes and no previous cardiovascular disease: national population based cohort study. BMJ 354:i4070. https://doi.org/10.1136/bmj.i4070
Yi SW, Shin DH, Kim H et al (2018) Total cholesterol and stroke mortality in middle-aged and elderly adults: a prospective cohort study. Atherosclerosis 270:211–217. https://doi.org/10.1016/j.atherosclerosis.2017.12.003
Wang A, Li H, Yuan J et al (2020) Visit-to-visit variability of lipids measurements and the risk of stroke and stroke types: a prospective cohort study. J Stroke 22:119–129. https://doi.org/10.5853/jos.2019.02075
Noh M, Kwon H, Jung CH et al (2017) Impact of diabetes duration and degree of carotid artery stenosis on major adverse cardiovascular events: a single-center, retrospective, observational cohort study. Cardiovasc Diabetol 16:74. https://doi.org/10.1186/s12933-017-0556-0
Tang O, Matsushita K, Coresh J et al (2020) Mortality implications of prediabetes and diabetes in older adults. Diabetes Care 43:382–388. https://doi.org/10.2337/dc19-1221
Young JB, Gauthier-Loiselle M (2018) Development of predictive risk models for major adverse cardiovascular events among patients with type 2 diabetes mellitus using health insurance claims data. Cardiovasc Diabetol 17:118. https://doi.org/10.1186/s12933-018-0759-z
Piniés JA, González-Carril F, Arteagoitia JM et al (2014) Development of a prediction model for fatal and non-fatal coronary heart disease and cardiovascular disease in patients with newly diagnosed type 2 diabetes mellitus: the Basque Country Prospective Complications and Mortality Study risk engine (BASCORE). Diabetologia 57:2324–2333. https://doi.org/10.1007/s00125-014-3370-1
Hu WS, Lin CL (2018) Use of the progression of adapted Diabetes Complications Severity Index to predict acute coronary syndrome, ischemic stroke, and mortality in Asian patients with type 2 diabetes mellitus: a nationwide cohort investigation. Clin Cardiol 41:1038–1043. https://doi.org/10.1016/j.clnu.2017.01.012 (10.1002/clc.22991)
Eastman RC, Javitt JC, Herman WH et al (1997) Model of complications of NIDDM. I. Model construction and assumptions. Diabetes Care 20:725–734. https://doi.org/10.2337/diacare.20.5.725
Bergemann R, Hauner H, Morris AD et al (2006) Prediction of acute and chronic complications by a new computer simulation model for type 1 and type 2 diabetes: the Diabetes Mellitus Model (DMM). J Med Econ 9:83–99
Tao L, Wilson EC, Griffin SJ et al (2013) Performance of the UKPDS outcomes model for prediction of myocardial infarction and stroke in the ADDITION-Europe trial cohort. Value Health 16:1074–1080. https://doi.org/10.1016/j.jval.2013.06.001
Bannister CA, Poole CD, Jenkins-Jones S et al (2014) External validation of the UKPDS risk engine in incident type 2 diabetes: a need for new type 2 diabetes-specific risk equations. Cardiovasc Diabetol 37:537–545. https://doi.org/10.1186/s12933-018-0664-5 (10.2337/dc13-1159)
Davis WA, Knuiman MW, Davis TM (2010) An Australian cardiovascular risk equation for type 2 diabetes: the Fremantle Diabetes Study. Intern Med J 40:286–292. https://doi.org/10.1111/j.1445-5994.2009.01958.x
Campbell PT, Newton CC, Patel AV et al (2012) Diabetes and cause-specific mortality in a prospective cohort of one million U.S. adults. Diabetes Care 35:1835–1844. https://doi.org/10.2337/dc12-0002
Woodward M, Zhang X, Barzi F et al (2003) The effects of diabetes on the risks of major cardiovascular diseases and death in the Asia-Pacific region. Diabetes Care 26:360–366. https://doi.org/10.2337/diacare.26.2.360
Yang X, Li J, Hu D et al (2016) Predicting the 10-year risks of atherosclerotic cardiovascular disease in Chinese population: the China-PAR project (Prediction for ASCVD Risk in China). Circulation 134:1430–1440. https://doi.org/10.1161/circulationaha.116.022367
Liu F, Li J, Chen J et al (2018) Predicting lifetime risk for developing atherosclerotic cardiovascular disease in Chinese population: the China-PAR project. Sci Bull 63:779–787. https://doi.org/10.1016/j.scib.2018.05.020
Silventoinen K, Pankow J, Lindström J et al (2005) The validity of the Finnish Diabetes Risk Score for the prediction of the incidence of coronary heart disease and stroke, and total mortality. Eur J Cardiovasc Prev Rehabil 12:451–458. https://doi.org/10.1097/01.hjr.0000174793.31812.21
Davis WA, Hellbusch V, Hunter ML et al (2020) Contemporary cardiovascular risk assessment for type 2 diabetes including heart failure as an outcome: the Fremantle diabetes study phase ii. J Clin Med. https://doi.org/10.3390/jcm9051428
Wong KS, Mok V, Lam WW et al (2000) Aspirin-associated intracerebral hemorrhage: clinical and radiologic features. Neurology 54:2298–2301. https://doi.org/10.1212/wnl.54.12.2298
Zinman B, Wanner C, Lachin JM et al (2015) Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med 373:2117–2128. https://doi.org/10.1056/NEJMoa1504720
Elisabetta Patorno AP, Bessette LG, Kim DH, Dave C, Glynn RJ, Munshi MN, Schneeweiss S, Wexler DJ, Kim SC (2021) Comparative effectiveness and safety of sodium-glucose cotransporter 2 inhibitors versus glucagon-like peptide 1 receptor agonists in older adults. Diabetes Care 44:826–835. https://doi.org/10.2337/dc20-1464
Acknowledgements
The authors thank the staff and participants of the study for their indispensable contributions.
Funding
This study was funded by the financial support from the National Natural Science Foundation of China (no.91746205), Open Project of Tianjin Key Laboratory of Metabolic Diseases (ZXY-ZDSYSZD2021-1), Tianjin Science and Technology Plan Project Public Health Science and Technology Major Special Project (No.21ZXGWSY00100), and Tianjin Key Medical Discipline (Specialty) Construct Project (No.TJYXZDXK-032A). The funder (Prof. Pei Yu) designed this study and was not for profit.
Author information
Authors and Affiliations
Contributions
XS, HYL, and FH contributed equally to this study. XS prepared the figures and wrote the manuscript. PY designed this study; YL, XJ, PFB, YRZ, CLL, HL, and FH recorded and prepared the data; XS, HYL, and FH analyzed the data and interpreted the results of the study; SJZ, FH, and YB edited and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
The study was reviewed and approved by the ethics committee of Tianjin Chu Hsien-l Memorial Hospital. The study was registered in the Chinese Clinical Trial Register with the identification number ChiCTR1900023701 (2019/06/08).
Research involving human participants and/or animals
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Verbal informed consent was obtained from each participant and was recorded by the physician who explained the study procedures.
Consent for publication
Written informed consent for publication was obtained from all participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shao, X., Liu, H., Hou, F. et al. Development and validation of risk prediction models for stroke and mortality among patients with type 2 diabetes in northern China. J Endocrinol Invest 46, 271–283 (2023). https://doi.org/10.1007/s40618-022-01898-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-022-01898-0