Abstract
Purpose
Preoperative digital planning of total hip arthroplasty (THA) anticipates difficulties while increasing implant survival. The objective was to establish the learning curve to produce a reliable and reproducible preoperative planning for THA. We hypothesize that a learning curve exists for planning, and we want to determine the number of procedures required to accomplish it.
Methods
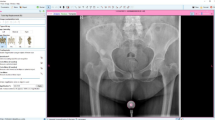
This prospective study included patients for THA from 02/11/2019 to 01/11/2022. Ten junior (Juniors) and senior surgeons (Seniors) had received dedicated training in the use of the software. Modeling was done blindly by Juniors and Senior before surgery on a standardized front pelvis X-ray (mediCAD 2D Classic Hospital software). Statistical analyses to establish the learning curve were done to compare the Juniors and Seniors.
Results
60% of the Juniors achieved competence after 31.5 ± 12.9 [14–54] planning sessions for the acetabular implant, and 80% after 30.3 ± 8.3 [17–40] planning sessions for the femoral implant. Femoral neck size was achieved by all ten Juniors after 23.1 ± 6.8 [17–38] planning. The offset was correctly restored on the plan by 30% of the Juniors after 33.5 ± 11.6 [18–46] planning.
Conclusion
There is a learning curve for 2D planning of uncemented THA. The different planning items seem to have different learning curves. Compared to Seniors, the completion of 75 planning sessions is not sufficient in totality. The competence of the Juniors for the acetabular implant, the length of the neck and the size of the femoral stem are mostly acquired before 75 sessions.
Level of evidence
Prospective study—Level II.



Similar content being viewed by others
References
Learmonth ID, Young C, Rorabeck C (2007) The operation of the century: total hip replacement. The Lancet 370:1508–1519. https://doi.org/10.1016/S0140-6736(07)60457-7
Maitama Implant factors that might influence components’ survival in primary total hip arthroplasty. https://www.npmj.org/article.asp?issn=1117-1936;year=2022;volume=29;issue=1;spage=1;epage=5;aulast=Maitama. Accessed 8 Jan 2023
Viricel C, Boyer B, Philippot R et al (2022) Survie et complications des prothèses totales de hanche à double mobilité de troisième génération avec du polyéthylène non réticulé chez des patients de moins de 55 ans. Rev Chir Orthopédique Traumatol 108:161–168. https://doi.org/10.1016/j.rcot.2022.01.011
Thirion T, Georis P, Gillet P (2019) Preoperative planning interest of a total hip prosthesis. Rev Med Liege 74:593–597
Knight JL, Atwater RD (1992) Preoperative planning for total hip arthroplasty. Quantitating its utility and precision. J Arthroplasty 7:403–409. https://doi.org/10.1016/s0883-5403(07)80031-3
Eggli S, Pisan M, Müller ME (1998) The value of preoperative planning for total hip arthroplasty. J Bone Joint Surg Br 80-B:382–390. https://doi.org/10.1302/0301-620X.80B3.0800382
Davila JA, Kransdorf MJ, Duffy GP (2006) Surgical planning of total hip arthroplasty: accuracy of computer-assisted EndoMap software in predicting component size. Skeletal Radiol 35:390–393. https://doi.org/10.1007/s00256-006-0106-4
Wright TP (1936) Factors affecting the cost of airplanes. J Aeronaut Sci 3:122–128. https://doi.org/10.2514/8.155
Carter LW, Stovall DO, Young TR (1995) Determination of accuracy of preoperative templating of noncemented femoral prostheses. J Arthroplasty 10:507–513. https://doi.org/10.1016/S0883-5403(05)80153-6
Franken M, Grimm B, Heyligers I (2010) A comparison of four systems for calibration when templating for total hip replacement with digital radiography. J Bone Joint Surg Br 92-B:136–141. https://doi.org/10.1302/0301-620X.92B1.22257
Sinclair VF, Wilson J, Jain NPM, Knowles D (2014) Assessment of accuracy of marker ball placement in pre-operative templating for total hip arthroplasty. J Arthroplasty 29:1658–1660. https://doi.org/10.1016/j.arth.2014.03.013
Charnley J (1979) Low friction arthroplasty of the hip: theory and practice. Springer-Verlag, Berlin
Jung S, Neuerburg C, Kappe T et al (2012) Validity of digital templating in total hip arthroplasty: impact of stem design and planner’s experience. Z Orthopadie Unfallchirurgie 150:404–408. https://doi.org/10.1055/s-0031-1298386
Turgay EF, El Zayat BF, Heyse TJ, Timmesfeld N, Fuchs-Winkelmann S, Schmitt J (2011) Precision of preoperative digital templating in total hip arthroplasty. Acta orthopaedica Belgica 77:616–21
Della Valle AG, Padgett DE, Salvati EA (2005) Preoperative planning for primary total hip arthroplasty. J Am Acad Orthop Surg 13:455–462. https://doi.org/10.5435/00124635-200511000-00005
Mittag F, Ipach I, Schaefer R et al (2012) Predictive value of preoperative digital templating in THA depends on the surgical experience of the performing physician. Orthopedics 35:e144-147. https://doi.org/10.3928/01477447-20120123-14
Dammerer D, Keiler A, Herrnegger S et al (2021) Accuracy of digital templating of uncemented total hip arthroplasty at a certified arthroplasty center: a retrospective comparative study. Arch Orthop Trauma Surg 142:2471–2480. https://doi.org/10.1007/s00402-021-03836-w
Kearney R, Shaikh AH, O’Byrne JM (2013) The accuracy and inter-observer reliability of acetate templating in total hip arthroplasty. Ir J Med Sci 182:409–414. https://doi.org/10.1007/s11845-013-0901-6
Thirion T, Georis P, Szecel Z, Gillet P (2020) Preoperative planning of total hip arthroplasty. Must this essential part of the procedure be necessarily performed by the orthopedic surgeon? A prospective study about 100 Corail® Hip System. Acta Orthop Belg 86:644–649
Waldstein W, Bouché PA, Pottmann C et al (2021) Quantitative and individualized assessment of the learning curve in preoperative planning of the acetabular cup size in primary total hip arthroplasty. Arch Orthop Trauma Surg 141:1601–1608. https://doi.org/10.1007/s00402-021-03848-6
Biau DJ, Meziane M, Bhumbra RS et al (2011) Monitoring the quality of total hip replacement in a tertiary care department using a cumulative summation statistical method (CUSUM). J Bone Joint Surg Br 93:1183–1188. https://doi.org/10.1302/0301-620X.93B9.26436
Bertz A, Indrekvam K, Ahmed M et al (2012) Validity and reliability of preoperative templating in total hip arthroplasty using a digital templating system. Skeletal Radiol 41:1245–1249. https://doi.org/10.1007/s00256-012-1431-4
Sershon RA, Diaz A, Bohl DD, Levine BR (2017) Effect of body mass index on digital templating for total hip arthroplasty. J Arthroplasty 32:1024–1026. https://doi.org/10.1016/j.arth.2016.09.020
González Della Valle A, Comba F, Taveras N, Salvati EA (2008) The utility and precision of analogue and digital preoperative planning for total hip arthroplasty. Int Orthop 32:289–294. https://doi.org/10.1007/s00264-006-0317-2
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cypel, S., Bouche, PA., Heliere, G. et al. Junior surgeon learning curve for performing digital planning of a first-line uncemented total hip prothesis. Eur J Orthop Surg Traumatol (2024). https://doi.org/10.1007/s00590-024-03986-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00590-024-03986-8