Abstract
Purpose
Major orthopedic surgeries of the lower extremities, which heavily injure the metaphyseal region, are strongly associated with the risk of developing deep vein thrombosis (DVT). This study aims to investigate the role of metaphyseal trauma as an independent risk factor for DVT.
Methods
Patients undergoing major orthopedic surgery of the hip and knee had their existing DVT risk factors recorded. Metaphyseal trauma was defined by the extent of bone injury during these surgeries. The samples were categorized into three surgery groups: total arthroplasty group (TA), hemiarthroplasty group (HA), and the open reduction internal fixation group (ORIF). Logistic regression test between significant existing risk factors and surgery groups determines the independent association between risk factors and DVT.
Result
The study found a 24.8% incidence of asymptomatic DVT in patients undergoing major orthopedic surgeries, with the highest prevalence (37.2%) in TA, which had the largest extent of metaphyseal trauma and the least existing DVT risk factors. TA showed 6.2 OR and 95% CI (p = 0.036) compared to the other existing risk factor in relation to DVT incidence.
Conclusion
Metaphyseal bone trauma in the hip and knee major orthopedic surgery is an independent risk factor for deep vein thrombosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Deep vein thrombosis (DVT) is a blood clot that forms within the deep veins, most commonly in the lower limbs with clot formation originating in a deep calf vein propagating proximally [1]. As a part of venous thromboembolism (VTE) disorder, DVT represents the third most common mortality cause of cardiovascular disease due to pulmonary embolism. DVT occurs frequently as a postoperative complication, particularly after major lower limb orthopedic surgeries, a risk recognized previously by the American College of Chest Physicians (ACCP) and the American Academy of Orthopaedic Surgeon (AAOS) [2, 3].
Hip arthroplasty, knee arthroplasty, as well as hip or knee fracture surgeries are strongly associated with a risk of developing DVT [2, 4,5,6]. These surgeries primarily injured the metaphyseal region of the lower extremities bone [7]. The amount of endothelial damage in a heavily vascularized structure injury as in metaphyseal trauma increases the risk of DVT. Endothelial damage is one of the factors in Virchow’s triad (1856). In contrast, in cases of acute trauma in the diaphysis involving long bone such as a fracture of midshaft femur, fat emboli are more likely to occur due to the intravasation of bone marrow fat [8, 9].
Despite numerous studies on potential risk factors for DVT, there has been no published research on the impact of metaphyseal trauma as a risk factor for DVT. Therefore, the primary objective of this study was to analyze metaphyseal trauma as a potential risk factor for DVT. We hypothesize that trauma to the metaphyseal cancellous bone in the lower extremities is an independent risk factor for DVT after major lower orthopedic surgery.
Methods
An observational prospective cohort was conducted during a 28-month period from 2008 to 2011. Inclusion criteria were patients aged above 50 years old and who were admitted to the hospital for major hip and knee surgery without chemical or mechanical thromboprophylaxis. The major lower orthopedic surgeries included were total knee arthroplasty (TKA), total hip arthroplasty (THA), hip hemiarthroplasty (HHA), as well as proximal and distal femur fixation (FF). All surgical procedures were performed by a single senior orthopedic surgeon in two private hospitals. Exclusion criteria were total paralysis patients, patients with central vein catheter, patients under estrogen treatment, post major operation patients within the last 3 months, patients with previous DVT or other rare conditions such as nephrotic syndrome, and inflammatory bowel disease.
All patients were hospitalized on an average of 8 to 12 days. Ambulatory observation was conducted for up to 30 postoperative days. Any anticoagulant treatments were stopped one week before the surgical procedures. DVT was confirmed as positive by venography or alternative USG color Doppler on the 7th to 8th postoperative day defined by fresh thrombus in the deep vein of the lower extremity. Patients with confirmed positive DVT were treated with an oral anticoagulant.
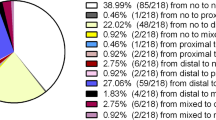
Metaphyseal trauma was defined by the extent of bone injury during major hip and knee surgery. Although this area can certainly vary, we estimate the area of bony trauma by calculating the implant surface area of THA, TKA, and HHA. In cases of proximal and distal femur fractures, we quantify the implant surface area and the estimated surface area of the average existing fracture line. Bone traumatization surface area was calculated with AutoCAD 2018 (Fig. 1).
When each trauma surface was compared, we found that the extent of metaphyseal trauma measured in TKA and THA is nearly identical and they had the largest traumatic surface area, while the plate and screw implant had the least traumatic surface area.
Based on this finding, we divided the samples into three surgery groups according to the extent of metaphyseal trauma, namely the total arthroplasty group (TA), comprised of TKA and THA; the hip hemiarthroplasty group (HA) comprised of HHA; and the open reduction and internal fixation group (ORIF) comprised of FF.
The existing DVT risk factors of each patient were recorded and listed according to the surgery group (Table 1). Various risk factors were analyzed to the DVT incidence and compared between each surgery group (Table 2). Data were evaluated by Chi-square test or Fisher’s exact test. A p value < 0.05 was considered statistically significant.
To identify the role of metaphyseal trauma as an independent risk factor for DVT, we conducted a multivariate logistic regression test between the existing risk factors and the surgery groups (TA and HA or ORIF) in association with DVT incidence (Table 3), where the extent of metaphyseal trauma was represented by the surgery groups.
All tests in this study were analyzed by using IBM SPSS Statistics 23. This study had been approved by the boards of the ethical committee of the two hospitals where the study was conducted with approval number 0584/RSPIK-DIR/VIII/08 and 0378/H04.8.4.5.31/PP36-KOMETIK/2010.
Result
From a total of 167 patients who underwent the procedures, 101 patients met the inclusion criteria. Twenty-five patients (24.8%) were found asymptomatic DVT positive. Where 16 patients out of 43 (37.2%) from TA, 5 patients out of 32 (15.6%) from HA and 4 patients out of 26 (15.4%) from ORIF were DVT positive. TA consisted of 43 non-emergency osteoarthrosis patients (42.6%) who underwent TKA and THA. HA consisted of 32 emergency sub-capital femur fracture patients (31.7%) treated with Austin Moore Hip Prosthesis (AMP) or Bipolar Hip Prosthesis (BHP) implants. Moreover, ORIF consisted of 26 emergency trochanteric and condylar femur fracture patients (25.7%), treated with either dynamic hip screws (DHS), condylar blade plate (CBP), proximal femur locking plate (PFLP) or cannulated screws (CS) implants.
The recorded existing risk factor from total patients was found to be dominated by older age > 70 years (61.4%), slender patients with BMI < 25 kg/m2 (68.3%), female (75.2%), hypertension (50.5%), 3 days total blood loss > 300 ml (81.2%), and high 7th day post-op D-dimer (70.3%) (Table 2). These risk factors were found mostly in emergency/acute trauma patients within the HA and ORIF.
From the bivariate analysis of the existing risk factors to DVT incidence in the three surgery groups, we found that the significant risk factors in each group were: hypertension in the TA group, high BMI and female gender in the HA group, and high LDL, HDL, and high D-dimer levels on the 7th day post-operation in the ORIF group. Meanwhile, when considering the total number of patients from all groups, significant risk factors included hypertension (p = 0.04, OR = 2.6), high D-Dimer on the 7th day post-op (p = 0.02, OR = 4.0), and long duration of surgery (p = 0.04, OR = 2.5) (Table 3).
The adjusted OR of the multivariate logistic regression test between the existing risk factors and the surgery groups (TA and HA or ORIF) showed for TA is 6.2 with a 95% CI (p = 0.036) in relation to the incidence of DVT. The other risk factors were not found to be significant except for hypertension (p = 0.05), although the OR was only 0.301 (Table 3).
Discussion
In this cohort study, we found that TA group have a sixfold increased risk of developing DVT (OR 6.2, p = 0.036). TA, comprised of TKR and THR, represents the largest extent of metaphyseal trauma (Fig. 1) that occurs in the hip and knee major orthopedic surgery. Apart from hypertension (OR 0.31, p = 0.054), the other risk factors were not significantly associated with an increased risk of DVT. This strongly implies that the metaphyseal trauma during hip and knee major orthopedic surgery itself has a role in DVT occurrence.
The distinguishing factor between major orthopedic surgery in hip and knee, as opposed to the other region, is the extent of trauma in the metaphysis. Hip fracture surgery, hip arthroplasty, and knee arthroplasty are strongly associated with the risk of developing DVT, with an incidence rate of 30–80% for asymptomatic DVT and 0.5–4% for symptomatic DVT [10, 11]. These surgeries primarily injured the heavily vascularized metaphyseal region of the lower extremities through bone cutting and reaming procedures [7]. Initial studies from the author have also demonstrated that metaphyseal bone trauma is linked with marked changes in thrombogenic biomarkers post-operatively and influence the incidence of DVT [12, 13]. Recent studies from Asian demographic also showed that simultaneous bilateral TKA increased the risk of DVT [14, 15]. Moreover, a large nationwide study by Seung et al. concluded TKA as one of a risk factor for developing postoperative DVT [10].
Concluding based on the previous statements, it can be implied that surgeries in the diaphyseal region cause less endothelial damage. Diaphyseal trauma is more commonly associated with the development of fat emboli [16]. For this reason, we mainly highlight the impact of metaphyseal trauma, rather than comparing between metaphyseal and diaphyseal trauma, as a risk factor for DVT.
Surgery is associated with several prothrombotic processes, which can be one or more components of Virchow's triad (venous stasis, endothelial damage, and hypercoagulability). Despite major orthopedic surgery having long been known as a risk factor for DVT [1], to our knowledge, the role of metaphyseal trauma as a risk factor in lower extremities, major orthopedic surgery on DVT incidence has not been proven before.
We measured the extent of metaphyseal trauma in our sample. Based on the measurement of metaphyseal trauma surface area, we observed that the largest area of metaphyseal trauma occurs in the TA (Fig. 1). This can be attributed to the extensive bone cutting and reaming involved in implant preparation during total arthroplasty of the hip and knee, which was performed to a lesser extent in the HA and ORIF.
From the patient demographic, we observed consistent findings with previous studies, with 24.8% of patients who underwent major orthopedic surgeries developing asymptomatic DVT, and consequently, the majority was TA patients (Table 1). It is worth noting that in our sample, the recorded existing DVT risk factors in the TA group were fewer compared to the other groups; however, they still had the highest incidence of DVT.
The existing risk factors in our sample were dominated by older age, female gender, hypertension, significant blood loss, and elevated D-dimer levels on the 7th day post-operation (Table 1). However, when we compare the existing risk factor with the incidence of DVT, the significant risk factors were indeed hypertension, high D-dimer levels, and longer surgical duration (p < 0.05) (Table 2). This aligns with previous research where patients with hypertension showed a twofold increased likelihood of developing DVT [17], while longer surgical durations were associated with a 1.2–threefold increase in the development of VTE [18, 19].
Even though many known DVT risk factors were present in our sample, they proved to be statistically insignificant. However, the incidence rate of DVT remained relatively high (24.8%). Consequently, we conducted logistic regression analysis to determine the presence of other risk factors, particularly metaphyseal trauma, which may increase the likelihood of DVT incidence. Within this analysis, we included the extent of metaphyseal trauma as one of the risk factors and compared it to the other existing risk factors. Both TA and HA/ORIF represent the extent of metaphyseal trauma that occurs in the hip and knee major orthopedic surgery. Here we found that the largest metaphyseal trauma in TA has a sixfold increase of developing DVT compared to HA and ORIF. Interestingly, a more recent study from Fu et al. with a larger sample found a similar finding in a femoral neck fracture population, where patients who underwent THR and HA have a higher incidence of DVT [20]. In the relationship between metaphyseal trauma area and DVT incidence, the isolated upper extremity fracture also is not associated with significant increase in DVT [21]. This finding adds to the literature by specifically identifying metaphyseal trauma as a risk factor in major orthopedic surgery and understanding the risk associated with different types of orthopedic trauma.
Excessive bone cutting in major orthopedic surgery has been widely known to cause complications, i.e., alignment and instability issues that could lead to implant loosening in the future [22]. The increasing risk of DVT during hip and knee surgery most likely occurs due to the injury to bone and soft tissues, which causes extensive endothelial damage. This stimulates the release of tissue factor, initiates local activation of the clotting cascade, and increases the activity of plasminogen activator inhibitor. Activation of coagulation results in the generation of excessive amounts of thrombin, which then leads to thrombus formation and platelet activation [23]. Minimizing metaphyseal bone trauma may play a crucial role in reducing DVT incidence by optimizing venous flow, preserving endothelial integrity, and reducing hypercoagulability.
The most significant finding of this study was that metaphyseal trauma is an independent risk factor for DVT, particularly in TKA and THA. Therefore, the necessity of fine surgical technique, gentle handling, adjustment in broaching and reaming technique, and correct sizing in major orthopedic surgery is now a critical part to mitigate the risk of DVT.
Clinical practice guidelines have been proposed to assist healthcare providers in offering prophylactic measures against the risk of DVT in major orthopedic surgery. At the same time, there is a lack of published evidence to give specific guidance for selection of the optimum thromboprophylaxis after surgery for fractures around the knee [24]. From our findings, the extent of metaphyseal trauma arises as a critical factor that warrants updating these guidelines to align with current practices.
Limitations
The sample size is limited, and the extent of metaphyseal damage was estimated indirectly based on implant surface measurements, as direct bone traumatization measurements were impractical intraoperatively. Another limitation to consider is that our study only focuses on the extent of metaphyseal trauma without a direct comparison to diaphyseal trauma. We also assume that the amount of soft tissue injury in all three groups is comparable. Due to the consecutive nature of the study, the number of patients in each group is unequal with also an unequal distribution of the risk factors.
Future directions
Future studies with a larger sample and more accurate measurement of bone traumatization will provide valuable insight into the role of metaphyseal bone trauma in DVT. Studies focusing on selective use of thromboprophylaxis based on the extent metaphyseal trauma, classified according to the type of orthopedic surgeries, could contribute to reach a thromboprophylaxis management consensus in clinical practice.
Conclusions
Metaphyseal bone trauma is an independent risk factor for deep vein thrombosis, especially in total knee and total hip arthroplasty.
Abbreviations
- AAOS:
-
American Academy of Orthopaedic Surgeon
- ACCP:
-
American College of Chest Physicians
- AMP:
-
Austin Moore Hip Prosthesis
- BHP:
-
Bipolar hip prosthesis
- BMI:
-
Body mass index
- CBP:
-
Condylar blade plate
- CKD:
-
Chronic kidney disease
- CS:
-
Cannulated screws
- D-1:
-
One day before surgery
- D + 7:
-
7 Days after surgery
- DHS:
-
Dynamic hip screws
- DVT:
-
Deep vein thrombosis
- FF:
-
Proximal and distal femur fixation
- HA:
-
Hemiarthroplasty group
- HDL:
-
High-density lipoprotein
- HHA:
-
Hip hemiarthroplasty
- LDL:
-
Low-density lipoprotein
- Med:
-
Median
- Min:
-
Minimum
- Max:
-
Maximum
- N:
-
Normal
- ORIF:
-
Open reduction and internal fixation
- OR:
-
Odds ratio
- PFLP:
-
Proximal femur locking plate
- Sig:
-
Significances
- TA:
-
Total arthroplasty group
- TKA:
-
Total knee arthroplasty
- VTE:
-
Venous thromboembolism
References
Waheed SM, Kudaravalli P, Hotwagner DT (2023) Deep vein thrombosis. StatPearls Publishing, In StatPearls
Falck-Ytter Y, Francis CW, Johanson NA, Curley C, Dahl OE, Schulman S, Ortel TL, Pauker SG, Colwell CW Jr (2012) Prevention of VTE in orthopedic surgery patients: antithrombotic therapy and prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141(2 Suppl):e278S-e325S. https://doi.org/10.1378/chest.11-2404
Jacobs JJ, Mont MA, Bozic KJ, Della Valle CJ, Goodman SB, Lewis CG, Yates AC Jr, Boggio LN, Watters WC 3rd, Turkelson CM, Wies JL, Sluka P, Hitchcock K (2012) American Academy of Orthopaedic Surgeons clinical practice guideline on: preventing venous thromboembolic disease in patients undergoing elective hip and knee arthroplasty. The J Bone Joint Surg 94(8):746–747. https://doi.org/10.2106/JBJS.9408.ebo746
Prevention of venous thrombosis and pulmonary embolism. NIH Consensus Development. JAMA (1986). 256(6):744–749
Cohen AT, Board A-P (2010) Asia-Pacific thrombosis advisory board consensus paper on prevention of venous thromboembolism after major orthopaedic surgery. Thromb Haemost 104(5):919–930. https://doi.org/10.1160/TH10-03-0190
Piovella F, Wang CJ, Lu H, Lee K, Lee LH, Lee WC, Turpie AG, Gallus AS, Planès A, Passera R, Rouillon A, AIDA investigators (2005) Deep-vein thrombosis rates after major orthopedic surgery in Asia. An epidemiological study based on postoperative screening with centrally adjudicated bilateral venography. J Thrombosis Haemostasis: JTH, 3(12):2664–2670. https://doi.org/10.1111/j.1538-7836.2005.01621.x
Shapiro F (2008) Bone development and its relation to fracture repair. The role of mesenchymal osteoblasts and surface osteoblasts. Eur Cells Mater 15:53–76. https://doi.org/10.22203/ecm.v015a05
Blokhuis TJ, Pape HC, Frölke JP (2017) Timing of definitive fixation of major long bone fractures: Can fat embolism syndrome be prevented? Injury 48(Suppl 1):S3–S6. https://doi.org/10.1016/j.injury.2017.04.015
Kalbas Y, Seaver T, Kumabe Y, Halvachizadeh S, Lempert M, Pfeifer R, Marcantonio A, Pape HC (2022) Fat embolism syndrome in patients with bilateral femur fractures: a systematic review and case comparison. OTA Int: The Open Access J Orthopaedic Trauma 5(2 Suppl):e187. https://doi.org/10.1097/OI9.0000000000000187
Lee SY, Ro duH, Chung CY, Lee KM, Kwon SS, Sung KH, Park MS (2015) Incidence of deep vein thrombosis after major lower limb orthopedic surgery: analysis of a nationwide claim registry. Yonsei Med J 56(1):139–145. https://doi.org/10.3349/ymj.2015.56.1.139
Januel JM, Chen G, Ruffieux C, Quan H, Douketis JD, Crowther MA, Colin C, Ghali WA, Burnand B, IMECCHI Group (2012) Symptomatic in-hospital deep vein thrombosis and pulmonary embolism following hip and knee arthroplasty among patients receiving recommended prophylaxis: a systematic review. JAMA 307(3):294–303. https://doi.org/10.1001/jama.2011.2029
Hartono F, Yusuf I, Suhadi B, Fachruddin A (2013) A study on prothrombogenic and antithrombogenic biomarkers in deep vein thrombosis following meta-epiphyseal cancellous bone traumatization in major orthopedic surgeries. Med J Indones [Internet]. https://mji.ui.ac.id/journal/index.php/mji/article/view/515. Accessed 2 November 2023
Hartono F, Yusuf I, Suhadi B, Fachruddin A, Augustinus Y (2021) Trauma magnitude of the meta-epyphyseal cancellous affects the incidence of deep vein thrombosis. A prospective cohort study on the dynamic of Collagen I, Collagen IV, Tissue factor, P-Selectin and Nitric Oxide in the thrombus formation following hip and knee surgeries. Ann Med Surg 63:102190. https://doi.org/10.1016/j.amsu.2021.102190
Lee JK, Lee KB, Kim JI, Park GT, Cho YC (2021) Risk factors for deep vein thrombosis even using low-molecular-weight heparin after total knee arthroplasty. Knee Surg Relat Res 33(1):29. https://doi.org/10.1186/s43019-021-00109-z
Liu L, Liu H, Zhang H, Song J, Zhang L (2019) Bilateral total knee arthroplasty: simultaneous or staged? A systematic review and meta-analysis. Medicine (Baltimore) 98(22):e15931. https://doi.org/10.1097/MD.0000000000015931
Giannoudis PV, Pape HC, Cohen AP, Krettek C, Smith RM (2002) Review: systemic effects of femoral nailing: from Küntscher to the immune reactivity era. Clin Orthop Relat Res 404:378–386
Huang L, Li J, Jiang Y (2016) Association between hypertension and deep vein thrombosis after orthopedic surgery: a meta-analysis. Eur J Med Res 21:13. https://doi.org/10.1186/s40001-016-0207-z
Kim JY, Khavanin N, Rambachan A, McCarthy RJ, Mlodinow AS, De Oliveria GS Jr, Stock MC, Gust MJ, Mahvi DM (2015) Surgical duration and risk of venous thromboembolism. JAMA Surg 150(2):110–117. https://doi.org/10.1001/jamasurg.2014.1841
Yu X, Wu Y, Ning R (2021) The deep vein thrombosis of lower limb after total hip arthroplasty: what should we care. BMC Musculoskelet Disord 22(1):547. https://doi.org/10.1186/s12891-021-04417-z
Fu YH, Liu P, Xu X, Wang PF, Shang K, Ke C, Fei C, Yang K, Zhang BF, Zhuang Y, Zhang K (2020) Deep vein thrombosis in the lower extremities after femoral neck fracture: a retrospective observational study. J Orthop Surg (Hong Kong) 28(1):2309499019901172. https://doi.org/10.1177/2309499019901172
Zhao WG, Zhang WL, Zhang YZ (2022) Characteristics of deep venous thrombosis in isolated lower extremity fractures and unsolved problems in guidelines: a review of recent literature. Orthop Surg 14(8):1558–1568. https://doi.org/10.1111/os.13306
Al-Jabri T, Brivio A, Maffulli N, Barrett D (2021) Management of instability after primary total knee arthroplasty: an evidence-based review. J Orthop Surg Res 16(1):729. https://doi.org/10.1186/s13018-021-02878-5
Mann KG, Brummel K, Butenas S (2003) What is all that thrombin for? J Thrombosis Haemostasis: JTH 1(7):1504–1514. https://doi.org/10.1046/j.1538-7836.2003.00298.x
Ricci WM, Broekhuyse H, Keating JF, Teague DC, White TO (2019) Thromboprophylaxis an update of current practice: Can we reach a consensus? OTA Int: The Open Access J Orthop Trauma 2(4):e027. https://doi.org/10.1097/OI9.0000000000000027
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Informed consent
All study participants provided informed written consent prior to study enrollment. This study had been approved by the board of the ethical committee of the Pantai Indah Kapuk Hospital dan Siloam Hospitals Kebon Jeruk where the study was conducted with approval number 0584/RSPIK-DIR/VIII/08 and 0378/H04.8.4.5.31/PP36-KOMETIK/2010.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hartono, F., Ananditya, T., Augustinus, Y. et al. Metaphyseal trauma of the lower extremities in major orthopedic surgery as an independent risk factor for deep vein thrombosis. Eur J Orthop Surg Traumatol (2024). https://doi.org/10.1007/s00590-024-03960-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00590-024-03960-4