Abstract
Purpose
This study aims to compare the functional and radiological outcomes following both guided growth surgery (GGS) and acute corrective osteotomy (ACO) correction of angular deformities in children with rickets.
Methods
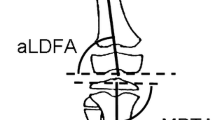
A total of 8 and 7 children who had gradual GGS and ACO correction, respectively, for angular deformities due to rickets from 2002 to 2022 were recalled for follow-up. Demographic data, types of rickets, data on pharmacological treatment, biochemical parameters, recurrence of angular deformity and postoperative complications were obtained from the medical records. A radiographic evaluation of the leg was performed to determine the tibiofemoral angle. For functional evaluation, the Active Scale for Kids (ASK) and Lower Extremity Functional Scale (LEFS) instruments were used for children below and above 15 years old, respectively.
Results
In terms of the tibiofemoral angle, the GGS group documented greater angle changes compared to the ACO group, but the difference was not significant. In terms of functional outcomes, the overall score percentage of both groups was comparable with the GGS group showing a trend of higher score percentage compared to the ACO group. The GGS group presented no complication while 2 neurovascular injuries and 1 implant failure were recorded in the ACO group.
Conclusion
Both GGS and ACO procedures resulted in similar radiographic and functional outcomes for the treatment of rickets in children. GGS may be advantageous in terms of reducing complications of surgery. Nevertheless, the choice of surgical intervention should be made based on the patient's circumstances and the surgeon's preference.
Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this published article.
References
Creo AL, Thacher TD, Pettifor JM et al (2017) Nutritional rickets around the world: an update. Paediatr Int Child Health 37:84–98. https://doi.org/10.1080/20469047.2016.1248170
Reddy KA (2020) Prevalence of rickets: a clinical study. Int J Contemp Pediatr 7:593. https://doi.org/10.18203/2349-3291.ijcp20200684
Gentile C, Chiarelli F (2021) Rickets in children: an update. Biomedicines. https://doi.org/10.3390/biomedicines9070738
Bitzan M, Goodyer PR (2019) Hypophosphatemic rickets. Pediatr Clin North Am 66:179–207. https://doi.org/10.1016/j.pcl.2018.09.004
De Cicco A, Toro G, Grandone A et al (2021) X-linked hypophosphatemic rickets. What the orthopedic surgeon needs to know. Int J Bone Fragility 1:59–66. https://doi.org/10.57582/IJBF.210102.059
Gottliebsen M, Shiguetomi-Medina JM, Rahbek O, Møller-Madsen B (2016) Guided growth: mechanism and reversibility of modulation. J Child Orthop 10:471–477. https://doi.org/10.1007/s11832-016-0778-9
Vaishya R, Shah M, Agarwal AK, Vijay V (2018) Growth modulation by hemi epiphysiodesis using eight-plate in Genu valgum in Paediatric population. J Clin Orthop trauma 9:327–333. https://doi.org/10.1016/j.jcot.2017.11.004
Stevens PM, Klatt JB (2008) Guided growth for pathological physes: radiographic improvement during realignment. J Pediatr Orthop 28:632–639. https://doi.org/10.1097/BPO.0b013e3181841fda
Al Kaissi A, Farr S, Ganger R et al (2013) Windswept lower limb deformities in patients with hypophosphataemic rickets. Swiss Med Wkly 143:w13904. https://doi.org/10.4414/smw.2013.13904
Feldman DS, Madan SS, Ruchelsman DE et al (2006) Accuracy of correction of tibia vara: acute versus gradual correction. J Pediatr Orthop 26:794–798. https://doi.org/10.1097/01.bpo.0000242375.64854.3d
Kuwashima U, Yonekura A, Itoh M et al (2020) Tibial condylar valgus osteotomy—indications and technique. J Exp Orthop 7:30. https://doi.org/10.1186/s40634-020-00247-5
Kolbe N, Haydon F, Kolbe J, Dreher T (2023) Single-stage tibial osteotomy for correction of genu varum deformity in children. Child. https://doi.org/10.3390/children10020377
Masquijo JJ, Artigas C, de Pablos J (2021) Growth modulation with tension-band plates for the correction of paediatric lower limb angular deformity: current concepts and indications for a rational use. EFORT open Rev 6:658–668. https://doi.org/10.1302/2058-5241.6.200098
Paley D, Tetsworth K (1992) Mechanical axis deviation of the lower limbs. Preoperative planning of multiapical frontal plane angular and bowing deformities of the femur and tibia. Clin Orthop Relat Res 280:65–71
Salenius P, Vankka E (1975) The development of the tibiofemoral angle in children. J Bone Jt Surg 57:259–261
Mohiuddin MJ, Rafeeq H, Mrudula K et al (2019) Genu valgum correction by distal femoral lateral open wedge corrective osteotomy. Int J Orthop Sci 5:344–346. https://doi.org/10.22271/ortho.2019.v5.i2g.45
Barakat AS, Arafa A, Mohamed MT et al (2022) Treatment of genu valgum by a novel percutaneous transverse metaphyseal osteotomy of the distal femur in children and adolescents. Eur J Orthop Surg Traumatol 32:1179–1186. https://doi.org/10.1007/s00590-021-03093-y
Sangnod DPA, U DH, Assudani DA, et al (2018) Effectiveness of eight plate in correcting angular deformity around knee: a study at tertiary care hospital. Int J Orthop Sci 4:1024–1028. https://doi.org/10.22271/ortho.2018.v4.i2o.146
El-Sobky TA, Samir S, Baraka MM et al (2020) Growth modulation for knee coronal plane deformities in children with nutritional rickets: a prospective series with treatment algorithm. J Am Acad Orthop Surg Glob Res Rev. https://doi.org/10.5435/JAAOSGlobal-D-19-00009
Gupta P, Gupta V, Patil B, Verma V (2020) Angular deformities of lower limb in children: correction for whom, when and how? J Clin Orthop trauma 11:196–201. https://doi.org/10.1016/j.jcot.2020.01.008
Yang I, Gottliebsen M, Martinkevich P et al (2017) Guided growth: current perspectives and future challenges. JBJS Rev 5:e1. https://doi.org/10.2106/JBJS.RVW.16.00115
Popkov A, Aranovich A, Popkov D (2015) Results of deformity correction in children with X-linked hereditary hypophosphatemic rickets by external fixation or combined technique. Int Orthop 39:2423–2431. https://doi.org/10.1007/s00264-015-2814-7
Bueno-Sánchez AM (2020) Surgical Indications in hypophosphataemic rickets. Adv Ther 37:113–120. https://doi.org/10.1007/s12325-019-01179-y
Colombo M, Mangano C, Mijiritsky E et al (2017) Clinical applications and effectiveness of guided implant surgery: a critical review based on randomized controlled trials. BMC Oral Health 17:150. https://doi.org/10.1186/s12903-017-0441-y
Funding
No funds, grants, or other support was received.
Author information
Authors and Affiliations
Contributions
ASM, KJ, AHAR, AFAR and NAA contributed to conceptualization; ASM, KJ, AHAR, AFAR and NAA contributed to methodology; ASM, KJ, AHAR, AFAR and NAA contributed to formal analysis and investigation; ASM contributed to writing—original draft preparation; ASM, KJ and AHAR contributed to writing—review and editing; and KJ, AHAR, and AR supervised the study.
Corresponding author
Ethics declarations
Conflict of interest
The author(s) declare that they have no competing interests.
Ethical approval
This study was approved by the Ethical Committee, Faculty of Medicine, Universiti Kebangsaan Malaysia (FF-2022–011).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Muhammad, A.S., Jamil, K., Abdul-Rashid, A.H. et al. Surgical outcome of angular deformity correction of lower limbs in rickets: a cross-sectional study. Eur J Orthop Surg Traumatol (2024). https://doi.org/10.1007/s00590-024-03943-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00590-024-03943-5