Abstract
Purpose
Acetabular fracture fixation can be challenging, especially in the elderly. Open reduction and internal fixation (ORIF) alone may not allow for early weight bearing and is associated with a high rate of secondary osteoarthritis; therefore, a combined hip procedure (CHP) or ORIF with acute total hip arthroplasty, may be beneficial in this population. The objective of this study was to perform a systematic review of all reported cases of CHP.
Methods
PubMed, Embase, Scopus, and Cochrane databases were searched for studies analyzing acetabular fractures in the elderly managed with a combined hip procedure (CHP). The research was performed following the PRISMA guidelines. The included studies' methodological quality was evaluated using the MINORS score. The present study was registered on PROSPERO.
Results
Eleven clinical studies were included in the final analysis. The mean age was 74.4 (63.2–78) years. Low-energy trauma was the most common mechanism of injury (64%). The most prevalent fracture pattern was the anterior column and posterior hemitransverse (ACPHT) (30.6%). The Kocher-Langenbeck approach was preferred for ORIF of posterior fractures and hip arthroplasty. The ilioinguinal approach and modified Stoppa were generally used for anterior fractures. The overall complication rate was 12.2%, and hip dislocation was the most frequent cause of reoperation (4.4%). The average Harris Hip Score reported postoperatively was 81.6 points, which was considered “good.”
Conclusions
CHP is a safe treatment for elderly acetabular fractures with an acceptable complication and reoperation rate that results in good clinical outcomes.
Level of evidence
Level of evidence IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Open reduction and internal fixation (ORIF) of acetabular fractures is challenging, especially in elderly patients with complex fractures and poor bone quality [1,2,3]. Unfavorable prognostic factors for ORIF in this patient population include articular impaction, comminution, preexisting osteoarthritis, severe osteopenia, or osteoporosis [4].
The management of acetabular fractures in the elderly population depends on the fracture pattern, fracture severity, and the patients’ general conditions [3, 4]. These fractures are typically treated with ORIF if no unfavorable prognostic factors are present, with the goal of preserving the native joint [5, 6]. In cases with one or more negative prognostic factors, a combined hip procedure (CHP), or ORIF with acute total hip arthroplasty (THA), can be considered due to the high risk of secondary osteoarthritis [3,4,5,6,7].
The most appropriate treatment for patients with these injuries is still under debate; ORIF has been shown to have better clinical results, while THA allows for immediate weight bearing and has lower reoperation rate [6, 7]. The purpose of this study was to provide a comprehensive systematic review of the present literature on CHP, to describe the indications, surgical approaches, and clinical and radiological outcomes of this procedure.
Materials and methods
Search criteria
This research was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The present study was registered in the PROSPERO database: CRD42022385186 [8, 9]. A comprehensive review of PubMed/Medline, Cochrane, Scopus, and Embase databases was performed using the following key terms in association with the Boolean operators AND, OR until December 2022: “acetabular fracture,” “total hip arthroplasty,” “open reduction internal fixation,” “ORIF,” “combined hip procedure,” “CHP,” and “THA.”
Inclusion and exclusion criteria
Articles that evaluated the clinical outcomes of patients treated with a combined hip procedure (ORIF and THA) for treating displaced acetabular fractures in patients older than 60 years were considered. Inclusion criteria were original articles written in English, which included at least ten patients, and a minimum follow-up of one year. Exclusion criteria were different surgical techniques, such as ORIF or THA alone, unavailable full-text articles, case reports, letters to the editor, biomechanics reports, and instructional course lectures.
Study screening
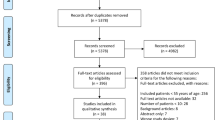
Two independent authors (GC and FP) independently searched by title and abstract. The full text was obtained and examined if the articles met the inclusion criteria following the title and abstract screening. If the title and abstract of each study did not contain sufficient information to determine its eligibility for inclusion, the full manuscript was examined. A cross-search of the selected articles was also conducted to obtain other articles relevant to the study. In case of disagreement between the two authors, a third author (AA) was consulted, and a consensus was reached. The search yielded 456 studies that were screened to determine the outcome of elderly patients treated with a CHP following acetabular fractures. After eliminating duplicate articles and applying inclusion and exclusion criteria, 11 clinical studies met the inclusion criteria and were included in the final analysis [10,11,12,13,14,15,16,17,18,19,20] (Fig. 1).
Data collection
For each study, the following data were collected: title, first author, year of publication, level of evidence (LoE), injury mechanism, classification according to Letournel and Judet [21], number of patients, patients who died and were lost to follow-up, age of patients, length of follow-up, indication, surgical approaches and techniques, complications, reinterventions, mortality rate, and patient-reported outcome measures scores (PROMs).
Methodological quality assessment
The Methodological Index for Non-Randomized Studies (MINORS) score routinely applied in the arthroplasty-related literature [22,23,24] was used to assess the quality of the included studies. For each question (8 items), the scale assigned a score of 0 if the item is not provided, 1 if the item is partially described, or 2 if the item is well-described. Study quality was assessed by the sum of all items: poor (0–5 points), moderate (6–10 points), and good (11–16 points). The risk of bias using the MINORS score was performed separately by two different authors (GC and FP), and in case of discrepancies, a third author (FB) was consulted.
Statistical analysis
A descriptive statistical analysis was conducted with R software, version 4.0.5 (2020; R Core Team, Vienna, Austria). Categorical variables were presented as an absolute number and frequency distribution. Continuous variables were presented as means and standard deviation (SD), with the range between minimum and maximum values. A p-value < 0.05 was considered statistically significant.
Results
Quality assessment
The quality of the eleven included studies [10,11,12,13,14,15,16,17,18,19,20] was assessed, and the mean score was 11.2 (range, 9–12), of which eight were rated good quality. The remaining three studies were rated as moderate quality. No study was classified as poor (Table 1).
Demographic and clinical data
A total of 302 hips were initially included. After excluding thirty-two hips (10.6%) due to missing data or patients lost to follow-up, 270 hips were left for analysis. The mean age at the time of surgery was 74.4 (range 63.2–78) years. There were 117 women (38.7%) and 185 men (61.3%). The mean follow-up was 23.7 (range 12–58) months (Table 1). Ten of the eleven included studies reported the mechanism of injury (222 hips) [10,11,12,13,14,15,16,17,18,19]. Low-energy trauma from ground-level falls was the most common mechanism in 64% of cases (142 hips), while high-energy trauma was responsible for 36% of cases (80 hips). Ten of the eleven included studies reported fracture classification according to Judet and Letournel’s criteria (245 hips) [11,12,13,14,15,16,17,18,19,20,21]. Associated pattern fractures were more common than simple fractures, with 180 cases (73.5%) and 65 cases (26.5%), respectively. The most common fracture pattern was an anterior column and posterior hemitransverse (ACPHT, 75 cases, 30.6%), followed by both column fractures (39 cases, 15.9%). For simple pattern fractures, posterior wall fractures were the most common (29 cases, 11.8%) (Table 2).
Indications and surgical approach
All included studies reported data on factors that should be considered preoperatively before performing a CHP because of the high risk of secondary osteoarthritis after ORIF alone [10,11,12,13,14,15,16,17,18,19,20]. Six factors were identified: preexisting hip osteoarthritis [11, 12, 14, 19], presence of acetabular dome impaction [10,11,12, 14, 16,17,18,19,20], femoral head impaction [10,11,12, 14, 15, 17,18,19,20], intra-articular comminution [10,11,12, 14, 15, 17], posterior wall involvement alone or in association with other fracture patterns [10, 11, 13, 17], and preexisting osteopenia/osteoporosis [14, 17, 20] (Table 3).
All included studies [10,11,12,13,14,15,16,17,18,19,20] reported details of the surgical approaches used for CHP (Table 4). A Kocher-Langenbeck (KL) approach in lateral decubitus was generally used for the fixation of posterior fractures. In three studies [15, 16, 19], anterior pattern fracture fixation was conducted through an ilioinguinal approach. Two studies reported anterior fracture fixation by a modified Stoppa approach [11, 14]. Two studies reported the ilioinguinal or Stoppa approach based on fracture patterns [12, 18]. In one study, the fixation of both anterior and posterior fractures was performed by percutaneous technique [17]. In all included studies [10,11,12,13,14,15,16,17,18,19,20], THA was performed with the KL approach.
Complications, reoperations, and revisions
All included studies [10,11,12,13,14,15,16,17,18,19,20] reported data on postoperative complications. The overall complication, reoperation, and prosthetic revision rates were 12.2% (33 cases), 6.3% (17 cases), and 3.7% (10 cases), respectively. The most frequent complication was hip dislocation (12 cases, 4.4%), followed by heterotopic ossification (eight cases, 3%) and periprosthetic joint infection (PJI) (five cases, 1.9%) (Table 5).
Clinical scores
Eight included studies [10,11,12, 14,15,16, 19, 20] reported at least one clinical score. Five studies [10, 12, 14, 19, 20] reported the mean postoperative Harris Hip Score (HHS) (mean 81.6, range 72–92.5). Three studies [10, 12, 15] reported the mean postoperative Short Form-36 score, the mean value for physical component synthesis (PCS) was 48.9 (range 41.3–67.5), while the mean value for mental component synthesis (MCS) was 36.4 (range 12.5–45.6). Two studies [11, 16] reported the mean value of the Oxford Hip Score (OHS) (mean 38.7, range 37.3–41). Two studies [12, 15] reported the mean Pelvic Discomfort Index (PDI) (mean 46.7, range 28.5–57.9). One study reported the mean Western Ontario and McMaster Universities Arthritis Index (WOMAC) (mean 16.5 ± 13.9) [10] (Table 6).
Discussion
Results summary
In this systematic review and meta-analysis, the CHP achieved good clinical results with acceptable complication rates. Acetabular fractures treated with CHP were typically caused by low-energy trauma (64% of cases) and patients had an average age of 74.5 years. The complication, reoperation, and prosthetic revision rates were 12.2%, 6.3%, and 3.7%, respectively. Hip dislocation was the most frequent postoperative complication (4.4%), requiring revision in 50% of cases. The average HHS reported postoperatively was 81.6 points, which was considered good.
Indications
Open reduction and internal fixation is the standard treatment for displaced acetabular fractures. However, in elderly patients with fractures that have negative prognostic factors, such as articular impaction and preexisting arthritis, the high rate of secondary hip osteoarthritis limits the success of this procedure [25, 26]. There are now a substantial number of studies evaluating [10,11,12,13,14,15,16,17,18,19,20] CHP in this setting warranting this systematic review. We identified six different factors that are used to identify patients the CHP may be appropriate for, including preexisting hip osteoarthritis, acetabular dome impaction, femoral head impaction, intra-articular comminution, fractures that include involvement of posterior wall, and preexisting osteopenia/osteoporosis [27].
Secondary osteoarthritis is the leading cause of reoperation after ORIF for acetabular fractures [28,29,30]. In a series of ORIF alone, Smakaj et al. [12] reported that 29.2% of patients developed secondary osteoarthritis and required THA. Similarly, Manson et al. [10] reported that 16% of patients treated by ORIF developed secondary osteoarthritis. In a recent systematic review, McCormick et al. [31] reported that patients managed with ORIF, independent from fracture patterns, showed a THA conversion rate of 15% at an average of 16.7 months.
A poor acetabular reduction (> 3 mm gap) can lead to early degeneration of the hip joint and a rapid development of secondary osteoarthritis [32,33,34]. In young patients with good bone quality, performing an ORIF to obtain an anatomic reduction is essential and not debated [32, 33]. But in case of complex fractures (acetabular dome impaction, femoral head impaction, and intra-articular comminution) in elderly patients with poor bone quality, the CHP may be a superior treatment [34]. Fractures involving the posterior wall, alone or in association with other patterns, such as transverse plus posterior wall, T-Type, ACPHT, and both columns, are associated with a higher risk of non-anatomic reductions and secondary osteoarthritis [34]. Several biomechanics studies reported that even a minimum posterior wall defect significantly increases the superior contact forces leading to early degenerative changes [32,33,34].
Surgical approaches
The primary surgical objective is to restore the relationship between the ischium and anterior inferior iliac spine to ensure the stability of the acetabular component. The choice between the anterior and KL approaches depends on the fracture's location and associated comminution. KL is the gold standard approach for managing posterior column area fractures. KL approach allows the direct visualization of the entire posterior column, posterior wall, and supra-acetabular region. Isolated posterior wall, isolated posterior column, associated posterior wall and column, and fractures with posterior wall/column fragment could be treated through the KL approach [35, 36].
On the other hand, the limitations of a KL approach become apparent when dealing with isolated anterior wall/column fractures or when confronting associated fractures accompanied by anterior fragments. The intricacies of such fractures demand alternative strategies beyond the scope of a KL approach [35, 36]. In the case of fracture involving the anterior column fragment, experts like Manson and Chen et al. [37, 38] propose a more comprehensive solution involving reduction and fixation through an anterior approach. Subsequently, the avenue for a successful THA through a KL approach opens up. This hybrid approach capitalizes on the strengths of both techniques to ensure optimal outcomes. In situations where obtaining adequate column stability poses a challenge via the posterior approach alone, the necessity of an anterior approach for ORIF becomes evident. To bolster column stability, recourse to an anterior approach, such as the ilioinguinal approach or the modified Stoppa approach, might become inevitable for addressing anterior wall fractures [10, 12, 37, 38]. This multifaceted approach underscores the adaptable nature of fracture management, tailored to the unique demands of each case.
Complications
The complexity of the surgery during CHP leads to various and frequent intraoperative and postoperative complications, and outcomes following CHP for acetabular fractures have previously been quite unpredictable. However, all studies and reviews considered postoperative instability and dislocation the most frequent complications and leading causes of revision [39]. The all-cause reoperation-free survivorship was 93.7%, and the all-cause revision-free survivorship was 96.3% at an average follow-up of 23.7 months. We reported a pooled CHP survivorship similar to the revision rate reported in a recent systematic review on acute THA for acetabular fracture (21 studies, 430 acetabular fractures with a revision rate of 4.3% [40]). The reoperation rate of CHP reported in our study is significantly lower than that of ORIF alone, as reported by McCormick et al. [31] who reviewed 19 studies with 1413 patients, and found a 15% rate of conversion to THA.
In our review, recurrent dislocation as a complication was reported in 12 (4.4%) cases, and 50% of them required component revisions. Different authors described many techniques to reduce the risk of dislocation [41, 42]. Three of the eleven studies suggest using dual mobility liners to reduce the risk of recurrent dislocation [11, 14, 15]. Despite using dual mobility liners, Hislop et al. [11] reported a dislocation rate of 23.8% (five cases). Only one required revision of the component due to recurrent dislocation, while the remaining four were managed by closed reduction showing no further dislocation.
PROMs
Despite the complexity of the surgical procedure and the relatively high complication associated with a CHP for the treatment of acetabular fracture in the elderly, patients showed good function scores. The average HHS, reported by five studies [10, 12, 14, 19, 20], was considered “good.” Manson reported an “optimal” average postoperative HHS with 92.5 points. Two studies reported a “good” average postoperative [12, 20], while two studies reported an average “fair” postoperative HHS [14, 19]. Comparing the average postoperative HHS reported by using CHP with the average HHS reported by McCormick et al. [31] for ORIF alone and THA, there were no significant differences.
Two studies reported the average postoperative pelvic discomfort index (PDI) score. PDI is a 14-items questionnaire developed in 2015 by Borg et al. [15] to evaluate the outcomes following pelvic ring or acetabular fracture. It ranges from 0% (no discomfort) to 100% (maximum discomfort). Manson et al. [10] reported an average PDI score of 57.9 points after two years after surgery, meaning that patients reported “severe discomfort.” On the other hand, Borg et al. [15] reported "moderate" pelvic discomfort, with an average score of 35 points. In both studies, the average PDI was higher, meaning that CHP causes more pelvic discomfort than ORIF alone, but the difference does not reach a statistically significant value [10, 15].
Limitations
The included research quality is inextricably linked to the quality of this systematic review. A critical flaw in our systematic review was the absence of Level I or II comparative clinical trial studies. In general, selection bias is more likely to occur in Level III and IV research. These limitations are evidenced in the low average MINORS score and methodological issues such as the lack of consecutively examined patients and prospective study designs.
We were unable to do a meta-analysis because there were insufficient homogenous comparison papers available. Additionally, we could not account for several variables that affected the results of our investigation. Some studies differed according to patient characteristics, prostheses, implantation by various surgeons, techniques, and approaches with various rehabilitation programs. Most studies did not explicitly state whether any associated procedures were carried out.
Additionally, our ability to report complications was somewhat constrained by varied (and frequently insufficient) descriptions of complications, radiographic characteristics, and distinctions between minor and major complications. Because the included studies did not describe the results separately by gender or age, no subgroup analysis involving gender or age groups could be carried out.
Conclusion
In patients with complex acetabular fracture, in the presence of one or more negative prognostic factors for developing secondary osteoarthritis after ORIF alone, CHP provides good hip functionality, quality of life, and an acceptable complication rate. In addition, our data suggest that CHP, in comparison with ORIF alone, reduces the complication and reoperation rates while resulting in similar PROMs. The CHP can be challenging however, and should likely be reserved for tertiary centers where experienced arthroplasty and pelvic trauma surgeons can work together to obtain the most optimal outcomes for these patients.
Data availability
The dataset analyzed in this study is available from the corresponding author on reasonable request.
References
Riemenschneider J, Vollrath JT, Mühlenfeld N, Frank J, Marzi I, Janko M (2022) Acetabular fractures treatment needs in the elderly and nonagenarians. I Open Rev 7(6):433–445
Walls A, McAdam A, McMahon SE, Diamond OJ (2021) The management of osteoporotic acetabular fractures: current methods and future developments. Surgeon 19(5):e289–e297
Tissingh EK, Johnson A, Queally JM, Carrothers AD (2017) Fix and replace: An emerging paradigm for treating acetabular fractures in older patients. World J Orthop 8(3):218–220
Cohen DA, Montgomery SJ, Stavrakis A, Mears SC, Atrey A, Khoshbin A (2021) Treatment of geriatric acetabular fractures-a concise review of the literature. Orthop Clin North Am 52(4):323–333
Daurka JS, Pastides PS, Lewis A, Rickman M, Bircher MD (2014) Acetabular fractures in patients aged > 55 years: a systematic review of the literature. Bone Joint J 96-B(2):157–63
Boelch SP, Jordan MC, Meffert RH, Jansen H (2017) Comparison of open reduction and internal fixation and primary total hip replacement for osteoporotic acetabular fractures: a retrospective clinical study. Int Orthop 41(9):1831–1837
Nicol GM, Sanders EB, Kim PR, Beaulé PE, Gofton WT, Grammatopoulos G (2021) Outcomes of total hip arthroplasty after acetabular open reduction and internal fixation in the elderly-acute versus delayed total hip arthroplasty. J Arthroplasty 36(2):605–611
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71
Bosco F, Giustra F, Crivellaro M, Giai Via R, Lavia AD, Capella M et al (2022) Is augmentation the best solution in partial anterior cruciate ligament tears? A literature systematic review and meta-analysis. J Orthop 36:11–17
Manson TT, Slobogean GP, Nascone JW, Sciadini MF, LeBrun CT, Boulton CL et al (2022) Open reduction and internal fixation alone versus open reduction and internal fixation plus total hip arthroplasty for displaced acetabular fractures in patients older than 60 years: A prospective clinical trial. Injury 53(2):523–528
Hislop S, Alsousou J, Chou D, Rawal J, Hull P, Carrothers A (2022) Fix and replace: simultaneous fracture fixation and hip replacement for acetabular fractures in older patients. Injury 53(12):4067–4071
Smakaj A, Rovere G, Scoscina D, De Mauro D, Erasmo R, Battiato C et al (2022) Outcomes of acetabular fractures treated with acute fix and replace versus open reduction and internal fixation in elderly population: a multicentric retrospective study. Int Orthop 46(11):2659–2666
Selvaratnam V, Panchani S, Jones HW, Chitre A, Clayson A, Shah N (2021) Outcomes of acute fix and replace in complex hip posterior fracture dislocations with acetabular fractures : a minimum of 3 years follow-up. Acta Orthop Belg 87(4):635–642
Lannes X, Moerenhout K, Duong HP, Borens O, Steinmetz S (2020) Outcomes of combined hip procedure with dual mobility cup versus osteosynthesis for acetabular fractures in elderly patients: a retrospective observational cohort study of fifty one patients. Int Orthop 44(10):2131–2138
Borg T, Hernefalk B, Hailer NP (2019) Acute total hip arthroplasty combined with internal fixation for displaced acetabular fractures in the elderly: a short-term comparison with internal fixation alone after a minimum of two years. Bone Jt J 101(4):478–483
Lont T, Nieminen J, Reito A, Pakarinen TK, Pajamäki I, Eskelinen A et al (2019) Total hip arthroplasty, combined with a reinforcement ring and posterior column plating for acetabular fractures in elderly patients: good outcome in 34 patients. Acta Orthop 90(3):275–280
Chakravarty R, Toossi N, Katsman A, Cerynik DL, Harding SP, Johanson NA (2014) Percutaneous column fixation and total hip arthroplasty for the treatment of acute acetabular fracture in the elderly. J Arthroplasty 29(4):817–821
Rickman M, Young J, Trompeter A, Pearce R, Hamilton M (2014) Managing acetabular fractures in the elderly with fixation and primary arthroplasty: aiming for early weightbearing. Clin Orthop Relat Res 472(11):3375–3382
Herscovici D Jr, Lindvall E, Bolhofner B, Scaduto JM (2010) The combined hip procedure: open reduction internal fixation combined with total hip arthroplasty for the management of acetabular fractures in the elderly. J Orthop Trauma 24(5):291–296
Boraiah S, Ragsdale M, Achor T, Zelicof S, Asprinio DE (2009) Open reduction internal fixation and primary total hip arthroplasty of selected acetabular fractures. J Orthop Trauma 23(4):243–248
Judet R, Judet J, Letournel E (1964) Fractures of the acetabulum: classification and surgical approaches for open reduction. Preliminary report. J Bone Jt Surg Am 46:1615–1646
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 73(9):712–716
Risitano S, Cacciola G, Sabatini L, Capella M, Bosco F, Giustra F et al (2022) Restricted kinematic alignment in primary total knee arthroplasty: A systematic review of radiographic and clinical data. J Orthop 33:37–43
Cacciola G, Bosco F, Giustra F, Risitano S, Capella M, Bistolfi A et al (2022) Learning curve in robotic-assisted total knee arthroplasty: a systematic review of the literature. Appl Sci 12(21):11085
Matta JM (1996) Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Jt Surg Am 78(11):1632–1645
Cimerman M, Kristan A, Jug M, Tomaževič M (2021) Fractures of the acetabulum: from yesterday to tomorrow. Int Orthop 45(4):1057–1064
Murphy D, Kaliszer M, Rice J, McElwain JP (2003) Outcome after acetabular fracture. Prognostic factors and their inter-relationships. Injury 34(7):512–517
Cacciola G, Aprato A, Branca Vergano L, Sallam A, Massé A (2022) Is non-operative management of acetabular fracture a viable option for older patients? A systematic review of the literature for indication, treatments, complications and outcome. Acta Biomed 92(S3):e2021555
Zha GC, Sun JY, Dong SJ (2013) Predictors of clinical outcomes after surgical treatment of displaced acetabular fractures in the elderly. J Orthop Res 31(4):588–595
Yuan Q, Wang X, Cai Y, Yang M, Zheng H, Zhao X et al (2022) Total hip arthroplasty for posttraumatic osteoarthritis secondary to acetabular fracture: An evidence based on 1284 patients from 1970 to 2018. Front Surg 9:953976
McCormick BP, Serino J, Orman S, Webb AR, Wang DX, Mohamadi A et al (2022) Treatment modalities and outcomes following acetabular fractures in the elderly: a systematic review. Eur J Orthop Surg Traumatol 32(4):649–659
Olson SA, Bay BK, Pollak AN, Sharkey NA, Lee T (1996) The effect of variable size posterior wall acetabular fractures on contact characteristics of the hip joint. J Orthop Trauma 10(6):395–402
Lin SY, Ho CJ, Liu WC, Chen JK, Tu HP, Lee TC et al (2022) Predicting the poor clinical and radiographic outcomes after the anatomical reduction and internal fixation of posterior wall acetabular fractures: a retrospective analysis. J Clin Med 11(11):3244
Kojima KE, Fuller H, Vieira TJAC, Clemente HRA, Zanesco L, Leonhardt MC et al (2022) Pre-operative predictors of poor reduction in acetabular fractures submitted to surgical treatment. Injury 53(11):3769–3773
Timmer RA, Mostert CQB, Krijnen P, Meylaerts SAG, Schipper IB (2022) The relation between surgical approaches for pelvic ring and acetabular fractures and postoperative complications: a systematic review. Eur J Trauma Emerg Surg. https://doi.org/10.1007/s00068-022-02118-3
Tian S, Zhang R, Liang S, Yin Y, Ma L, Liu G et al (2022) Is plating fixation through the Kocher-Langenbeck approach for associated posterior wall fragment indispensable in both-column acetabular fractures? Orthop Surg 14(3):513–521
Manson TT (2020) Open reduction and internal fixation plus total hip arthroplasty for the acute treatment of older patients with acetabular fracture: surgical techniques. Orthop Clin North Am 51(1):13–26
Chen Z, Yang H, Wu Z, Chen G, Ou Y, Bi X et al (2019) A combination of the modified Stoppa approach and the iliac fossa approach in treating compound acetabular fractures by using an anterior ilioischial plate. Acta Orthop Belg 85(2):182–191
Morison Z, Moojen DJ, Nauth A, Hall J, McKee MD, Waddell JP et al (2016) total hip arthroplasty after acetabular fracture is associated with lower survivorship and more complications. Clin Orthop Relat Res 474(2):392–398
Jauregui JJ, Weir TB, Chen JF, Johnson AJ, Sardesai NR, Maheshwari AV et al (2020) Acute total hip arthroplasty for older patients with acetabular fractures: A meta-analysis. J Clin Orthop Trauma 11(6):976–982
Romagnoli M, Grassi A, Costa GG, Lazaro LE, Lo Presti M, Zaffagnini S (2019) The efficacy of dual-mobility cup in preventing dislocation after total hip arthroplasty: a systematic review and meta-analysis of comparative studies. Int Orthop 43(5):1071–1082
Mancino F, Cacciola G, Di Matteo V, De Marco D, Greenberg A, Perisano C et al (2020) Reconstruction options and outcomes for acetabular bone loss in revision hip arthroplasty. Orthop Rev (Pavia) 12(Suppl 1):8655
Funding
Open access funding provided by Università degli Studi di Torino within the CRUI-CARE Agreement. No funding has been received for this study.
Author information
Authors and Affiliations
Contributions
GC, FP, FG, and FB have made substantial contributions to conception and design, acquisition of data, analysis, and interpretation of data, have been involved in drafting the manuscript or revising it critically for important intellectual content, and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. GR and IDM have made substantial contributions to the analysis and interpretation of data and have been involved in drafting the manuscript. LS, LC, and AM have made substantial contributions to conception and design and have drafted the manuscript. All the authors participated in the writing of the article and gave final approval of the version to be published.
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Giustra, F., Cacciola, G., Pirato, F. et al. Indications, complications, and clinical outcomes of fixation and acute total hip arthroplasty for the treatment of acetabular fractures: A systematic review. Eur J Orthop Surg Traumatol 34, 47–57 (2024). https://doi.org/10.1007/s00590-023-03701-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-023-03701-z




