Abstract
Introduction
Aim of our study was to evaluate the influence of working length and screw density on callus formation in distal tibial fractures fixed with a medial bridge plate.
Materials and methods
42 distal tibia fractures treated with a bridge plate were analyzed. Minimum follow-up was 12 months. mRUST score (modified Radiographic Union Scale for Tibial fractures) was used to assess callus formation. Working length and screw density were measured from post-operative radiographs.
Results
39 (92.9%) fractures healed uneventfully. 32 (76.19%) patients showed signs of early callus formation 3 months post-surgery. In these patients a lower screw density was used compared to patients who didn’t show early callus (33.4 vs. 26.6; p = 0.04). No differences was noticed in working length.
Conclusion
Bridge plate osteosynthesis is a good treatment option in distal tibia fractures. In our series increasing the working length was not associated with a faster callus formation in distal tibia fractures. Conversely, a lower screw density proximally to the fracture site was associated to a faster callus growth.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Distal tibial fractures account for 3–10% of all tibial fractures or 1% of lower extremities fractures [1]. As these fractures are often caused by high-energy trauma, the association with bone comminution and extensile soft tissue damage is very common. Comminution at the fracture site makes anatomic reduction unfeasible. Aiming for a secondary bone healing through a bridge plate is the treatment associated with higher rates of success [2].
Controversy exists on how to recreate the most biomechanically effective environment for bridge plate osteosynthesis. Many studies have investigated how plate design, plate length and screw configuration can influence fixation stability and promote fracture healing, often with unclear results.
One of the most important parameters regulating plate-screws stiffness and construct stability is working length which is defined as the distance between the two innermost screws on either side of the fracture. Larger working length makes fixation more flexible, in an effort to reduce strain and stress on the plate [3].
Another parameter that has been investigated in previous studies is screw density. This parameter influences system rigidity. It has been suggested empirically that half of the holes in the plate should be occupied by screws [4].
Many biomechanical studies on locking plates focused on diaphyseal fractures of the femur, where a positive association between working length and fracture healing was demonstrated. Few studies have investigated these associations in the treatment of distal tibial fractures. The aim of this study is to analyze the influence of working length and screw density on distal tibia fractures fixed with a medial bridge plate. Specifically, we investigated how these parameters affect the velocity of callus formation at 3 months and the fracture healing at 1 year.
Material and methods
This is a retrospective analysis of a consecutive series of patients treated for distal tibia fractures at authors’ institution from January 2014 to December 2019. All fractures treated with a medial bridge plate were included. The same plate (LCP Metaphyseal Plate for distal medial tibia 3.5–4.5, Depuy Synthes, Warsaw, IN) was used in all patients but in different sizes. In all patients only locking screws were used proximally to fracture site. Patients were excluded when non-locking or hybrid fixation was used proximally. Patients treated with a different plate were excluded. Distal tibia fractures that were fixed using more than one bridge plate were excluded. Fractures treated using the aforementioned Distal Tibia LCP plus a fibular plate were included. Fractures treated with intramedullary nail, lag screw or compression plate were also excluded. Patients’ demographics were recorded. We excluded patients under 18 year and over 85 years, patients with neuromuscular diseases or diseases affecting bone metabolism, heavy smokers (2 packs/day) and patients with previous fractures in the affected limb. Open fractures were also excluded.
Two senior trauma surgeons (> 10 years of experience) classified the fractures according to the AO/OTA classification based on preoperative X-rays and CT scans.
Surgical procedure
All procedures were performed by the two aforementioned fellowship-trained trauma surgeons. Informed consent was obtained from all patients prior to surgery. In high energy fractures with severe tissue swelling a two-stage treatment was performed. First an external fixator spanning the ankle joint was applied and then, at oedema subsidence, definitive fixation was performed 7–15 days after trauma. A single shot of cefazolin or clindamycin was administered. Under general or spinal anesthesia, patients were positioned supine on a radiolucent table. No tourniquet was used during the surgical procedure. Whenever possible tibial fracture was reduced percutaneously or with a surgical approach centered on the fracture site. After adequate reduction, all tibia fractures were fixed with a medial bridge plate. Percutaneous osteosynthesis was preferred whenever technically feasible. If a fibula fracture was associated, it was fixed based on surgeon preference and experience. The patients began ankle mobilization on postoperative day 1. Toe-touch weight bearing was allowed from the second post-operative week. From the forth to the tenth post-operative week partial weight bearing (20 kg) was prescribed and after that weight bearing as tolerated was allowed.
Biomechanical parameters evaluation
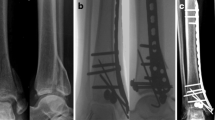
On post operative radiographs and on operative reports the following parameters were collected: plate length, number and location of the screws, working length (defined as the distance between the two innermost screws in mm) and proximal screw density. According to Harvin et al. proximal screw density was calculated as L/n, where L is the length of the plate proximally to the fracture site and n is the number of screws proximally to the fracture. It is expressed in mm [5] (Fig. 1). In distal metaphysis screw placement is dictated by the limited space available and by plate design, thus screw density distally from fracture site wasn’t analyzed. Fracture healing was evaluated according to the modified Radiographic Union Scale in Tibia (mRUST) on AP and LL X-rays 3–6–12 months post-op by two surgeons not involved in the treatment. mRUST defines bone healing based on the number of cortices bridged by callus [5,6,7]. Union was defined as a minimum mRUST score of 10. Early callus formation was noticed when mRUST score > 8 on 3 months post-surgery radiographs (Fig. 2). In this study the authors analyze whether longer working length and lower screw density were associated with early (< 3 months) callus formation and definitive fracture healing (at 1 year follow-up).
Pre operative radiographs of a left tibia show a 42-B2 fracture with an associated transverse fibula fracture. The tibial fracture was treated with a medial distal tibial bridge plate. Working length is depicted on post operative radiograph (WL). Screw density is defined as the length of the plate proximally to the fracture site (L) divided by the number of screws proximally. In this radiograph L is 112 mm, resulting in a screw density of 37.3 mm
Statistical analysis
Statistical analysis was performed using SPSS Statistics 20.0 software (IBM, Armonk, NY). Differences in age and sex were analyzed with Pearson’s Chi-squared test and Fisher’s exact test. Differences in fracture type were analyzed with the Freeman–Halton extension of the Fisher’s exact. The Student’s t test was performed to compare averages in screw density values and working length values. Association between fibula fixation and callus formation was investigated with Pearson’s Chi-squared test. A p value of < 0.05 was considered statistically significant. No power analysis has been performed during the design of the study.
Results
Forty-two patients met the inclusion criteria: 30 male and 12 female. Mean age was 55.3 year (SD 16.4; 26–85). All fractures were classified according to AO/OTA. A bridge plate osteosynthesis was performed in every patient. LCP Metaphyseal Plate for distal medial tibia 3.5–4.5 was used in every patient. Patients demographic, fracture characteristics and biomechanical parameters are summarized in Table 1.
Mean working length of the construct was 103.0 mm (SD 32.9; 29.7–168.6). Mean screw density was 31.8 mm (SD 7.0; 17.6–44.0). Working length and screw density values were normally distributed according to Shapiro–Wilk test.
32 patients (76.19%) showed radiographic signs of early callus formation (mRUST score > 8 at 3 months). Patients with signs of early callus were not different to patients without early callus according to age (p = 0.29), sex (p = 0.70) and fracture type (p = 0.95). Mean working length in patients with early callus was 103.1 (± 32.2) mm. In patients who didn’t reach early callus formation the mean working length was 102.4 (± 37.0) mm. No significant difference in the two group was found (p = 0.95). Conversely, patients who presented early callus had a significant lower screw density (33.4 mm vs. 26.6 mm, p = 0.04).
9 patients (21.4%) had an intact fibula at presentation. Among the 33 fractured fibulas only 20 were fixed surgically (60.6%). 13 patients had a fractured fibula that was not fixed during surgery. Among the patients with a fractured fibula, no difference in early callus formation was noticed if fibula was fixed or left untouched (p = 0.39).
39 fractures (92.9%) healed uneventfully, while 3 patients (7.1%) presented major complications, namely one nonunion and two infections, that required further surgical procedures. Of note, none of these patients was smoker or had a diagnosis of diabetes. Two patients healed at 1 year follow-up, one was lost at follow-up. 34 fractures (80.9%) were treated with percutaneous (MIPO) osteosynthesis.
Discussion
Although distal tibial fractures are very common injuries, some aspects of their treatment remain unclear. In the past two decades many studies have investigated LCP plate osteosynthesis on long bone fractures. Most of them consist of clinical and biomechanical studies focusing on femur [8,9,10,11,12]. Fewer studies focused on the treatment of distal tibia fracture [13, 14]. To the best of our knowledge none investigated how working length and screw density affect construct stability and promote callus formation on distal tibia fractures. These parameters are of paramount importance especially when planning a bridge plate osteosynthesis [15].
Since their introduction locking plates have gained popularity because they showed to provide more stable fixation than conventional non-locking plates, especially in metaphyseal and osteoporotic bone and in highly comminuted fractures. However, some authors argue that LCP plates are too stiff and do not allow the interfragmentary movement needed for callus formation with a rate of insufficient callus formation up to 40% at 6 months follow-up [16].
Increasing the working length is one way to reduce the stiffness of the plate-screw construct [17]. Based on this assumption, we hypothesized that in the context of distal tibia fractures longer working length reduced time to callus formation. Conversely our result showed no significant correlation between callus formation and working length. Our data seems to confirm Parks et al. findings [18]. In their study the authors claim there is no correlation between callus formation and construct stiffness and working length.
We assume that the reason behind the lack of correlation between longer working length and faster callus formation is that in our series many patients (20 out of 42) underwent fibula fracture fixation simultaneously. Our possible explanation is that fixing fibular fracture with a plate may act as a lateral buttress, thus increasing fixation stiffness and preventing valgus collapse of the tibia. This would create a biomechanical environment prone to fracture healing and it would cause the tibial plate to be less dependent on the working length of the construct itself.
Screw density proximally to the fracture site was also evaluated. In our series lower screw density positively correlated with the velocity of callus formation. In patients with an mRUST score > 8 three months post-surgery, a significant lower screw density was noticed. It has been proven that the higher it is the distance between each screw the higher the pull-out force acting on the screws, making the construct less prone to failure and promoting callus formation [4]. However, our results are not aligned with the studies of Harvin et al. and Rodriguez et al. In both these studies the authors found no correlation between screw density and union rates [8, 11]. Nevertheless, a recent study from Jang et al. compared two types of proximal fixation in distal femur plating, namely scattered fixation, in which screws were distant from one another, and clustered fixation, in which screws were spanned over a short segment of the plate. The authors argue that scattering the proximal screws contributed to achieve earlier and more balanced radiographic union in unilateral plating of distal femoral fractures [19].
96.9% of all patients reached uneventful bone healing. Complication rate (nonunions and infections) was 7.1% which is lower than previously reported in literature [20,21,22]. This can be attributed to the fact open fractures were excluded in our series. Also, many distal tibia fractures undergo a staged treatment at our institution using a temporary external fixator. Finally, in our series the vast majority (34 out of 42) of the patients was treated using minimally invasive approaches and percutaneous application of the implants. MIPO is well known to reduce nonunion risks especially in tibia fractures [23, 24].
Our study has some inherent limitations. First, it is a retrospective study with a limited number of patients. Second, the treatment is not standardized as the two surgeons were free to choose the construct and both simple and comminuted fractures were included. Third, in our series 32 patients reached an mRUST score > 8 at 3 months post-surgery, while only 10 patients didn’t, which is a factor that decreases the power of our statistics. Finally callus formation was assessed on plain film, while a CT scan would have been more accurate. However, unlike in previous clinical studies, we treated our patients with the same tibial plate in titanium, thus avoiding implant selection bias.
Conclusion
Our findings show that in distal tibia fractures fixed with a medial bridge plate a low screw density is associated with faster callus formation. Conversely, no association was noticed between working length and velocity of callus formation. Our explanation is that in distal tibia fractures—both with intact fibula and where fibula is fixed—the fibula itself acts as a lateral buttress, influencing the biomechanics of the tibial bridge plate and making the construct less dependent on its working length. Future clinical studies with a higher number of patients are needed. Studies comparing screw types (cortical, locking or hybrid) may be necessary. Finally, biomechanical tests and finite element analysis may better clarify the role of working length in distal tibia fractures.
References
Sitnik A, Beletsky A, Schelkun S (2017) Intra-articular fractures of the distal tibia: current concepts of management. EFORT Open Rev 2(8):352–361. https://doi.org/10.1302/2058-5241.2.150047
Wagner M, Frigg R (2006) AO manual of fracture management: internal fixators concept and cases using LCP and LISS. Thime, New York
Chen G, Schmutz B, Wullschleger M, Pearcy MJ, Schuetz MA (2010) Computational investigations of mechanical failures of internal plate fixation. Proc Inst Mech Eng H 224(1):119–126. https://doi.org/10.1243/09544119JEIM670
Gautier E, Sommer C (2003) Guidelines for the clinical application of the LCP. Injury 34(suppl. 2):B63-76. https://doi.org/10.1016/j.injury.2003.09.026
Harvin WH, Oladeji LO, Della Rocca GJ, Murtha YM, Volgas DA, Stannard JP, Crist BD (2017) Working length and proximal screw constructs in plate osteosynthesis of distal femur fractures. Injury 48(11):2597–2601. https://doi.org/10.1016/j.injury.2017.08.064
Whelan DB, Bhandari M, Stephen D, Kreder H, McKee MD, Zdero R, Schemitsch EH (2010) Development of the radiographic union score for tibial fractures for the assessment of tibial fracture healing after intramedullary fixation. J Trauma 68(3):629–632. https://doi.org/10.1097/TA.0b013e3181a7c16d
Plumarom Y, Wilkinson BG, Willey MC, An Q, Marsh L, Karam MD (2021) Sensitivity and specificity of modified RUST score using clinical and radiographic findings as a gold standard. Bone Jt Open 2(10):796–805. https://doi.org/10.1302/2633-1462.210.BJO-2021-0071.R1
Litrenta J, Tornetta P 3rd, Mehta S, Jones C, O’Toole RV, Bhandari M, Kottmeier S, Ostrum R, Egol K, Ricci W, Schemitsch E, Horwitz D (2015) Determination of radiographic healing: an assessment of consistency using RUST and modified RUST in metadiaphyseal fractures. J Orthop Trauma 29(11):516–520. https://doi.org/10.1097/BOT.0000000000000390
Rodriguez EK, Zurakowski D, Herder L, Hall A, Walley KC, Weaver MJ, Appleton PT, Vrahas M (2016) Mechanical construct characteristics predisposing to non-union after locked lateral plating of distal femur fractures. J Orthop Trauma 30(8):403–408. https://doi.org/10.1097/BOT.0000000000000593
Kanchanomai C, Muanjan P, Phiphobmongkol V (2010) Stiffness and endurance of a locking compression plate fixed on fractured femur. J Appl Biomech 26(1):10–16. https://doi.org/10.1123/jab.26.1.10
Kregor PJ, Stannard JA, Zlowodzki M, Cole PA (2004) Treatment of distal femur fractures using the less invasive stabilization system surgical experience and early clinical results in 103 fractures. J Orthop Trauma 18(8):509–520. https://doi.org/10.1097/00005131-200409000-00006
Henderson CE, Kuhl LL, Fitzpatrick DC, Marsh JL (2011) Locking plates for distal femur fractures: is there a problem with fracture healing? J Orthop Trauma 25(suppl. 1):S8-14. https://doi.org/10.1097/BOT.0b013e3182070127
Wenger R, Oehme F, Winkler J, Perren SM, Babst R, Beeres FJP (2017) Absolute or relative stability in minimal invasive plate osteosynthesis of simple distal meta or diaphyseal tibia fractures? Injury 48(6):1217–1223. https://doi.org/10.1016/j.injury.2017.03.005
Piątkowski K, Piekarczyk P, Kwiatkowski K, Przybycień M, Chwedczuk B (2015) Comparison of different locking plate fixation methods in distal tibia fractures. Int Orthop 39(11):2245–2251. https://doi.org/10.1007/s00264-015-2906-4
Perren SM (1979) Physical and biological aspects of fracture healing with special reference to internal fixation. Clin Orthop Relat Res 138:175–196
Lujan TJ, Henderson CE, Madey SM, Fitzpatrick DC, Marsh JL, Bottlang M (2010) Locked plating of distal femur fractures leads to inconsistent and asymmetric callus formation. J Orthop Trauma 24(3):156–162. https://doi.org/10.1097/BOT.0b013e3181be6720
MacLeod AR, Pankaj P (2018) Pre-operative planning for fracture fixation using locking plates: device configuration and other considerations. Injury 49:S12–S18. https://doi.org/10.1016/S0020-1383(18)30296-1
Parks C, McAndrew CM, Spraggs-Hughes A, Ricci WM, Silva MJ, Gardner MJ (2018) In-vivo stiffness assessment of distal femur fracture locked plating constructs. Clin Biomech 56:46–51. https://doi.org/10.1016/j.clinbiomech.2018.05.012
Jang JH, Rhee SJ, Bin Jun S, Choi YY (2022) Scattering and clustering the proximal screw construct in unilateral locking plate osteosynthesis of distal femoral fractures. Arch Orthop Trauma Surg 142(9):2193–2203. https://doi.org/10.1007/s00402-021-03912-1
Neumann MV, Strohm PC, Reising K, Zwingmann J, Hammer TO, Suedkamp NP (2016) Complications after surgical management of distal lower leg fractures. Scand J Trauma Resusc Emerg Med 24(1):146. https://doi.org/10.1186/s13049-016-0333-1
McCann PA, Jackson M, Mitchell ST, Atkins RM (2011) Complications of definitive open reduction and internal fixation of pilon fractures of the distal tibia. Int Orthop 35(3):413–418. https://doi.org/10.1007/s00264-010-1005-9
Bacon S, Smith WR, Morgan SJ, Hasenboehler E, Philips G, Williams A, Ziran BH, Stahel PF (2008) A retrospective analysis of comminuted intra-articular fractures of the tibial plafond: open reduction and internal fixation versus external Ilizarov fixation. Injury 39(2):196–202. https://doi.org/10.1016/j.injury.2007.09.003
Tian R, Zheng F, Zhao W, Zhang Y, Yuan J, Zhang B, Li L (2020) Prevalence and influencing factors of nonunion in patients with tibial fracture: systematic review and meta-analysis. J Orthop Surg Res 15(1):377. https://doi.org/10.1186/s13018-020-01904-2
Andalib A, Sheikhbahaei E, Andalib Z, Tahririan MA (2017) Effectiveness of minimally invasive plate osteosynthesis (MIPO) on comminuted tibial or femoral fractures. Arch Bone Jt Surg 5(5):290–295
Funding
Open access funding provided by Università degli Studi di Milano within the CRUI-CARE Agreement. This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
The study above comply with the current laws of the country in which they were performed (Italy). The study received IRB (Comitato Etico Milano Area 1, ASST Santi Paolo e Carlo) approval prior to retrospective analysis.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gilli, A., Ghirardelli, S., Pozzi, P. et al. Do working length and proximal screw density influence the velocity of callus formation in distal tibia fractures treated with a medial bridge plate?. Eur J Orthop Surg Traumatol 34, 523–528 (2024). https://doi.org/10.1007/s00590-023-03697-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-023-03697-6