Abstract
Purpose
This systematic review and meta-analysis aimed to compare the outcomes of total hip arthroplasty (THA) in patients with developmental dysplasia of the hip (DDH) and those with osteoarthritis (OA).
Methods
Four databases were searched from inception till February 2023 for original studies that compared the outcomes of THA in DDH and OA. The primary outcome was the revision rate; the secondary outcomes were dislocation and failure modes (i.e. aseptic loosening, PJI, instability, and periprosthetic fractures), hospital stay and costs. This review was conducted as per PRISMA guidelines, and the risk of bias was assessed using the Newcastle–Ottawa scale.
Results
A total of 9 observational studies with 575,255 THA (469,224 hips) were included, with a mean age of 50.6 years and 62.1 years for DDH and OA groups, respectively. There was a statistically significant difference in revision rate between DDH and OA patients in favour of OA (OR, 1.66; 95% CI 1.11–2.48; p-value, 0.0251). However, dislocation rate (OR, 1.78, 95% CI 0.58–5.51; p-value, 0.200), aseptic loosening (OR, 1.69; 95% CI 0.26–10.84; p-value, 0.346) and PJI (OR, 0.76; 95% CI 0.56–1.03; p-value, 0.063) were comparable across both groups.
Conclusion
A higher revision rate following total hip arthroplasty was associated with DDH compared with osteoarthritis. However, both groups had similar dislocation rates, aseptic loosening and PJI. Consideration of confounding factors, such as patient age and activity level, is crucial when interpreting these findings.
Level of evidence
III.
Trial registration
PROSPERO registration: CRD42023396192.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Introduction
Total hip arthroplasty (THA) is a frequently performed surgical intervention to alleviate hip pain and dysfunction when non-operative measures have failed. There are estimated to be more than 500,000 annual THA cases in the USA alone [1]. Primary hip osteoarthritis (OA) and developmental dysplasia of the hip (DDH) are the two most common etiologists for THA [2,3,4,5,6]. DDH is a spectrum of diseases that ranges from a shallow acetabulum to a complete dislocation of the femoral head. This condition results in acetabular and femoral changes that disrupt the normal hip anatomy and biomechanics, making DDH the leading cause of secondary hip osteoarthritis requiring THA. In addition, DDH is responsible for 20% of all THA in patients younger than 50 years [7], thus, posing a significant burden on patients and the entire healthcare system.
Given the complexity of DDH and associated challenges, the long-term consequences, potential complications, and success rate of THA in such cases remain debatable. While some studies showed satisfactory and good clinical outcomes, others reported inferior long-term results and higher revision rates [8].
To the best of our knowledge, no previous systematic reviews have directly assessed the long-term outcomes and safety of THA in DDH versus osteoarthritis. Therefore, this study aimed to review and compare the clinical outcomes of THA in patients with DDH to those with hip OA. This meta-analysis hypothesises that THA in patients with DDH has inferior clinical outcomes and higher complication and revision rates.
Methods
This systematic review adhered to the guidelines provided by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [9]. The review protocol was registered in advance on the International Prospective Register of Systematic Reviews (PROSPERO) with the Registration Number CRD42023396192.
Search strategy
A comprehensive search was conducted across several databases, including PubMed/Medline, Ovid, Google Scholar, and the Cochrane Library. The search encompassed the entire available literature up until February 2023, using a combination of specific keywords and their variations. The keywords used were “Total hip replacement” OR “Total hip arthroplasty”, “Developmental dysplasia of the hip”, “Osteoarthritis”, and “Outcomes.” The search results were initially screened by two authors independently, who assessed the relevance based on each article’s title and/or abstract. In case of disagreements, a meeting involving a third, more senior author was held to resolve any conflicts. A thorough review of the full-text articles that met the eligibility criteria was conducted following the initial screening. Additionally, the reference lists of these selected articles were manually examined to ensure that all relevant studies were included in the analysis.
Outcomes of interest
The primary outcome was the revision rate, defined by the National joint registry consensus as “Any operation performed to add, remove or modify one or more components of a joint replacement” [10]. The number of dislocations, modes of failure (i.e. aseptic loosening, PJI, instability, and periprosthetic fractures), hospital stay and costs were used as secondary outcomes of interest.
Eligibility criteria
Inclusion criteria
-
1.
All original comparative, RCTs and observational studies reporting the outcome of THR in Hip dysplasia or primary OA.
-
2.
Studies with a minimum follow-up period of 1 year.
-
3.
All types of THR prosthesis designs.
Exclusion criteria
-
1.
Studies with different indications for THR other than hip dysplasia or OA
-
2.
Noncomparative or not reporting outcomes or failures by subgroups (i.e. DDH vs OA)
-
3.
Review articles, cross-sectional, preclinical studies, case series and reports
-
4.
Studies with incomplete or unextractable data
-
5.
Studies published in languages other than English
Data extraction and items
Two independent reviewers used a pre-defined Microsoft Excel data collection sheet to extract relevant data. The extracted data encompassed various demographic aspects, such as the surname of the first authors, study year, design and location, mean patient age, number of participants and hips, age, type of total hip replacement (THR) (including cementless and cemented), type of prosthesis and bearings used, mean follow-up period, number of revisions, complications, modes of revisions, hospital stays, costs, statistical tests employed, and the conclusion of each study.
Qualitative assessment (Risk of bias)
Two authors assessed the methodological quality of the included studies using the Newcastle–Ottawa tool, which comprises three key domains; patient selection, comparability, and outcomes [11, 12]. A higher overall score indicates a lower risk of bias; a score of 5 or less (out of 9) corresponds to a high risk of bias.
Quantitative analysis
A meta-analysis of eligible studies using R software (version 4.0.2, R Core Team, Vienna, Austria, 2020), particularly the meta package (i.e. forest_meta and metabin), was performed. Odds ratios (OR) and their associated 95% confidence intervals were expressed for dichotomous variables (e.g. rate of revisions). Heterogeneity among effect sizes was evaluated using the I-squared statistic. Definitions for heterogeneity were adapted from the Cochrane Handbook (> 25% mild, 25–50% moderate, > 50% severe). Due to the high heterogeneity for the dichotomous variables, a random-effects model was utilized. Both a funnel plot and Egger’s test of asymmetry were used to assess publication bias.
Results
Study selection
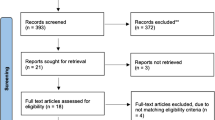
Rayyan AI website was used to manage the literature search results [13]. Searching the databases yielded 367 articles, and after removing 98 duplicates, 269 records were screened by title and abstracts, of which 254 were excluded. A total of 15 papers were eligible for a full-text review. As a result, 9 studies met the eligibility criteria and were included in the qualitative and quantitative synthesis. The PRISMA flowchart is displayed in Fig. 1.
Study characteristics
A total of 9 articles investigating the impact of total hip arthroplasty (THA) on patients with developmental dysplasia of the hip (DDH) and osteoarthritis (OA) were included. The included studies were published during the time period from 2008 to 2022. Included publications were primarily from the United States of America (n = 3), Denmark, Norway and Sweden (n = 3), New Zealand (n = 2), and Iran (n = 1). These studies were entirely cohort-based, of which 8 were retrospective and 1 was prospective (Table 1).
A total of 575,255 THA procedures were recorded across the included studies. A total of 469,224 hips were examined. Altogether, 23,072 hips with DDH were examined while 445,894 hips with OA were pooled. The mean age for participants with DDH was 50.6 years, while participants with OA had a mean age of 62.1 years. The pooled number of participants were followed up for anywhere between 4.6 and 42.3 years.
Quality assessment (risk of bias and level of evidence (LoE))
Following OCEBM criteria [14], one study was level 2b and eight were level 3a (Table 1), with an overall grade B of recommendation assigned to the review [15]. The Newcastle–Ottawa scores of all 9 observational studies ranged from 6 to 8, with an average of 7 ± 0.67, indicating a low overall risk of bias. A summary of the qualitative assessment, using the Newcastle–Ottawa scale, is displayed in Table 2.
Outcome results
The impact of THA on DDH and OA were examined through a number of outcome measures including number of revisions, number of dislocations, and modes of treatment failure (i.e. aseptic loosening, PJI, instability, and periprosthetic fractures). In terms of revisions, patients with DDH are 1.66 times more likely to have revisions than their OA counterparts (OR, 1.66; 95% CI 1.11–2.48; p-value, 0.0251) (Refer to Fig. 2). On the other hand, a total of 4 studies reported on number of dislocations and demonstrated that patients with DDH are 1.78 times more likely to experience dislocations; however, such difference is statistically insignificant (OR, 1.78, 95% CI 0.58–5.51; p-value, 0.200) (Refer to Fig. 3).
With respect to modes of failure, only aseptic loosening and PJI were eligible for quantitative analysis reported by 3 studies each. Patients with DDH were 1.69 more likely to have aseptic loosening (OR, 1.69; 95% CI 0.26–10.84) and were 0.76 times less likely to have PJI (OR, 0.76; 95% CI 0.56–1.03) (Refer to Figs. 4 and 5). However, both rates were statistically insignificant (p-value, 0.346 and 0.063, respectively). In addition, no studies reported on instability while only one study reported on periprosthetic fractures (PPF). Thillemann et al. (2008) reported 4 and 109 PPF incidents among 1455 patients with DDH and 53,694 patients with OA, respectively.
Three studies reported on hospital stay and hospital costs associated with THA (Ashraf 2014, Aggarwal 2019, and Siddiqi 2020). Hospital stays for patients undergoing THA ranged from 3 to 11 days. Moreover, hospital costs ranged from 16,949$ to 28,207$ for patients with DDH, and from 16,485$ to 27,078$ for patients with OA.
Discussion
The most significant findings of this systematic review and meta-analysis were that the revision rate was significantly higher following THA for DDH than for primary OA. Another important finding was that patients with DDH were more likely to have dislocations and aseptic loosening; however, such differences were statistically insignificant. Additionally, Hospital stay and hospital costs were comparable.
Revision
This study found a significant increase in revision procedures among the DDH group following their initial surgery compared to THA for primary OA. This finding is consistent with some previous studies. Engesæter12 et al. [16] have postulated that patients with DDH have an increased overall risk of revision within the first six months postoperatively in comparison to patients with OA. However, the higher revision rate was not sustained, and there was no significant difference after the first six months. The authors attributed this finding to the fact that dislocation was significantly higher in DDH than for OA within the first six months [16]. The authors have also reported no difference in the risk of revision due to aseptic loosening or infection [16].
Thillemann et al. [17] and Boyle et al. [18] reported a higher rate of revision favouring OA, but the difference was not statistically significant. Meanwhile, Siddiqi et al. [8] reported comparable results across both groups. The reasons for these findings are not clearly defined, and caution should be exercised when interpreting these results due to significant heterogeneity among the studies. Factors such as pooling mild and severe dysplasia groups likely underestimate the risks of revision associated with THA for severe dysplasia and may have played a role in the differences observed between studies [2]. Additionally, DDH patients are often younger and more active than those with primary OA and may have higher expectations for their postoperative function and activity levels. This may lead to revision surgery being offered more readily in this population, compared to older patients with primary OA who may have multiple co-morbidities that could make revision surgery less feasible or desirable.
Dislocations
Four studies were included in this meta-analysis that investigated the dislocation rate between both cohorts. The cohort undergoing THA for DDH demonstrated an overall statistically insignificant higher dislocation rate than OA patients. This increased risk of dislocation in THA after DDH is probably to be expected since DDH patients often have extreme anteversion of the proximal femur, which governs the anteversion of the femoral component and thereby increases the risk of anterior dislocation. Mortazavi et al. reported that the dislocation rate was significantly higher in the DDH group than in the primary OA group [19]. Furthermore, a univariate analysis in the same study indicated an increase in the dislocation rate in relation to the severity and grade of DDH. Similarly, a significant increase in dislocation rate was also observed in two other studies [2, 16]. This can be due to a dysplastic acetabulum, a narrow femur, shortening, rotational deformity, and previous surgeries can further contribute to the risk of dislocation. The altered anatomy can lead to a technically challenging THA with a higher likelihood of dislocation. Further, it is essential to consider the risk of dislocation as a significant factor when assessing the overall revision rate.
Aseptic loosening
The cohort undergoing THA for DDH revealed a statistically insignificant higher aseptic loosening than the OA group. While earlier studies have shown a higher risk of aseptic loosening of the acetabular component following THA surgery in patients with DDH [20, 21], it is essential to note that the difference was not statistically significant in this meta-analysis. This suggests that the risk of aseptic loosening may have decreased over time as improvements in surgical technique and prosthetic design have been made.
The inclusion of a large sample size, long follow-up periods, and high-quality studies with low risk of bias were key strengths that bolstered the external validity and generalizability of our findings. Additionally, the incorporation of various total hip replacement (THR) prosthesis designs (hybrid, cementless, and cemented) further contributed to the robustness of our results.
However, it is important to acknowledge several limitations. Firstly, the analysis of the developmental dysplasia of the hip (DDH) cohort encompassed a range of presentations, from dysplasia to dislocation. Conducting subgroup analyses based on specific DDH morphological severity would have mitigated the heterogeneity of this condition and its potential impact on the overall outcome of THA. Unfortunately, limited studies and inconsistent reporting of DDH in the literature hindered the feasibility of this approach.
Another potential limitation was the inadequate reporting of factors that could influence the outcomes of THR, such as implant type and surgical factors [22, 23]. Moreover, future research should prioritize prospective studies to better control for these confounding factors and to evaluate this issue in a statistically robust manner.
Conclusion
This study demonstrated a significantly higher revision rate in patients with DDH following total hip arthroplasty compared to patients with primary osteoarthritis. However, dislocation rates, aseptic loosening and PJI were comparable. This finding should be applied in context given the heterogeneity of patients and confounding factors.
Data availability
Not applicable. However, happy to provide access to any statistical data (coding) upon request.
References
Aggarwal VK, Suh YM, Hutzler L, Moscona L, Castañeda P (2019) Total hip arthroplasty for secondary causes of arthritis an increase in time and money. Bull Hosp Jt Dis 77(4):233–237
Engesaeter LB, Furnes O, Havelin LI (2008) Developmental dysplasia of the hip–good results of later total hip arthroplasty: 7135 primary total hip arthroplasties after developmental dysplasia of the hip compared with 59774 total hip arthroplasties in idiopathic coxarthrosis followed for 0–15 years in the Norwegian Arthroplasty Register. J Arthroplasty 23(2):235–240. https://doi.org/10.1016/j.arth.2007.03.023
Harris WH (1986) Etiology of osteoarthritis of the hip. Clin Orthop 213:20
Albinana J, Dolan LA, Spratt KF et al (2004) Acetabular dysplasia after treatment for developmental dysplasia of the hip. Implications for secondary procedures. J Bone Jt Surg Br 86:876
Hasegawa Y, Iwata H, Mizuno M et al (1992) The natural course of osteoarthritis of the hip due to subluxation or acetabular dysplasia. Arch Orthop Trauma Surg 11:187
Jacobsen S, Sonne-Holm S, Søballe K et al (2005) Hip dysplasia and osteoarthrosis. A survey of 4151 subjects from the osteoarthrosis substudy of the Copenhagen city heart study. Acta Orthop 76:149
Ashraf A, Larson AN, Maradit-Kremers H, Kremers WK, Lewallen DG (2014) Hospital costs of total hip arthroplasty for developmental dysplasia of the hip. Clin Orthop Relat Res 472(7):2237–2244. https://doi.org/10.1007/s11999-014-3587-9
Siddiqi A, White PB, Sloan M, Fox D, Piuzzi NS, Sankar WN, Sheth NP (2020) Total hip arthroplasty for developmental dysplasia of hip vs osteoarthritis: a propensity matched pair analysis. Arthroplasty today 6(3):607-611.e1. https://doi.org/10.1016/j.artd.2020.02.018
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 62:1006–1012
Registry NJ (2020) National Joint Registry 17th Annual Report. https://www.njrcentre.org.uk. Accessed 01 June 2021
Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P (2013) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 29 Jan 2023
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25(9):603–605. https://doi.org/10.1007/s10654-010-9491-z
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A (2016) Rayyan—a web and mobile app for systematic reviews. Syst Rev 5:210
OCEBM Levels of Evidence Working Group (2011) The Oxford levels of evidence 2. https://www.cebm.net/index.aspx?o=5653. Accessed 10 Dec 2022
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso- Coello P et al (2008) GRADE: an emerging consensus on rat- ing quality of evidence and strength of recommendations. BMJ 336(7650):924–926
Engesæter LB, Engesæter IØ, Fenstad AM, Havelin LI, Kärrholm J, Garellick G, Pedersen AB, Overgaard S (2012) Low revision rate after total hip arthroplasty in patients with pediatric hip diseases. Acta Orthop 83(5):436–441. https://doi.org/10.3109/17453674.2012.736171
Thillemann TM, Pedersen AB, Johnsen SP, Søballe K, Registry DHA (2008) Implant survival after primary total hip arthroplasty due to childhood hip disorders: results from the Danish Hip Arthroplasty Registry. Acta Orthop 79(6):769–776. https://doi.org/10.1080/17453670810016830
Boyle MJ, Singleton N, Frampton CM, Muir D (2013) Functional response to total hip arthroplasty in patients with hip dysplasia. ANZ J Surg 83(7–8):554–558. https://doi.org/10.1111/j.1445-2197.2012.06198.x
Mortazavi SMJ, Ghadimi E, Ardakani MV, Razzaghof M, Ghasemi MA, Nili A, Vafaei A, Moharrami A, Rasta S (2022) Risk factors of dislocation after total hip arthroplasty in patients with developmental dysplasia of the hip. Int Orthop 46(4):749–759. https://doi.org/10.1007/s00264-021-05294-w
MacKenzie JR, Kelley SS, Johnston RC (1996) Total hip replacement for coxarthrosis secondary to congenital dysplasia and dislocation of the hip. Long-term results. J Bone Jt Surg (Am) 78:55–61
Sochart DH, Porter ML (1997) The long-term results of Charnley low-friction arthroplasty in young patients who have congenital dislocation, degenerative osteoarthrosis, or rheumatoid arthritis. J Bone Jt Surg (Am) 79:1599–1617
Salvati EA, Cornell CN (1988) Long-term follow-up of total hip replacement in patients with avascular necrosis. Instr Course Lect 37:67–73
Xenakis TA, Beris AE, Malizos KK, Koukoubis T, Gelalis J, Sou- cacos PN, (1997) Total hip arthroplasty for avascular necrosis and degenerative osteoarthritis of the hip. Clin Orthop 341:62–68
Boyle MJ, Frampton CM, Crawford HA (2012) Early results of total hip arthroplasty in patients with developmental dysplasia of the hip compared with patients with osteoarthritis. J Arthroplasty 27(3):386–390. https://doi.org/10.1016/j.arth.2011.06.024
Acknowledgements
None
Funding
Open Access funding provided by the Qatar National Library.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, literature review, data collection and quality assessment were performed by LAS, OZA, ATH. Statistical analysis was performed by AA. The first draft of the manuscript was written by LAS, OZA, ATH, GA, and all authors commented on the previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent to participate
Not applicable.
Consent for publications
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Salman, L.A., Alzobi, O.Z., Al-Ani, A. et al. The outcomes of total hip arthroplasty in developmental dysplasia of hip versus osteoarthritis: a systematic review and meta-analysis. Eur J Orthop Surg Traumatol 34, 1–8 (2024). https://doi.org/10.1007/s00590-023-03635-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-023-03635-6