Abstract
Purpose
We investigated bacterial propagation through multifilament, monofilament sutures and whether sutures coated with triclosan would exhibit a different phenomenon.
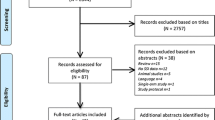
Methods
One centimetre (cm) wide trenches were cut in the middle of Columbia blood Agar plates. We tested a 6 cm length of two Triclosan-coated (PDS plus®, Vicryl plus®) and two uncoated (PDS ®, Vicryl ®) sutures. Each suture was inoculated with a bacterial suspension containing methicillin-sensitive Staphylococcus aureus (MSSA), Escherichia coli (E. coli), Staphylococcus epidermidis, methicillin-resistant Staphylococcus aureus (MRSA) at one end of each suture. The plates were incubated at 36C for 48 h, followed by room temperature for a further 5 days. We established bacterial propagation by observing for any bacterial growth on the Agar on the opposite side of the trench.
Results
Bacterial propagation was observed on the opposite side of the trench with both suture types, monofilament PDS and multifilament Vicryl, when tested with the motile bacterium (E. coli). Propagation was not observed on the other side of the trench with the monofilament PDS suture following incubation with MSSA and S. epidermidis, and in 66% of MRSA. With multifilament suture Vicryl, propagation was observed on the other side of the trench in 90% (MSSA), 80% (S. epidermidis), and 100% (MRSA) of plates tested. No bacterial propagation was observed in any of the triclosan-coated sutures (monofilament or multifilament).
Conclusions
Monofilament sutures are associated in vitro with less bacterial propagation along their course when compared to multifilament sutures. Inhibition in both sutures can be further enhanced with a triclosan coating.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Postoperative surgical site infection (SSI) following spinal surgery is a serious complication, with incidence rates reported to be up to 16% [1,2,3,4]. SSIs are reported to be the third most common complication of spinal surgery [5,6,7]. They are associated with significant morbidity and have a heavy economic burden [8]. In the USA, the direct and indirect health care costs associated with SSIs were reported to reach up to 10 billion USD, with up to 8000 death per year [9].
The Gram-positive bacteria (Staphylococci, Streptococci, Enterococci, Propionibacterium) are the most common organisms responsible for spinal SSI. Among the Gram positive bacteria, Staphylococcus aureus and Staphylococcus epidermis account for the majority of isolated organisms. The less common gram-negative bacteria, such as Pseudomonas aeruginosa, Escherichia coli, and Proteus species, may account for up to one-third of cases of spinal SSI [10,11,12,13,14].
Researchers have looked at modifiable risk factors with the aim of improving rates of SSI post-spinal surgery [15]. For example, Masaki et al. assessed the effect of triclosan-coated sutures on wound infections following spinal surgery, reporting that their use may reduce the incidence of postoperative SSI [16]. Furthermore, suture material can change the susceptibility to bacterial infections in surgical wounds [17]. Suture products have evolved over the years from natural to synthetic, in monofilament and multifilament forms with the synthetic multifilament Vicryl (Ethicon-Johnson & Johnson Medical Limited, Ohio, USA), ubiquitously used across the surgical specialities [18]. Both types (monofilament, multifilament) of sutures have their advances and disadvantages. Monofilament sutures require careful handling and tying. There is a risk of crushing or crimping of the suture can nick or weaken it which can lead to undesirable and suture failure. Multifilament sutures generally have greater tensile strength and better pliability and have relative greater flexibility in comparison with monofilament suture material. In addition, multifilament sutures have superior handling properties. In general, which suture is used depends on the surgeon’s preference.
Recent suture research has focused on triclosan-coated multifilament sutures (Ethicon, Somerville, New Jersey) [16, 18, 19]. Several high-profile organisations, such as the World Health Organisation (WHO), and National Institute for Health and Care Excellence (NICE), have been advocating the use of triclosan-coated sutures [20, 21]. Noticeably, the published literature about these sutures varies in their reported outcomes. Some recommend their use whilst other studies showed no statistical significance associated with their use [16, 18, 19].
To date, only one historic paper published in 1977 has quantitatively assessed the phenomena of bacterial transport through different suture materials [22]. Their experiments were conducted both in laboratory and rat models, using monofilaments and multifilament sutures. The researchers concluded that the tested immobile bacteria, Staphylococcus aureus, were transported inside multifilament materials. Similar results were obtained in their in vivo arm of the study in rats’ muscles. Bacterial transport was not observed through the monofilament sutures. The sutures used during the 1977 study are not currently in use.
Our aim was to investigate bacterial propagation through monofilament, multifilament sutures, and those coated with triclosan, using contemporary sutures in an in vitro, laboratory-based study. We used some of the commonly encountered bacteria associated with spinal surgical site infections (SSI) [23,24,25,26]. We hypothesised that synthetic monofilament sutures would be associated with less risk of bacterial propagation through suture strands in comparison with synthetic multifilament sutures. In addition, triclosan coating might have a synergistic effect to reduce bacterial propagation further.
Materials and methods
Suture material
The following suture materials were tested: PDS (Polydioxanone) size 1, PDS Plus size 1; Vicryl (Polyglactin 910) size 2.0, and Vicryl Plus size 2.0 (Ethicon-Johnson & Johnson Medical Limited).
PDS is a synthetic absorbable monofilament suture. It elicits minimal tissue reaction. It retains 80% of its strength by 14 days, 70% by 28 days, and 60% by 42 days. Absorption is essentially complete in 182–238 days [27].
Vicryl is a synthetic absorbable multifilament that elicits minimal acute inflammatory reaction. It retains 75% of its tensile strength at two weeks post-implantation, and 50% at three weeks. All the original tensile strength is lost between 4–5 weeks post-implantation. Absorption is essentially complete by 56–70 days [27].
The PDS Plus and Vicryl Plus sutures contained antibacterial Triclosan in the form of Irgacare® MP ≤ 2360 μg/m, and ≤ 472 μg/m, respectively [28].
Triclosan is an antimicrobial agent that has a broad range of activity against many Gram-positive, Gram-negative bacteria, and some fungi. Triclosan is bacteriostatic at low concentrations, but higher levels are bactericidal [29].
Methods
Petri dishes containing Columbia blood Agar (Sheep blood 5%) from Liofilchem® were used. A one centimetre (cm) wide trench was cut with a sterile scalpel in the middle of the agar plate. This trench created a complete gap in the agar plate to prevent bacterial spread from one side of the trench to the other directly through the agar.
A 6 cm length of each type of suture was placed on the Petri dish across the trench. A saline solution containing 0.5 McFarland bacterial suspensions was prepared. The 0.5 McFarland turbidity standard provides an optical density comparable to the density of a bacterial suspension with a 1.5 × 108 colony forming units (CFU/ml). The bacterial suspension used included one of the following four organisms: methicillin-sensitive Staphylococcus aureus (MSSA), (American Type Culture Collection (ATCC) Virginia, USA) ATCC29213; Escherichia coli ATCC25922; Staphylococcus epidermidis ATCC12228; Methicillin-resistant Staphylococcus aureus (MRSA) ATCC213300. In total, 80μL of a single bacterial suspension was inoculated to one end of each suture, in instalments of 20 μL every 30 min. Inoculation of the bacterial suspension was performed in a biosafety cabinet. The plates were incubated at 36 °C for 48 h and subsequently were kept at room temperature for a further five days.
We observed macroscopically for any presence of bacterial growth on the agar on the opposite side of the trench to establish any tracking/transfer of the organism. For sutures coated with triclosan, we also observed for the presence of a bacterial growth inhibition zone. We continued to observe whether the zone of growth inhibition was sustained until day seven.
Statistical analysis
Undertaken using Fisher’s exact test for categorical data. Statistical significance was set at p ≤ 0.05, and statistical analyses were calculated using IBM SPSS Statistics, Version 26.
Results
Monofilament PDS in comparison with multifilament Vicryl sutures without triclosan
Propagation was observed onto the other side of the trench with both suture types with E. coli (100%). This was not observed on the other side of the trench with the majority of monofilament (PDS) sutures following incubation with MSSA, S. epidermidis, and MRSA.
Propagation was observed on the other side of the trench in the vast majority with multifilament Vicryl sutures following incubation with MSSA, S. epidermidis, and MRSA (Table 1).
Triclosan-coated sutures (PDS plus and Vicryl plus)
Sutures with triclosan coating showed broad bacteria inhibition zones around them (Figs. 1, 2, 3, 4, 5, 6, 7, 8). Propagation onto the other side of the trench was not observed with the tested organisms (E. coli, MSSA, MRSA, and S. epidermidis). The results are presented in Tables 2 and 3. The inhibition of bacterial growth was retained up to seven days of incubation. No statistically significant difference was found between the triclosan-coated PDS Plus and the Vicryl Plus sutures.
Discussion
To the best of our knowledge, this is the first study investigating bacterial propagation through monofilament PDS and multifilament Vicryl sutures, with and without triclosan coating. We used a variable selection of commonly encountered organisms in orthopaedics SSIs [23,24,25,26]. The tested non-motile bacteria were able to propagate through multifilament sutures to the other side of the trench. This was not observed in the majority of the tested monofilament sutures. The absence of propagation associated with the monofilament suture was not retained when motile bacteria were tested as both sutures showed propagation when E.coli was tested.
Our study is not without limitations. Confounding variables such as suture material, structure, and capillarity may influence the observed bacterial propagation differences between the PDS monofilament and Vicryl multifilament sutures [17]. The PDS monofilament sutures are made from the polyester (p-dioxanone). The Vicryl multifilament sutures are from a copolymer, Polyglactin 910 which is composed of 90% glycolide, 10% l-lactide and calcium stearate. Monofilament sutures are single stranded sutures, whereas multifilament sutures are made of several filaments twisted together. Multifilament sutures have narrow tubular inner spaces that can transport bacteria as they transport fluids, similar to a wick [30]. This is due to the capillary ascent phenomenon where fluids can rise in a narrow tube when submerged, as a result of the molecular activity between adjacent bodies [31].
The spread of flagellated bacteria on surfaces can involve millions of bacteria moving together in complex patterns, through collective motion. This includes rapid migration on surfaces in groups through phenomena such as swarming and near-surface swimming [32, 33]. Previous research has also suggested that bacteria can use sutures as a guide rail for movement [30]. Although our study was conducted in vitro and its clinical relevance may be limited, our findings are supported by previous research and animal studies, which suggest that the observed bacterial propagation on suture surfaces can also occur in vivo after spinal operations [22]. Studies on animal models demonstrated that barbed monofilament suture performed similarly to monofilament suture and better than braided suture in terms of bacterial adherence, biofilm formation, and tissue reactivity [34].
We found that neither motile nor non-motile bacteria were able to spread through triclosan-coated sutures. We observed a sustained zone of bacterial growth inhibition around the triclosan-coated sutures throughout the entire duration of our study (168 h) for all types of bacteria tested. The bacterial suspensions used in our study were at a concentration of 1.5 × 108 CFU/ml, as determined by a 0.5 McFarland standard for E. coli. Previous research has also shown that triclosan is able to inhibit bacterial adhesion to sutures for at least 96 h, which is consistent with our findings [35]. However, further studies with longer duration are needed to determine how long this inhibition is sustained.
Our study found that monofilament sutures have a reduced risk of bacterial propagation compared to multifilament sutures. However, adding a triclosan coating to the suture may provide additional protection, especially against motile Gram-negative bacteria, which can cause up to one-third of spinal SSIs [36]. However, it is important to note that triclosan is not effective against all types of bacteria and resistance in some organisms has been documented [29, 37, 38]. Therefore, using monofilament sutures coated with triclosan could provide additional protection against susceptible bacteria and act as a secondary defence mechanism against the spread of infection in case of a resistant bacteria.
Bacteria can colonise sutures as they are implanted, potentially developing a biofilm, a complex and well-structured aggregation of microorganisms of single or multiple species [39, 40]. Biofilm associated infection is one of the most common causes of failure of orthopaedics and Spinal operations [40]. While animal studies have demonstrated rapid (minutes to hours) biofilm formation, some studies suggest that biofilm formation may also not correlate with the onset of infection [40]. The biofilm formed in suture knots, for example, can lie dormant for years, further highlighting the need for longer-tern studies [41].
Analysis of biofilm formation and electronic microscopy were not implemented in this study, but may form essential aspects of further research to identify biofilm formation and microscopic bacterial propagation through sutures [42]. Future research to improve surgical sutures might benefit from incorporating the biophysical interactions between bacteria and surfaces and assessing whether micro-structuring sutures’ surfaces could mitigate bacterial propagation through them or over their surfaces [32]. Novel surgical sutures may benefit from structural properties that inhibit, and disturb the biofilm formation.
Conclusion
In conclusion, our in vitro study demonstrated that the use of PDS monofilament sutures is associated with a lower likelihood of bacterial propagation along its course when compared to multifilament sutures. This suggests that monofilament PDS sutures may be a more suitable option for closing spinal wounds in order to reduce the risk of postoperative surgical site infections (SSIs). The use of triclosan-coated PDS monofilament sutures could further enhance the benefits of using this type of suture, assuming there are no contraindications [28]. While suture type is just one factor that influences surgical site infection, cumulatively, small improvement in reducing the risk of postoperative complications may lead to significant benefits in the success of spinal operations [43, 44].
Change history
15 April 2023
Corresponding author e-mail address has been updated
References
Ojo OA, Owolabi BS, Oseni AW, Kanu OO, Bankole OB (2016) Surgical site infection in posterior spine surgery. Niger J Clin Pract 19:821–826. https://doi.org/10.4103/1119-3077.183237
Iwakiri K, Kobayashi A, Seki M (1976) Waterless hand rub versus traditional hand scrub methods for preventing the surgical site infection in orthopedic surgery. Spine
Ramo BA, Roberts DW, Tuason D, McClung A, Paraison LE, Moore HG, Sucato DJ (2014) Surgical site infections after posterior spinal fusion for neuromuscular scoliosis: a thirty-year experience at a single institution. J Bone Joint Surg Am 96:2038–2048. https://doi.org/10.2106/JBJS.N.00277
Kim JH, Ahn DK, Kim JW, Kim GW (2015) Particular features of surgical site infection in posterior lumbar interbody fusion. Clin Orthop Surg 7:337–343. https://doi.org/10.4055/cios.2015.7.3.337
Lee MJ, Cizik AM, Hamilton D, Chapman JR (2014) Predicting surgical site infection after spine surgery: a validated model using a prospective surgical registry. Spine J Off J North Am Spine Soc 14:2112–2117. https://doi.org/10.1016/j.spinee.2013.12.026
Lonjon G, Dauzac C, Fourniols E, Guigui P, Bonnomet F, Bonnevialle P, French Orthopaedic Surgery Traumatology Society (2012) Early surgical site infections in adult spinal trauma: a prospective, multicentre study of infection rates and risk factors. Orthop Traumatol Surg Res OTSR 98:788–794. https://doi.org/10.1016/j.otsr.2012.07.006
Saeedinia S, Nouri M, Azarhomayoun A, Hanif H, Mortazavi A, Bahramian P, Yarandi KK, Amirjamshidi A (2015) The incidence and risk factors for surgical site infection after clean spinal operations: a prospective cohort study and review of the literature. Surg Neurol Int 6:154. https://doi.org/10.4103/2152-7806.166194
Anderson PA, Savage JW, Vaccaro AR, Radcliff K, Arnold PM, Lawrence BD, Shamji MF (2017) Prevention of surgical site infection in spine surgery. Neurosurgery 80:S114. https://doi.org/10.1093/neuros/nyw066
Hidron AI, Edwards PJ JR, (2006) NHSN annual update: antimicrobial-resistant pathogens associated with healthcare associated infections: annual summary of data reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention
Abdul-Jabbar A, Berven SH, Hu SS, Chou D, Mummaneni PV, Takemoto S, Ames C, Deviren V, Tay B, Weinstein P, Burch S, Liu C (2013) Surgical site infections in spine surgery: identification of microbiologic and surgical characteristics in 239 cases. Spine 38:E1425-1431. https://doi.org/10.1097/BRS.0b013e3182a42a68
Nasto LA, Colangelo D, Rossi B, Fantoni M, Pola E (2012) Post-operative spondylodiscitis. Eur Rev Med Pharmacol Sci 16(Suppl 2):50–57
Chahoud J, Kanafani Z, Kanj S (2014) Surgical site infections following spine surgery: eliminating the controversies in the diagnosis. Front Med, 1:
Weinstein MA, McCabe JP, Cammisa FP (2000) Postoperative spinal wound infection: a review of 2391 consecutive index procedures. J Spinal Disord 13:422–426. https://doi.org/10.1097/00002517-200010000-00009
Massie JB, Heller JG, Abitbol JJ, McPherson D, Garfin SR (1992) Postoperative posterior spinal wound infections. Clin Orthop 284:99–108
Yao R, Zhou H, Choma TJ, Kwon BK, Street J (2018) Surgical site infection in spine surgery: Who is at risk? Glob Spine J 8:5S-30S. https://doi.org/10.1177/2192568218799056
Ueno M, Saito W, Yamagata M, Imura T, Inoue G, Nakazawa T, Takahira N, Uchida K, Fukahori N, Shimomura K, Takaso M (2015) Triclosan-coated sutures reduce wound infections after spinal surgery: a retrospective, nonrandomized, clinical study. Spine J Off J North Am Spine Soc 15:933–938. https://doi.org/10.1016/j.spinee.2013.06.046
Elek SD, Conen PE (1957) The virulence of Staphylococcus pyogenes for man; a study of the problems of wound infection. Br J Exp Pathol 38:573–586
Sprowson AP, Jensen C, Parsons N, Partington P, Emmerson K, Carluke I, Asaad S, Pratt R, Muller S, Ahmed I, Reed MR (2018) The effect of triclosan-coated sutures on the rate of surgical site infection after hip and knee arthroplasty: a double-blind randomized controlled trial of 2546 patients. Bone Jt J 100B:296–302. https://doi.org/10.1302/0301-620X.100B3.BJJ-2017-0247.R1
Sukeik M, George D, Gabr A, Kallala R, Wilson P, Haddad FS (2019) Randomised controlled trial of triclosan coated vs uncoated sutures in primary hip and knee arthroplasty. World J Orthop 10:268–277. https://doi.org/10.5312/wjo.v10.i7.268
listed N (2016) Global guidelines for the prevention of surgical site infection. World Health Organization, 20 Avenue Appia, 1211 Geneva 27
listed N Plus Sutures for preventing surgical site infection
Blomstedt B, Osterberg B, Bergstrand A (1977) Suture material and bacterial transport. An Exp Study Acta Chir Scand 143:71–73
Cooper K, Lamagni T, Harrington P, Wloch C, England SHPH (2019) Surveillance of surgical site infections in NHS hospitals in England, April 2018 to March 2019. Public Health Engl
Barbolt TA (2002) Chemistry and safety of triclosan, and its use as an antimicrobial coating on Coated VICRYL* plus antibacterial suture (coated polyglactin 910 suture with triclosan). Surg Infect 3(Suppl 1):S45-53. https://doi.org/10.1089/sur.2002.3.s1-45
Rothenburger S, Spangler D, Bhende S, Burkley D (2002) In vitro antimicrobial evaluation of Coated VICRYL* plus antibacterial suture (coated polyglactin 910 with triclosan) using zone of inhibition assays. Surg Infect 3(Suppl 1):S79-87. https://doi.org/10.1089/sur.2002.3.s1-79
Storch ML, Rothenburger SJ, Jacinto G (2004) Experimental efficacy study of coated VICRYL plus antibacterial suture in guinea pigs challenged with Staphylococcus aureus. Surg Infect 5:281–288. https://doi.org/10.1089/sur.2004.5.281
Dunn DL (2007) Wound closure manual. Ethicon Inc, Somerville New Jersey
Ethicon product catalog. Jnjmedicaldevices.com
Russell AD (2004) Whither triclosan? J Antimicrob Chemother 53:693–695. https://doi.org/10.1093/jac/dkh171
Geiger D, Debus E-S, Ziegler UE, Larena-Avellaneda A, Frosch M, Thiede A, Dietz UA (2005) Capillary activity of surgical sutures and suture-dependent bacterial transport: a qualitative study. Surg Infect 6:377–383. https://doi.org/10.1089/sur.2005.6.377
Lexikon der Physik in 10 Bänden. DTV,1970, München
Be’er A, Ariel G (2019) A statistical physics view of swarming bacteria. Mov Ecol 7:9. https://doi.org/10.1186/s40462-019-0153-9
Makarchuk S, Braz VC, Araújo NAM, Ciric L, Volpe G (2019) Enhanced propagation of motile bacteria on surfaces due to forward scattering. Nat Commun 10:4110. https://doi.org/10.1038/s41467-019-12010-1
Markel DC, Bergum C, Wu B, Bou-Akl T, Ren W (2019) Does suture type influence bacterial retention and biofilm formation after irrigation in a mouse model? Clin Orthop 477:116–126. https://doi.org/10.1097/CORR.0000000000000391
Edmiston CE, Seabrook GR, Goheen MP, Krepel CJ, Johnson CP, Lewis BD, Brown KR, Towne JB (2006) Bacterial adherence to surgical sutures: can antibacterial-coated sutures reduce the risk of microbial contamination? J Am Coll Surg 203:481–489. https://doi.org/10.1016/j.jamcollsurg.2006.06.026
Long DR, Bryson-Cahn C, Pergamit R, Tavolaro C, Saigal R, Chan JD, Lynch JB (2021) Young investigator award winner: anatomic gradients in the microbiology of spinal fusion surgical site infection and resistance to surgical antimicrobial prophylaxis. Spine 46:143–151. https://doi.org/10.1097/BRS.0000000000003603
D’Arezzo S, Lanini S, Puro V, Ippolito G, Visca P (2012) High-level tolerance to triclosan may play a role in Pseudomonas aeruginosa antibiotic resistance in immunocompromised hosts: evidence from outbreak investigation. BMC Res Notes 5:43. https://doi.org/10.1186/1756-0500-5-43
Welsch TT, Gillock ET (2011) Triclosan-resistant bacteria isolated from feedlot and residential soils. J Environ Sci Health Part A Tox Hazard Subst Environ Eng 46:436–440. https://doi.org/10.1080/10934529.2011.549407
Kathju S, Nistico L, Tower I, Lasko L-A, Stoodley P (2014) Bacterial biofilms on implanted suture material are a cause of surgical site infection. Surg Infect 15:592–600. https://doi.org/10.1089/sur.2013.016
Saeed K, McLaren AC, Schwarz EM, Antoci V, Arnold WV, Chen AF, Clauss M, Esteban J, Gant V, Hendershot E, Hickok N, Higuera CA, Coraça-Huber DC, Choe H, Jennings JA, Joshi M, Li WT, Noble PC, Phillips KS, Pottinger PS, Restrepo C, Rohde H, Schaer TP, Shen H, Smeltzer M, Stoodley P, Webb JCJ, Witsø E (2019) 2018 international consensus meeting on musculoskeletal infection: summary from the biofilm workgroup and consensus on biofilm related musculoskeletal infections. J Orthop Res 37:1007–1017. https://doi.org/10.1002/jor.24229
Sulamanidze M (2007) Evaluation of a novel technique for wound closure using a barbed suture. Plast Reconstr Surg 120:349–350. https://doi.org/10.1097/01.prs.0000264565.76712.dc
Wilson C, Lukowicz R, Merchant S, Valquier-Flynn H, Caballero J, Sandoval J, Okuom M, Huber C, Brooks TD, Wilson E, Clement B, Wentworth CD, Holmes AE (2017) Quantitative and Qualitative Assessment Methods for Biofilm Growth: A Mini-review. Res Rev J Eng Technol, 6:http://www.rroij.com/open-access/quantitative-and-qualitative-assessment-methods-for-biofilm-growth-a-minireview-.pdf
Leng JC, Mariano ER (2020) A little better is still better: using marginal gains to enhance “enhanced recovery” after surgery. Reg Anesth Pain Med 45:173–175. https://doi.org/10.1136/rapm-2019-101239
Hall D, James D, Marsden N (2012) Marginal gains: Olympic lessons in high performance for organisations. HR Bull Res Pract 7(2):9–13
Acknowledgements
The authors would like to thank Sister S.Boswell, Mr J. Joseph, and Mr M.Hannay for their expert help in this study.
Funding
The authors did not receive support from any organisation for the submitted work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
No identifiably patient data were used, and ethical approval was not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fawi, H.M.T., Papastergiou, P., Khan, F. et al. Use of monofilament sutures and triclosan coating to protect against surgical site infections in spinal surgery: a laboratory-based study. Eur J Orthop Surg Traumatol 33, 3051–3058 (2023). https://doi.org/10.1007/s00590-023-03534-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-023-03534-w