Abstract
Purpose
The issue of optimal prophylactic antibiotic administration for closed and open fracture surgeries remains controversial. The purpose of this study was to assess the role of type and duration longer than 48 h of antibiotic prophylaxis on the rates of fracture-related infection (FRI).
Methods
This is a single-center, prospective observational cohort study carried out with patients undergoing surgery for implants insertion to fracture stability. Risk estimates were calculated on the variables associated with factors for FRI and reported as a prevalence ratio (PR) with respect to the 95% confidence interval (CI).
Results
Overall, 132 patients were analyzed. The global rate of FRI was 15.9% (21/132), with open and closed fractures accounting for 30.5% (11/36) and 10.4% (10/96), respectively. The FRI rates in patients undergoing orthopedic surgery for fracture stabilization who received prophylactic antibiotic for up to and longer than 48 h were 8.9% and 26.4%, respectively. This difference did not reach statistical significance (prevalence ratio [PR] = 2.6, 95% confidence interval [95% CI]: 0.9–7.3. p = 0.063).
Conclusions
Duration of antibiotic prophylaxis for surgical orthopedic fractures was not correlated with rates of FRI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Infectious complications after orthopedic surgeries for fracture stabilization are feared for their impact on patient’s morbidity and mortality and increased treatment costs [1]. The systematic preventive measures adopted during surgeries for fractures corrections is heterogeneous, especially regarding antibiotic prophylaxis, such as the choice of antibiotics (monotherapy or association of different drug classes) and duration of therapy [2]. Even with improvements of surgical techniques and promptness in the care of patients with closed or open fractures, the rates of fracture-related infections (FRI) remain high in specific population [3].
High severity trauma with open fractures classified as Gustilo–Anderson (GA) III, affecting lower extremity and smoking are known risk factors for FRI, which can reach infection rates up to 30% [2, 4]. Thus, in addition to irrigation, through debridement and cleaning the lesion during fracture stabilization with modern orthopedic implants, the early use of systemic and broad-spectrum prophylactic antibiotics is a decisive factor for the prevention of FRI [5]. The antimicrobial spectrum remains based upon classic studies of Gustilo et al. [6] It consists of targeting activity against gram-positive bacteria in GA grade I and II open and closed fractures and additional activity against gram-negative bacteria in GA grade III open fractures, despite limited evidence confirming the benefit of this recommendation [7]. Recently, Chen et al. and Saveli et al. [8, 9] showed high rates of community-associated methicillin-resistant Staphylococcus aureus (CA-MRSA) infections after open fractures, which is not usually eliminated by currently proposed antimicrobial regimens [10, 11].
The duration of antibiotic prophylaxis over three days in order to prevent FRI in the presence of osteosynthesis is another controversial topic [5, 12]. There is a lack of high-quality studies on the subject and the most recent articles did not show any benefit in terms of extended prophylaxis duration [2, 12]. The Eastern Association for Surgery of Trauma (EAST) [11], for example, pinpoints that antibiotics be discontinued 24 h after wound closure for the correction of GA type I and type II open fractures, while for GA type III open fractures it suggests that antibiotics either should be discontinued in 72 h or no more than 24 h after wound coverage [6]. These advices have a low rate of adherence and compliance due to multiple factors, including disparities between orthopedic surgeons in the classification system for open fractures’ severity, different surgical techniques and local protocols without validation [12]. Lack of consensus and low adherence to proposed recommendations [1, 2, 12], may have affected the microbiological profile of FRI due to over-prescription of antibiotics [8, 9] and the increasing global problem of bacterial resistance alerts to the need for further studies on antibiotic prophylaxis in the management of orthopedic fractures [13, 14].
Therefore, the purpose of this study was to investigate the compliance to standard administration of prophylactic antibiotics in patients undergoing surgical management of open and closed fractures and to assess the role of type and duration longer than 48 h of antibiotic prophylaxis on FRI rates.
Material and methods
Population studied
This is a single-center, prospective observational cohort study with the purpose of assessing the adherence to standard proposed recommendations of prophylactic antibiotic administration in patients undergoing surgical treatment of open and closed fractures, and to analyze the impact of the type and longer duration of antibiotics in the rates of FRI. The study followed patients from December 2019 to February 2021, during the COVID-19 pandemic period, at an orthopedic reference tertiary hospital in São Paulo—Brazil. The study was carried out with all trauma patients with orthopedic fractures undergoing surgery for implants insertion to fracture stability (plates and screws, intramedullary nail, Kirschner wires), who received at least one dose of antibiotic prophylaxis and who were monitored by a minimum period of one year. The primary outcome was to investigate the impact of duration of antibiotic prophylaxis longer than 48 h in the FRI rates. The study was approved by the Institution’s Research Ethics Committee under the number CEP/UNIFESP n.0846P/2021.
Patients under 18 years old, with nonsurgical treatment for orthopedic fractures, external fixation as a definitive treatment for bone consolidation, patients who did not receive antibiotic prophylaxis, patients who did not attend follow-up outpatient appointments and with incomplete medical information were excluded.
Definitions
The diagnosis of fracture-related infection (FRI) was based on criteria published by Metsemakers et al., 2018 [15]. Preoperative antimicrobial prophylaxis (PAP) is defined as the systemic administration of antibiotics started in the perioperative period. The type of medication, dose and frequency followed current institutional protocols, and could be adapted according to medical assessment.
Variables analyzed
The variables analyzed in the study were obtained through prospective clinical follow-up, electronic medical records, and laboratory results. The variable of greatest interest analyzed was the duration of antibiotic prophylaxis greater than or less than 48 h used in fracture correction surgeries. Other variables related to the patient (1), to the fracture (2) and the surgical procedure (3). The patient-related variables are (1): demographics, comorbidities, alcoholism, smoking, ASA score, Charlson comorbidity score, and previous antimicrobial use in the last three months. The fracture-related variables (2) are: type of fracture, location, mechanism of trauma; to the surgical procedure are (3): time between fracture and surgical treatment, use of external fixer, prophylactic antimicrobial regimen used.
Statistical analysis
The association between the qualitative variables was performed using the chi-square test and Fisher’s exact test, and between the quantitative variables, bivariate logistic regression was used. Risk estimates were calculated on the variables associated with risk factors for FRI and reported as a prevalence ratio (PR) with respect to the 95% confidence interval (CI). The difference was considered statistically significant if the p value was lower than 0.05. All data were analyzed using the IBM SPSS Statistics 20 software.
Results
Population studied
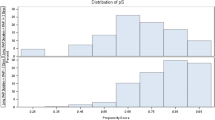
Overall, 132 patients with bone fractures undergoing surgical stabilization with osteosynthesis were included, 75% were male. The mean age was 50.4 years old (SD ± 22.9 years old). In the sample, 34.9% of the patients were older than 60 years old, but 64.9% had a Charlson morbidity score up to 2. Open fractures occurred in 27.3% (36/132) and among them, 69.4% were classified as GA type III. Most patients (66.7%) underwent definitive surgical correction of the fracture within 72 h after the trauma. The study period was almost fully carried out during the COVID-19 pandemic period. The overall rate of FRI was 15.9% (21/132), with open and closed fractures accounting for 30.5% (11/36) and 10.4% (10/96), respectively. Further demographic, clinical, and surgical information are described in Table 1.
Antibiotic prophylaxis
Antibiotic prophylaxis was universally applied to the sample population in the study. Prophylaxis with a single drug and combination therapy were performed in 78.8% (104/132) and 21.2% (28/132) of patients, respectively. The association of cephalosporin and aminoglycoside was prescribed in 71.4% of the cases of combination therapy. First-generation cephalosporin (cefazolin) was prescribed in 94.7% of the cases (Table 2).
All patients (25) with open fractures classified as G-A III received antibiotic therapy longer than 48 h and up to five days, while 17.7% (17/96) of closed fractures cases also received antibiotics longer than 48 h. The reasons for extending the duration of therapy for closed fractures were not described in the medical records. As expected, the duration of antibiotic prophylaxis was longer in the group of patients who received combination of antibiotics, due to the use of broader and more prolonged antibiotic therapy in the most severe open fractures.
Type and duration of antibiotic prophylaxis and fracture-related infection
Table 3 summarizes information of 21 patients with FRI. Prophylaxis with two or more antibiotics had a statistically significant correlation with higher rates of fracture-related infection (FRI) (non-infected 13.5% vs infected 57.1%, p < 0.001). This association is obviously expected, as all patients with open fractures received combined antibiotic prophylaxis.
On the other hand, among the 21 cases of FRI diagnosed, the analysis of duration of antibiotic prophylaxis revealed that only 12 (57.1%) received more than 48 h of antibiotic therapy, for open (7) and closed (5) fractures. The remaining nine FRI cases were open (4) and closed (5) fracture cases that took up to 48 h of therapy. It is worth mentioning that 17 of 96 closed fractures cases received antibiotic longer than 48 h with 5 of them evolving to FRI. The FRI rates among those who took up to and longer than 48 h of prophylactic antibiotic were 8.9% and 26.4%, respectively. Regardless of the considerable difference in FRI percentage found between these two groups, it did not reach statistical significance (prevalence ratio [PR] = 2.6, 95% confidence interval [95% CI]: 0.9–7.3. p = 0.063) as an independent risk factor for FRI. According to our results, the duration of antibiotic prophylaxis did not correlate with FRI rates.
Discussion
Our study demonstrated that antibiotic prophylaxis prescribed longer than 48 h for open and closed fractures stabilization did not correlate with FRI rates. Indeed, five of 17 patients (29.4%) with closed fractures who received prophylaxis for more than 48 h, evolved to FRI.
Protocols and guidelines [14, 16, 17] on the management of orthopedic fractures adopt antibiotic prophylaxis as a basic approach to reduce infections after fracture surgical stabilization with osteosynthesis. The purpose of antibiotic prophylaxis preoperatively is to obtain the maximum concentration above the drug minimum inhibitory concentration (MIC) in the skin and soft tissues during the period between the incision and the wound closure [13]. In open fractures, it has been shown that the early administration of antimicrobials is essential to reduce FRI even before performing the definitive synthesis, however, extending the duration of therapy does not guarantee greater success in preventing FRI [12, 18].
The duration of antibiotic prophylaxis after surgical management of orthopedic fractures remains debatable, especially for open fractures classified as GA III due to the lack of randomized controlled clinical trials [5, 18]. Gillespie et al. in a systematic review demonstrated that the antibiotic prophylaxis in closed fractures is cost-effective for preventing infections; however, the impact on bacterial resistance could not be estimated [13]. Dellinger et al. demonstrated that prophylaxis for one day versus five days in patients with open fractures had no statistically significant difference in relation to the FRI outcome [18]. Carsenti-Etesse et al. in a double-blind randomized study, demonstrated the equivalence of FRI rates in open fractures with a single dose of prophylactic antibiotic versus prolonged therapy [14]. Ondari et al. found no difference in FRI rates among patients with Gustilo II open tibial fractures that underwent antibiotic prophylaxis for 24 h or five days [19]. Dunkel et al. concluded, in a retrospective study that infection following open fractures is related to the extent of tissue damage, but not to the duration of antibiotic prophylaxis and that even for GA grade III fractures, one day of antibiotic administration may be as effective as prolonged prophylaxis [20]. Declerquet et al. in a retrospective study, did not find evidence for the prophylactic administration of antimicrobials for more than 72 h in open fractures of long bones [5]. Nevertheless, such studies have limitations and there is a lack of higher quality studies assessing the role of lower duration of prophylactic antibiotics on FRI rates.
Our study found an overall rate of 15.9% of FRI, 30.5% in open fractures. These results are consistent with rates found in other studies [6, 21,22,23]. Despite all the advances in the management of fractures, FRI rates remain stable, allowing questions about the protective effect of extended antibiotic prophylaxis. We argue that the use of antibiotics is one of the perioperative strategies that should be applied and taken in association with other measures already standardized, such as the adequate lavage, through debridement and coverage of soft tissues in the site of fracture.
Regarding the antibiotics used, cefazolin (1st generation cephalosporin) remains the leading drug, either as monotherapy or combined with aminoglycosides. In the present study, most antibiotics prescribed were in accordance with the guidelines of the EAST [22] and the Surgical Infections Society [23]. Johnson et al. in a retrospective study, demonstrated that 91.1% of cases had cefazolin as one of the agents used in prophylaxis with gentamicin being the second most used antibiotic in combination in dual therapy [24]. However, they also demonstrated a low rate of compliance with current recommendations for surgical fractures–only 33.2% of compliance [25]. In the present study, non-compliance was observed in 12.9% of closed fractures cases that received antibiotic prophylaxis longer than 48 h due to unexplained reasons. We hypothesized that the reason is likely due to concomitance between the COVID-19 pandemic period with which the study was carried out. Interestingly, an increased rate of hospitalization due to hip and femoral fractures in the elderly (probably related to the lockdown period) and a decrease in road traffic accidents were observed. Moreover, elderly people usually have more comorbidities, worse immune responses, and greater use of antibiotics for conditions other than orthopedic.
Our study has several limitations. It was conducted during the COVID-19 pandemic and lockdown period in a large tertiary teaching hospital offering special orthopedic care to a regional population located in a major city in a developing country, which limits the global comparison of the data. However, patients were prospectively followed for a period of at least 12 months, and importantly we applied the modern and standardized definition of FRI [15], decreasing the chance of bias. Despite the reasonable sample of patients undergoing surgical correction for fractures, the overall number of FRI was low which may have biased our results, although logistic regression analyses were performed to assess the role of type and duration of antibiotic administration on the rates of FRI.
We conclude that during the study period that was carried out concomitantly with the COVID-19 pandemic period, we observed an acceptable rate of non-compliance for antibiotic administration prophylaxis for closed and open fractures. Cefazolin and aminoglycosides in combination for open fractures correlates in higher rates of FRI, but the duration of antibiotic prophylaxis did not correlate with FRI.
References
Foster AL, Moriarty TF, Trampuz A, Jaiprakash A, Burch MA, Crawford R, Paterson DL, Metsemakers WJ, Schuetz M, Richards RG (2020) Fracture-related infection: current methods for prevention and treatment. Expert Rev Anti Infect Ther 18:307–321
Puetzler J, Zalavras C, Moriarty TF, Verhofstad MHJ, Kates SL, Raschke MJ, Rosslenbroich S, Metsemakers WJ (2019) Clinical practice in prevention of fracture-related infection: an international survey among 1197 orthopaedic trauma surgeons. Injury 50:1208–1215
Manuello R, Ruimy R, Boileau P, Trojani C, Courjon J (2020) Re: ‘Pathogenesis and management of fracture-related infection’ by Depypere et al. Clinical Microbiology and Infection 26:650–651
Saveli CC, Morgan SJ, Belknap RW, Ross E, Stahel PF, Chaus GW, Hak DJ, Biffl WL, Knepper B, Price CS (2013) Prophylactic antibiotics in open fractures: a pilot randomized clinical safety study.
Declercq P, Zalavras C, Nijssen A et al (2021) Impact of duration of perioperative antibiotic prophylaxis on development of fracture-related infection in open fractures. Arch Orthop Trauma Surg 141:235–243
Gustilo RB, Merkow RL, Templeman D (1990) The management of open fractures. J Bone Joint Surg Am 72(2):299–304 (PMID: 2406275)
Carver DC, Kuehn SB, Weinlein JC (2017) Role of systemic and local antibiotics in the treatment of open fractures. Orthop Clin North Am 48:137–153
Chen AF, Schreiber VM, Washington W, Rao N, Evans AR (2013) What is the rate of methicillin-resistant Staphylococcus aureus and gram-negative infections in open fractures? Clinical orthopaedics and related research. Springer, New York LLC, pp 3135–3140
Saveli CC, Belknap RW, Morgan SJ, Price CS. (2011) The role of prophylactic antibiotics in open fractures in an era of community-acquired methicillin-resistant Staphylococcus aureus. Orthopedics. 34(8):611–6; quiz 617. https://doi.org/10.3928/01477447-20110627-25. (PMID: 21800816).
Berriós-Torres SI, Umscheid CA, Bratzler DW et al (2017) Centers for disease control and prevention guideline for the prevention of surgical site infection, 2017. JAMA Surg 152:784–791
Hoff WS, Bonadies JA, Cachecho R, Dorlac WC (2011) East practice management guidelines work group: update to practice management guidelines for prophylactic antibiotic use in open fractures. J. Trauma–Injury, Infect Crit Care 70:751–754
Ryan SP, Kildow BJ, Tan TL, Parvizi J, Bolognesi MP, Seyler TM (2019) Is there a difference in infection risk between single and multiple doses of prophylactic antibiotics? A meta-analysis. Clin Orthop Relat Res 477:1577–1590
Wj G, Walenkamp G (2009) Antibiotic prophylaxis for surgery for proximal femoral and other closed long bone fractures (Review); Cochrane Database Syst Ver 17;2010(3):CD000244.
Carsenti-Etesse H, Doyon F, Desplaces N, Gagey O, Tancrède C, Pradier C, Dunais B, Dellamonica P (1999) Epidemiology of bacterial infection during management of open leg fractures. Springer-Verlag
Metsemakers WJ, Morgenstern M, McNally MA et al (2018) Fracture-related infection: a consensus on definition from an international expert group. Injury 49:505–510
Bratzler DW, Dellinger EP, Olsen KM et al (2013) Clinical practice guidelines for antimicrobial prophylaxis in surgery. Surg Infect 14:73–156
Chang Y, Bhandari M, Zhu KL et al (2019) Antibiotic Prophylaxis in the Management of Open Fractures. JBJS Reviews 7(2):e1
Patchen Dellinger E, Caplan ES, Weaver LD, et al (1987) Duration of preventive antibiotic administration for open extremity fractures from the departments of surgery ( PATIENTS AND METHODS Patients were enrolled at three centers (Harborview Medical).
Ondari JN, Masika MM, Ombachi RB, Ating’a JE (2016) Unblinded randomized control trial on prophylactic antibiotic use in gustilo II open tibia fractures at Kenyatta national hospital, Kenya. Injury 47:2288–2293
Dunkel N, Pittet D, Tovmirzaeva L, Suvà D, Bernard L, Lew D, Hoffmeyer P, Uçkay I, Bernard ν L, Lew ν D (2013) Short duration of antibiotic prophylaxis in open fractures does not enhance risk of subsequent infection; Bone Joint J. 95-B(6):831–7
Zimmerli W, Trampuz A, Ochsner PE (2004) Prosthetic-joint infections. N Engl J Med 351(16):1645–1654
Barton C, Bartlett C, McMillian W, Crookes B, Osler T (2012) Compliance with the eastern association for the surgery of trauma guidelines for prophylactic antibiotics after open extremity fracture. Int J Crit Illn Inj Sci 2:57
Hauser CJ, Adams CA, Eachempati SR (2006) Surgical infection society guideline prophylactic antibiotic use in open fractures: an evidence-based guideline*. Surg Infect (Larchmt) 7(4):379–405
Johnson EN, Burns TC, Hayda RA, Hospenthal DR, Murray CK (2007) Infectious complications of open type III tibial fractures among combat casualties. Clin Infect Dis 45:409–415
Johnson HC, Bailey AM, Baum RA, Justice SB, Weant KA (2020) Compliance and related outcomes of prophylactic antibiotics in traumatic open fractures. Hosp Pharm 55:193–198
Acknowledgements
We would like to thank the “Hospital São Paulo” for providing key support to conduct this study, and to Ana Claudia Couto de Abreu who contributed in the statistical analysis of our study.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
SBP, ECSdS, AMDA, MJCS, FBR and CAF were involved in substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work. SBP, ECSdS, AMDA and MJCS were involved in drafting the work or revising it critically for important be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. FBR and CAF were involved in drafting the work or revising it critically for important intellectual content and also involved in final approval of the version to be published.
Corresponding author
Ethics declarations
Conflict of interest
Each author certifies that neither he, nor any member of his immediate family, have funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Ethics approval
The study was approved by the Institution’s Research Ethics Committee under the number 50075321.30000.5505.
Informed consent
WAIVER OF CONSENT JUSTIFICATION: Patient consent was waived by the local IRB for this observational study because it involved minimal risk to the subject due to the anonymization of patients’ data and meets specific criteria during the COVID-19 pandemic period. The reasonable rationale for why the research would not be possible without the waiver is stated below: 1. The need to carry out only online consultation follow-up, made it difficult to obtain many patients’ consents, as social distance was mandatory during this period. 2. Fracture-related infection diagnosis is usually performed months after surgery, and many patients were contacted online or even by telephone, hindering the possibility to obtain a signed informed consent. 3. The research could not practically be carried out without waiver, as it involved more than 100 non-infected patients. 4. Part of this cohort study is retrospective because existing data, specimens and medical records were available and analyzed as of the date of IRB submission. 5. The research could not practicably be carried out without using identifiable private information and biospecimens in an identifiable format. 6. The waiver will not adversely affect the rights and welfare of the subjects. 7. Inability to identify subjects that are likely to evolve to fracture-related infection, which may occur from the emergency admission to months after the surgical procedure. Therefore, the study staff can't plan for coverage to obtain consent. 8. The study involved more than 100 patients undergoing any type of surgery for fracture stabilization, which has been physically impossible to obtain consent from them all. 9. The number of patients with FRI was small (21) and removing any subject due to the impossibility to obtain the consent or even those refusing to participate in the study would largely bias our results. 10. FRI is a relatively rare disease and loss of a few subjects would affect the power of the study. 11. During the COVID-19 pandemic period, there were subjects, especially older patients, with severe medical condition and co-infected with SARS-CoV2 virus infection, which was not appropriate to approach families during the course of hospitalization.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Prebianchi, S., Santos, E.C., Dell’Aquila, A. et al. Type of antibiotic but not the duration of prophylaxis correlates with rates of fracture-related infection. Eur J Orthop Surg Traumatol 33, 987–992 (2023). https://doi.org/10.1007/s00590-022-03246-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-022-03246-7