Abstract
Introduction
Improvement in reverse total shoulder arthroplasty (RTSA) prosthesis and technique has reduced the initially high complication and revision rates associated with this implant. However, instability continues to be a leading cause of reoperation after RTSA, being related in previous studies with medialized designs. The aim of this study was to determine the dislocation rate with the employment of two medialized modular systems of RTSA in our institution.
Materials and methods
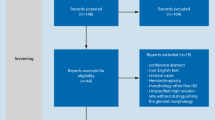
A retrospective review of two different modular systems of RTSA (SMR Modular Shoulder System and Delta XTEND Reverse Shoulder) was performed between 2009 and 2017 with a minimum 3-year follow-up. Baseline demographic, clinical (Constant, ASES and ROM), and radiographic data were collected. Characteristics of postoperative instability cases were also evaluated.
Results
237 primary RTSA (41% SMR/59% Delta) and 34 revision RTSA (44% SMR/56% Delta) with a mean follow-up of 75.6 ± 5.2 months (79.2 SMR/86.3 Delta, p = .586) were included in the present study. Indications for primary RTSA were osteoarthritis, rotator cuff tear arthropathy and massive irreparable rotator cuff tear (64%), acute fracture (32%), and fracture sequelae (4%). Subscapularis tendon was always repaired in degenerative pathology and tuberosities reattached in traumatic cases. The mean age of the global series was 76.5 ± 5.3 years (75.8 SMR/78.6 Delta, p = .104) with a mean Constant/ASES score at final follow-up of 68.5 ± 4.3/72.9 ± 20.3 (71/68 SMR and 69/74 Delta, p = .653 and .642). Only 2 patients (one acute fracture and one fracture sequelae) suffered an early postoperative anterior dislocation (before 3 months) which represents a rate of .84% in primary cases and .73% including revision surgery. Closed reduction manoeuvres were not successful, and both patients required revision surgery. At the end follow-up, both were stable and had no further dislocations.
Conclusion
The dislocation rate after RTSA with the employment of two contemporary modular systems with a medialized centre of rotation is extremely low, especially when compared with the previously published series with the original Grammont design. Acute fracture and fracture sequelae were the main diagnoses associated with this instability. The reasons for the low dislocation rate are multifactorial, but the improvement in the baseplate position according to the more recent standards of “ideal position” and technical aspects such as subscapularis repair or tuberosity reattachment in fractures probably play an important role in this aspect.


Similar content being viewed by others
References
Boileau P, Watkinson DJ, Hatzidakis AM, Balg F (2005) Grammont reverse prosthesis: design, rationales, and biomechanics. J Shoulder Elbow Surg 14:147S-S161. https://doi.org/10.1016/j.jse.2004.10.006
Lopiz Y, Garcia-Coiradas J, Serrano-Mateo L, García-Fernández C, Marco F (2016) Reverse shoulder arthroplasty for acute proximal humeral fractures in the geriatric patient: results, health-related quality of life and complication rates. Int Orthop 40:771–781. https://doi.org/10.1007/s00264-015-3085-z
García-Fernández C, Lopiz Y, Rizo B, Serrano-Mateos L, Alcobía-Díaz B et al (2018) Reverse total shoulder arthroplasty for the treatment of failed fixation in proximal humeral fractures. Injury 49S:S22–S26. https://doi.org/10.1016/j.injury.2018.06.042
Chalmers PN, Rahman Z, Romeo AA, Nicholson GP (2014) Early dislocation after reverse total shoulder arthroplasty. J Shoulder Elbow Surg 23(5):737–744. https://doi.org/10.1016/j.jse.2013.08.015
García-Fernández C, Lópiz-Morales Y, Rodríguez A, López-Durán L, Marco Martínez F (2015) Periprosthetic humeral fractures associated with reverse total shoulder arthroplasty: incidence and management. Int Orthop 39:1965–1969. https://doi.org/10.1007/s00264-015-2972-7
Cheung E, Willis M, Walker M, Clark R, Frankle M (2011) Complications in reverse total shoulder arthroplasty. J Am Acad Orthop Surg 19:439–449. https://doi.org/10.5435/00124635-201107000-00007
Scarlat MM (2013) Complications with reverse total shoulder arthroplasty and recent evolutions. Int Orthop 37:843–851. https://doi.org/10.1007/s00264-013-1832-6
Parada SA, Flurin PH, Wright TW, Zuckerman JD, Elwell JA et al (2021) Comparison of complication types and rates associated with anatomic and reverse total shoulder arthroplasty. J Shoulder Elbow Surg 30(4):811–818. https://doi.org/10.1016/j.jse.2020.07.028
Crum RJ, de Sa DL, Su FL, Lesniak BP, Lin A (2021) Decreased complication profile and improved clinical outcomes of primary reverse total shoulder arthroplasty after 2010: a systematic review. Shoulder Elbow 13(2):154–167. https://doi.org/10.1177/1758573219852977
Rauck RC, Eck EP, Chang B, Craig EV, Dines JS et al (2020) Survivorship of a medialized glenoid and lateralized onlay humerus reverse shoulder arthroplasty is high at midterm follow-up. HSS J 16(Suppl 2):293–299. https://doi.org/10.1007/s11420-019-09721-y
Cheung EV, Sarkissian EJ, Sox-Harris A, Comer GC, Saleh JR et al (2018) Instability after reverse total shoulder arthroplasty. J Shoulder Elbow Surg 27:1946–1952. https://doi.org/10.1016/j.jse.2018.04.015
Clark JC, Ritchie J, Song FS, Kissenberth MJ, Tolan SJ, Hart ND et al (2012) Complication rates, dislocation, pain, and postoperative range of motion after reverse shoulder arthroplasty in patients with and without repair of the subscapularis. J Shoulder Elbow Surg 21:36–41. https://doi.org/10.1016/j.jse.2011.04.009
Farshad M, Gerber C (2010) Reverse total shoulder arthroplasty-from the most to the least common complication. Int Orthop 34:1075–1082. https://doi.org/10.1007/s00264-010-1125-2
Zumstein MA, Pinedo M, Old J, Boileau P (2011) Problems, complications, reoperations and revision in reverse total shoulder arthroplasty: a systematic review. J Shoulder Elbow Surg 20:146–57. https://doi.org/10.1016/j.jse.2010.08.001
Boileau P (2016) Complications and revision of reverse total shoulder arthroplasty. Orthop Traumatol Surg Res 102(1 Suppl):S33-43. https://doi.org/10.1016/j.otsr.2015.06.031
Frankle M, Siegal S, Pupello D, Saleem A, Mighell M et al (2005) The reverse shoulder prosthesis for glenohumeral arthritis associated with severe rotator cuff deficiency. A minimum two-year follow-up study of sixty patients. J Bone Joint Surg Am 87:1697–1705. https://doi.org/10.2106/JBJS.D.02813
Werthel JD, Walch G, Vegehan P, Deransart P, Sánchez-Sotelo J et al (2019) Lateralization in reverse shoulder arthroplasty: a descritive analysis of different implants in current practice. Int Orthop 43:2349–2360. https://doi.org/10.1007/s00264-019-04365-3
Mattewson G, Kooner S, Kwapisz A, Leiter J, Old J et al (2019) The effect of subscapularis repair on dislocation rates in reverse shoulder arthroplasty: a meta-analysis and systematic review. J Shoulder Elbow Surg 28:989–997. https://doi.org/10.1016/j.jse.2018.11.069
Kang JR, Dubiel MJ, Cofield RH, Steinmann SP, Elhassan BT et al (2019) Primary reverse shoulder arthroplasty using contemporary implants is associated with very low reoperation rates. J Shoulder Elbow Surg 28:S175–S180. https://doi.org/10.1016/j.jse.2019.01.026
Constant CR, Murley AH (1987) A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 214:160–164
Constant CR, Gerber C, Emery RJ, Sojbjerg JO, Gohlke F et al (2008) A review of the Constant score: modifications and guidelines for its use. J Shoulder Elbow Surg 17:355–361. https://doi.org/10.1016/j.jse.2007.06.022
Cuff D, Pupello D, Virani N, Levy J, Frankle M (2008) Reverse shoulder arthroplasty for the treatment of rotator cuff deficiency. J Bone Joint Surg Am 90:1244–1251. https://doi.org/10.2106/JBJS.G.00775
Boileau P, Watkinson D, Hatzidakis AM, Hovorka I (2006) Neer Award 2005: the Grammont reverse shoulder prosthesis: results in cuff tear arthritis, fracture sequelae, and revision arthroplasty. J Shoulder Elbow Surg 15:527–540. https://doi.org/10.1016/j.jse.2006.01.003
Werner BS, Chaoui J, Walch G (2017) The influence of humeral neck shaft angle and glenoid lateralization on range of motion in reverse shoulder arthroplasty. J Shoulder Elbow Surg 26(10):1726–1731. https://doi.org/10.1016/j.jse.2017.03.032
Cuff DJ, Pupello DR, Santoni BG, Clark RE, Frankle MA (2017) Reverse shoulder arthroplasty for the treatment of rotator cuff deficiency: a concise follow-up, at a minimum of 10 years, of previous reports. J Bone Joint Surg Am 99(22):1895–1899. https://doi.org/10.2106/JBJS.17.00175
Edwards TB, Williams MD, Labriola JE, Elkousy HA, Garstman GM et al (2009) Subscapularis insufficiency and the risk of shoulder dislocation after reverse shoulder arthroplasty. J Shoulder Elbow Surg 18:892–896. https://doi.org/10.1016/j.jse.2008.12.013
Teusink MJ, Pappou IP, Schwartz CBJ, Frankle MA (2015) Results of closed management of acute dislocation after reverse shoulder arthroplasty. J Shoulder Elbow Surg 24:621–627. https://doi.org/10.1016/j.jse.2014.07.015
Gallo RA, Gamradt SC, Mattern CJ, Cordasco FA, Craig EV et al (2011) Instability after reverse total shoulder replacement. J Shoulder Elbow Surg 20:584–590. https://doi.org/10.1016/j.jse.2010.08.028
Abdelfattah A, Otto RJ, Simon P, Christmas KN, Tanner G et al (2018) Classification of instability after reverse shoulder arthroplasty guides surgical management and outcomes. J Shoulder Elbow Surg 27(4):e107–e118. https://doi.org/10.1016/j.jse.2017.09.031
Kohan EM, Chalmers PN, Salazar D, Keener JD, Yamaguchi K et al (2017) Dislocation following reverse total shoulder arthroplasty. J Shoulder Elbow Surg 26:1238–1245. https://doi.org/10.1016/j.jse.2016.12.073
Izquierdo-Fernández A, Minarrro JC, Carpintero-Lluch R, Estévez-Torres EM, Carpintero-Benítez P (2018) Reverse shoulder arthroplasty in obese patients: analysis of functionality in the medium term. Arch Orthop Trauma Surg 138:1–5. https://doi.org/10.1007/s00402-017-2816-6
Pastor MF, Kraemer M, Wellmann M, Hurschler C, Smith T (2016) Anterior stability of the reverse shoulder arthroplasty depending on implant configuration and rotator cuff condition. Arch Orthop Trauma Surg 136:1513–1519. https://doi.org/10.1007/s00402-016-2560-3
Raiss P, Edwards TB, Da Silva MR, Bruckner T et al (2014) Reverse shoulder arthroplasty for the treatment of nonunions of the surgical neck of the proximal part of the humerus (type-3 fracture sequelae). J Bone Joint Surg Am 96:2070–2076. https://doi.org/10.2106/JBJS.N.00405
Randelli P, Randelli F, Arrigoni P, Ragone V, D’Ambrosi R et al (2014) Optimal glenoid component inclination in reverse shoulder arthroplasty How to improve implant stability. Musculoskelet Surg 98(Suppl 1):S15–S18. https://doi.org/10.1007/s12306-014-0324-1
Martinez AA, Bejarano C, Carbonel I, Iglesias D, Gil-Albarova J et al (2012) The treatment of proximal humerus nonunions in older patients with reverse shoulder arthroplasty. Injury 43(Suppl 2):S3-6. https://doi.org/10.1016/S0020-1383(13)70172-4
Tashjian RZ, Martin BI, Ricketts CA, Henninger HB, Granger EK et al (2018) Superior baseplate inclination is associated with instability after reversing total shoulder arthroplasty. Clin Orthop Relat Res 476(8):1622–1629. https://doi.org/10.1097/CORR.0000000000000340
Kemp AL, King JJ, Farmer KW, Wright TW (2016) Reverse total shoulder arthroplasty in wheelchair-dependent patients. J Shoulder Elbow Surg 25(7):1138–1145. https://doi.org/10.1016/j.jse.2015.11.006
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
This manuscript has been read and approved by all authors, and we ensure that the manuscript represents an honest work. CG-F: Author responsible, YL: Writing—Review and Editing, CA: Investigation, VP: Writing—Original Draft, BA-D: Resources, Formal Analysis, MG-O: Writing—Original Draft, FM: Supervision.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare they have no financial interests.
Ethical approval
Institutional review board approval for this study was received from the Ethics Committee for Clinical Research (CEIC) from Hospital Clínico San Carlos (Madrid, Spain) (C.I. 20/779-E).
Consent of participate
Informed consent was obtained from all individual participants included in the study.
Consent of publication
All authors read and approved the final manuscript and give their consent for the publication of the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Garcia-Fernandez, C., Lopiz, Y., Arvinius, C. et al. Dislocation after reverse total shoulder arthroplasty using contemporary medialized modular systems. Can we still consider it such a frequent complication?. Eur J Orthop Surg Traumatol 32, 1525–1534 (2022). https://doi.org/10.1007/s00590-021-03131-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-021-03131-9