Abstract
Purpose
Gastrocnemius flaps provide reliable reconstructive solutions to soft-tissue loss of the knee and proximal tibia following orthopedic procedures. While this technique has been used and studied, little is known about its prophylactic application. Single-stage and delayed approaches were compared with respect to the timing of débridement, complications, and relationship between microorganisms and complications.
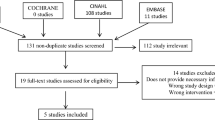
Methods
Gastrocnemius flaps for soft-tissue defects of the knee joint were retrospectively reviewed. Success of the flap procedure was defined as a healed soft-tissue envelope, no evidence of infection, a good blood supply to the flap, and adherence of the flap to its bed. Independent sample t test was used to compare the corresponding parameters (level of statistical significance was 0.05).
Results
Of 43 flaps (43 patients), 18 were performed during a single-stage procedure along with the orthopedic procedure and 25 were delayed. Success of the single-stage (100%) and delayed flaps (88%) was not significantly different (p = 0.083). Complication rate did not differ significantly for single-stage (11%) and delayed flaps (24%) (p = 0.272). We were unable to establish a relationship between complications and microorganisms.
Conclusion
Results indicate both approaches are reliable. Single-stage gastrocnemius flaps may eliminate the need for a second surgery.
Level of Evidence
Level III (Therapeutic, Retrospective cohort)





Similar content being viewed by others
Availability of data and material
Data available upon request.
Code availability
Not applicable.
References
Hallock GG (2000) Utility of both muscle and fascia flaps in severe lower extremity trauma. J Trauma 48(5):913–917
Phisitkul P, McKinley TO, Nepola JV, Marsh JL (2007) Complications of locking plate fixation in complex proximal tibia injuries. J Orthop Trauma 21(2):83–91
Pu LL (2010) Soft-tissue coverage of an extensive mid-tibial wound with the combined medial gastrocnemius and medial hemisoleus muscle flaps: the role of local muscle flaps revisited. J Plast Reconstr Aesthet Surg 63(8):e605–e610
Conway JD, Mont MA, Bezwada HP (2004) Arthrodesis of the knee. J Bone Joint Surg Am 86:835–848
Gerwin M, Rothaus KO, Windsor RE, Brause BD, Insall JN (1993) Gastrocnemius muscle flap coverage of exposed or infected knee prosthesis. Clin Orthop Relat Res 286:64–70
Nahabedian MY, Mont MA, Orlando JC, Delanois RE, Hungerford DS (1999) Operative management and outcome of complex wounds following total knee arthroplasty. Plast Reconstr Surg 104:1688–1697
Sanders R, O’Neill T (1981) The gastrocnemius myocutaneous flap used as a cover for the exposed knee prosthesis. J Bone Joint Surg Br 63:383–386
Innocenti M, Cardin-Langlois E, Menichini G, Baldrighi C (2014) Gastrocnaemius-propeller extended miocutanous flap: a new chimaeric flap for soft tissue reconstruction of the knee. J Plast Reconstr Aesthet Surg 67(2):244–251
McPherson EJ, Patzakis MJ, Gross JE, Holtom PD, Song M, Dorr LD (1997) Infected total knee arthroplasty. Two-stage reimplantation with a gastrocnemius rotational flap. Clin Orthop Relat Res 341:73–81
Panni AS, Vasso M, Cerciello S, Salgarello M (2011) Wound complications in total knee arthroplasty. Which flap is to be used? With or without retention of prosthesis? Knee Surg Sports Traumatol Arthrosc 19(7):1060–1068
Ries MD, Bozic KJ (2006) Medial gastrocnemius flap coverage for treatment of skin necrosis after total knee arthroplasty. Clin Orthop Relat Res 446:186–192
Corten K, Struelens B, Evans B, Graham E, Bourne RB, MacDonald SJ (2013) Gastrocnemius flap reconstruction of soft-tissue defects following infected total knee replacement. Bone Joint J 95-B(9):1217–1221
Tetreault MW, Della Valle CJ, Bohl DD, Lodha SJ, Biswas D, Wysocki RW (2016) What factors influence the success of medial gastrocnemius flaps in the treatment of infected TKAs? Clin Orthop Relat Res 474(3):752–763
Macedo JLS, Rosa SC, Silva AA, Filho Neto AVR, Rugé PHS, Scartazzini C (2016) Versatility of the medial gastrocnemius muscle flap in reconstructing lower limb soft tissue lesions. Rev Bras Cir Plást 31(4):527–533
Houdek MT, Wagner ER, Wyles CC, Harmsen WS, Hanssen AD, Taunton MJ, Moran SL (2018) Long-term outcomes of pedicled gastrocnemius flaps in total knee arthroplasty. J Bone J Surg Am 100(10):850–856
Warren SI, Murtaugh TS, Lakra A, Reda LA, Shah RP, Geller JA, Cooper HJ (2018) Treatment of periprosthetic knee infection with concurrent rotational muscle flap coverage is associated with high failure rates. J Arthroplasty 33(10):3263–3267
Acknowledgements
The authors thank Alvien Lee and Amanda E. Chase, MA, for their invaluable assistance with the manuscript.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and/or design. Data collection and analysis were performed by VH. The first draft of the manuscript was written by VH, and critical revisions were made to improve intellectual content by the other three authors. All authors commented on previous versions of the manuscript as well as read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
JDC is a consultant for Bonesupport, Smith + Nephew, and Zimmer Biomet; receives fellowship support from Biocomposites; and her spouse receives royalties from University of Florida. The following organizations supported the institution of JDC and CJD: Biocomposites, DePuy Synthes Companies, MHE Coalition, Orthofix, OrthoPediatrics, Pega Medical, Smith + Nephew, Stryker, and Zimmer Biomet. VH and HMA have nothing to disclose. CJD has nothing additional to disclose.
Ethics approval
An official exemption letter was obtained from our organization’s institutional review board.
Ethical standards
The study was conducted in accordance with the ethical standards of the institutional review board, with the 1964 Helsinki Declaration and its later amendments, and with current national laws. An official exemption letter was obtained from our organization’s institutional review board. For this retrospective study, formal consent was not required.
Consent to participate
For this retrospective study, formal consent was not required.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hambardzumyan, V., Deter, C.J., Alrabai, H.M. et al. Comparison of single-stage and delayed gastrocnemius flap procedures for soft-tissue defects of the knee and proximal tibia. Eur J Orthop Surg Traumatol 32, 1081–1087 (2022). https://doi.org/10.1007/s00590-021-03058-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-021-03058-1