Abstract
Purpose
The cemented Exeter V40 stem is known to migrate distally. Several previous studies have reported on the extent of stem migration and its influence on clinical outcome. However, no studies have investigated the influence of stem migration on Patient Reported Outcome Measures (PROM).
Methods
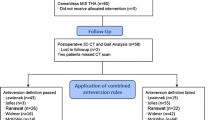
One hundred and twelve total hip arthroplasties (THA) were included in a 2-year follow-up using Radiostereometric Analysis (RSA). Patients were evaluated using the Oxford Hip Score (OHS) and EQ-5D-3L PROMs. The purpose of this study was to assess the influence of stem migration, measured by Maximum Total Point Motion (MTPM), on the 2-year postoperative score (OHS and EQ-5D). Furthermore, the influence of pre-operative PROM, age, gender, acetabular component and BMI was associated with the 2-year postoperative OHS and EQ-5D scores.
Results
MTPM was a non-significant predictor of the 2-year postoperative OHS (regression coefficient (B) = − 2.38 (CI − 5.44; .69)) and of the 2-year postoperative EQ-5D (B = − .01 (CI − .04; .02)). The only significant predictor of the 2-year postoperative OHS and 2-year postoperative EQ-5D was gender (B = 8.71 (CI 3.52; 13.90)) and (B = .13 (CI .07; .18)), respectively.
Conclusion
Stem migration did not significantly influence PROMs at 2 years post-operatively. Using a patient-focused approach, our results seem to corroborate results reported by previous studies, showing that slow migration of the Exeter V40 stem does not seem to influence the clinical outcome.





Similar content being viewed by others
Availability of data and materials
Data are available from corresponding author on request.
References
Overgaard (ed.) S. Danish Hip Arthroplasty Register. 2018.
Stryker. Stryker’s Exeter hip stem turns 50|Stryker 2020. https://www.stryker.com/us/en/about/news/2020/stryker-s-exeter-hip-stem-turns-50.html. Accessed February 21, 2021.
Shen G (1998) Femoral stem fixation. Aan engineering interpretation of the long-term outcome of Charnley and Exeter stems. J Bone Joint Surg Br 80:754–756. https://doi.org/10.1302/0301-620X.79B5.7177
Alfaro-Adrian J, Gill HS, Murray DW (1999) Cement migration after THR A comparison of charnley elite and exeter femoral stems using RSA. J Bone Joint Surg Br 81:130–134
Stefansdottir A, Franzén H, Johnsson R, Ornstein E, Sundberg M (2004) Movement pattern of the Exeter femoral stem: a radiostereometric analysis of 22 primary hip arthroplasties followed for 5 years. Acta Orthop Scand 75:408–414. https://doi.org/10.1080/00016470410001169
Alfaro-Adrián J, Gill HS, Murray DW (2001) Should total hip arthroplasty femoral components be designed to subside? A radiostereometric analysis study of the Charnley Elite and Exeter stems. J Arthroplasty 16:598–606. https://doi.org/10.1054/arth.2001.23576
Nieuwenhuijse MJ, Valstar ER, Kaptein BL, Nelissen RG (2012) The Exeter femoral stem continues to migrate during its first decade after implantation: 10–12 years of follow-up with radiostereometric analysis (RSA). Acta Orthop 83:129–134. https://doi.org/10.3109/17453674.2012.672093
Carrington NC, Sierra RJ, Gie GA, Hubble MJW, Timperley AJ, Howell JR (2009) The Exeter Universal cemented femoral component at 15–17 years. J Bone Joint Surg Br 84:324–334
Rolfson O, Bohm E, Franklin P, Lyman S, Denissen G, Dawson J et al (2016) (2016) Patient-reported outcome measures in arthroplasty registries Report of the Patient-Reported Outcome Measures Working Group of the International Society of Arthroplasty Registries Part II. Recommendations for selection, administration, and analysis. Acta Orthop. https://doi.org/10.1080/17453674.2016.1181816
Kingsley C, Patel S (2017) Patient-reported outcome measures and patient-reported experience measures. BJA Educ 17:137–144. https://doi.org/10.1093/bjaed/mkw060
Paulsen A, Odgaard A, Overgaard S (2012) Translation, cross-cultural adaptation and validation of the Danish version of the Oxford hip score: assessed against generic and disease-specific questionnaires. Bone Joint Res 1:225–233. https://doi.org/10.1302/2046-3758.19.2000076
Aalund P, Glassou E, Hansen T (2017) The impact of age and preoperative health-related quality of life on patient-reported improvements after total hip arthroplasty. Clin Interv Aging 12:1951–1956. https://doi.org/10.2147/CIA.S149493
Singh JA (2009) Age, gender, obesity, and depression are associated with patient- related pain and function outcome after revision total hip arthroplasty. Clin Rheumatol 28:1419–1430. https://doi.org/10.1007/s10067-009-1267-z.Age
Biring GS, Masri BA, Greidanus NV, Duncan CP, Garbuz DS (2007) Predictors of quality of life outcomes after revision total hip replacement. J Bone Joint Surg Br 89:1446–1451. https://doi.org/10.1302/0301-620x.89b11.19617
Jameson SS, Mason JM, Baker PN, Elson DW, Deehan DJ, Reed MR (2014) The impact of body mass index on patient reported outcome measures (proms) and complications following primary hip arthroplasty. J Arthroplasty 29:1889–1898. https://doi.org/10.1016/j.arth.2014.05.019
Kärrholm J (1989) Roentgen stereophotogrammetry. Review of orthopedic applications. Acta Orthop Scand 60:491–503. https://doi.org/10.3109/17453678909149328
Valstar ER, Gill R, Ryd L, Flivik G, Börlin N, Kärrholm J (2005) Guidelines for standardization of radiostereometry (RSA) of implants. Acta Orthop 76:563–572. https://doi.org/10.1080/17453670510041574
Ejaz A, Laursen AC, Jakobsen T, Rasmussen S, Nielsen PT, Laursen MB (2015) Absence of a tourniquet does not affect fixation of cemented TKA: a randomized RSA study of 70 patients. J Arthroplasty 30:2128–2132. https://doi.org/10.1016/j.arth.2015.05.058
Ryd L, Albrektsson BEJ, Carlson L, Dansgård F, Herberts P, Lindstrand A et al (1995) Roentgen Stereophotogrammetric Analysis as a Predictor of Mechanical Loosening of Knee Prosthesis. Surgery 77:377–383
McCalden RW, Charron KD, Yuan X, Bourne RB, Naudie DD, MacDonald SJ (2010) Randomised controlled trial comparing early migration of two collarless polished cemented stems using radiostereometric analysis. J Bone Jt Surg 92:935–940. https://doi.org/10.1302/0301-620X.92B7.24462
Paulsen A, Roos EM, Pedersen AB, Overgaard S (2014) Minimal clinically important improvement (MCII) and patient-acceptable symptom state (PASS) in total hip arthroplasty (THA) patients 1 year postoperatively. Acta Orthop 85:39–48. https://doi.org/10.3109/17453674.2013.867782
Beard DJ, Harris K, Dawson J, Doll H, Murray DW, Carr AJ et al (2015) Meaningful changes for the Oxford hip and knee scores after joint replacement surgery. J Clin Epidemiol 68:73–79. https://doi.org/10.1016/j.jclinepi.2014.08.009
Acknowledgements
The authors thank Eric Garling for providing the RSA models, Kirsten Duch for vetting the statistical analysis, Heidi Ladefoged Poulsen for performing the RSA analyses and Merete Hessellund for technical support.
Funding
This study was supported by Innovation Fund Denmark. Grant No: 69-2013-1.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
This study was approved by the Ethics Committee of the North Jutland Region, and the National Data Protection Agency RN2015-141.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Steiner, D.K., Drivsholm, N.S., Buchardt, S.T.E. et al. The influence of migration of the exeter V40 stem on patient reported outcome measures: a 2-year follow-up of 112 total hip arthroplasties using radiostereometric analysis. Eur J Orthop Surg Traumatol 32, 167–174 (2022). https://doi.org/10.1007/s00590-021-02937-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-021-02937-x