Abstract
Background
We established a method in which patients are instructed before total knee arthroplasty (TKA) in a differentiated way without the necessity of reading any self-orientation, which can be applied even for illiterate patients
Methods
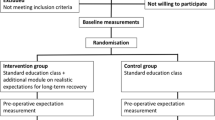
We developed a multidisciplinary approach to improve patient education in TKA comprising of a differentiated orientation conducted by an orthopedic surgeon, a nurse and a physiotherapist. It consists of standardized lectures regarding on pre-, intra- and postoperative issues in a randomized controlled trial of 79 consecutive patients undergoing primary TKA. Thirty-four patients received the standard education (control group), and 45 patients received the differentiated education (intervention group). The patients were evaluated during at least 6 months.
Results
After a 6-month follow-up period, the Short Form Health Survey (SF-36), the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), the visual analogue pain scale (VAS) and knee range of motion (ROM) improved significantly in both groups. Range of motion was better in the intervention group (mean and SD—106.9 ± 5.7 versus 92.5 ± 12.1 degrees, p = 0.02). Moreover, walk ability (more than 400 m) was better in the intervention group compared with the control group (97.4% versus 72.4%, p = 0.003). In the intervention and control groups, respectively, 10.5% and 31% of patients reported the need for some walking devices (p = 0.03).
Conclusions
A differentiated educational program with a multidisciplinary team had a positive impact on functional outcomes, improving ROM and walk ability of patients undergoing TKA in a short-term evaluation.


Similar content being viewed by others
Availability of data and materials
Abbreviations
- TKA:
-
Total knee arthroplasty
- SF-36:
-
Medical Study 36-item Short-Form Health Survey
- WOMAC:
-
Western Ontario and McMaster Universities Osteoarthritis Index
- ROM:
-
Range of motion
- OA:
-
Osteoarthritis
- VAS:
-
Visual analog scale
References
Buckwalter JA (1995) Osteoarthritis and articular cartilage use, disuse, and abuse: experimental studies. J Rheumatol Suppl 43:13–15
Neogi T, Zhang Y (2013) Epidemiology of osteoarthritis. Rheum Dis Clin North Am 39(1):1–19
Murphy L, Schwartz TA, Helmick CG, Renner JB, Tudor G, Koch G et al (2008) Lifetime risk of symptomatic knee osteoarthritis. Arthritis Rheum 59(9):1207–1213
Arden N, Nevitt MC (2006) Osteoarthritis: epidemiology. Best Pract Res Clin Rheumatol 20(1):3–25
Senna ER, De Barros AL, Silva EO, Costa IF, Pereira LV, Ciconelli RM et al (2004) Prevalence of rheumatic diseases in Brazil: a study using the COPCORD approach. J Rheumatol 31(3):594–597
Utrillas-Compaired A, De la Torre-Escuredo BJ, Tebar-Martínez AJ, Asúnsolo-Del BÁ (2014) Does preoperative psychologic distress influence pain, function, and quality of life after TKA? Clin Orthop Relat Res 472(8):2457–2465
Pagnano MW, McLamb LA, Trousdale RT (2004) Total knee arthroplasty for patients 90 years of age and older. Clin Orthop Relat Res 418:179–183
Ethgen O, Bruyère O, Richy F, Dardennes C, Reginster JY (2004) Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg Am. 86(A5):963–974
Shan L, Shan B, Suzuki A, Nouh F, Saxena A (2015) Intermediate and long-term quality of life after total knee replacement: a systematic review and meta-analysis. J Bone Joint Surg Am 97(2):156–168
Louw A, Diener I, Butler DS, Puentedura EJ (2013) Preoperative education addressing postoperative pain in total joint arthroplasty: review of content and educational delivery methods. Physiother Theory Pract 29(3):175–194
McDonald S, Page MJ, Beringer K, Wasiak J, Sprowson A (2014) Preoperative education for hip or knee replacement. Cochrane Database Syst Rev. 5:CD 003526
Sanz-Ruiz P, Carbo-Laso E, Alonso-Polo B, Matas-Diez JA, Vaquero-Martín J (2016) Does a new implant design with more physiological kinematics provide better results after knee arthroplasty? Knee 23:399–405
Noble PC, Conditt MA, Cook KF, Mathis KB (2006) The John Insall Award: Patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res 452:35–43
Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD (2010) Patient satisfaction after total knee arthroplasty: Who is satisfied and who is not? Clin Orthop Relat Res 468(1):57–63
Ritter MA, Lutgring JD, Davis KE, Berend ME (2008) The effect of postoperative range of motion on functional activities after posterior cruciate-retaining total knee arthroplasty. J Bone Joint Surg Am 90(4):777–784
Laubenthal KN, Smidt GL, Kettelkamp DB (1972) A quantitative analysis of knee motion during activities of daily living. Phys Ther 52(1):34–43
Kotani A, Yonekura A, Bourne RB (2005) Factors influencing range of motion after contemporary total knee arthroplasty. J Arthroplasty 20(7):850–856
Gocen Z, Sen A, Unver B, Karatosun V, Gunal I (2004) The effect of preoperative physiotherapy and education on the outcome of total hip replacement: a prospective randomized controlled trial. Clin Rehabil 18(4):353–358
Vukomanović A, Popović Z, Durović A, Krstić L (2008) The effects of short-term preoperative physical therapy and education on early functional recovery of patients younger than 70 undergoing total hip arthroplasty. Vojnosanit Pregl 65(4):291–297
Abu Al-Rub Z, Hussaini M, Gerrand CH (2014) What do patients know about their joint replacement implants? Scott Med J 59(3):158–161
Demir F, Ozsaker E, Ilce AO (2008) The quality and suitability of written educational materials for patients*. J Clin Nurs 17(2):259–265
Ayers DC, Franklin PD, Trief PM, Ploutz-Snyder R, Freund D (2004) Psychological attributes of preoperative total joint replacement patients: implications for optimal physical outcome. J Arthroplasty 19(7 Suppl 2):125–130
Nilsdotter AK, Toksvig-Larsen S, Roos EM (2009) A 5 year prospective study of patient-relevant outcomes after total knee replacement. Osteoarthritis Cartilage 17(5):601–606
Papakostidou I, Dailiana ZH, Papapolychroniou T, Liaropoulos L, Zintzaras E, Karachalios TS et al (2012) Factors affecting the quality of life after total knee arthroplasties: a prospective study. BMC Musculoskelet Disord 13:116
Fitzgerald JD, Orav EJ, Lee TH, Marcantonio ER, Poss R, Goldman L et al (2004) Patient quality of life during the 12 months following joint replacement surgery. Arthritis Rheum 51(1):100–109
Acknowledgements
No further acknowledgements.
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
MAPA conceptualized the study and design. DGKB, DSL, MVTR, TFGM and FSM recruited the participants and collected the data. MAPA, GMAS and TVOC prepared the first draft of the manuscript and all authors contributed to writing, as well as review and approval of the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest regarding this research.
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments. The consent obtained from study participants was written and approved by the Ethics Committee. An institutional review board approval from the Ethics Committee of the Universidade Federal de Minas Gerais was obtained for our research protocol to prospective data acquisition of 39 (79) patients undergoing TKA (CAAE:11677714.4.0000.5149), and an informed consent was signed by all the participants or one person responsible for them.
Consent for publication
Not Applicable.
Competing interests
Authors declare that they do not have any financial and non-financial competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Percope de Andrade, M.A., Moreira de Abreu Silva, G., de Oliveira Campos, T.V. et al. A new methodology for patient education in total knee arthroplasty: a randomized controlled trial. Eur J Orthop Surg Traumatol 32, 107–112 (2022). https://doi.org/10.1007/s00590-021-02936-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-021-02936-y