Abstract
Purpose
Injuries to the long bones of the upper limb resulting in bone defects are rare but potentially devastating. Literature on the management of these injuries is limited to case reports and small case series. The aim of this study was to collate the most recent published work on the management of upper limb bone defects to assist with evidence based management when confronted with these cases.
Methods
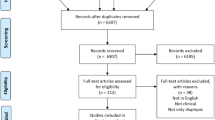
Following a preliminary search that confirmed the paucity of literature and lack of comparative trials, a scoping review using the Preferred Reporting Items for Systematic Reviews and Meta-Analysis extension for Scoping Reviews (PRISMA-ScR) was conducted. A literature search of major electronic databases was conducted to identify journal articles relating to the management of upper limb long bone defects published between 2010 and 2020.
Results
A total of 46 publications reporting on the management of 341 patients were reviewed. Structural autograft, bone transport, one-bone forearm and the induced membrane technique were employed in an almost equal number of cases. The implemented strategies showed similar outcomes but different indications and complication profiles were observed.
Conclusion
Contemporary techniques for the management of post-traumatic upper limb bone defects all produce good results. Specific advantages, disadvantages and complications for each modality should be considered when deciding on which management strategy to employ for each specific patient, anatomical location, and defect size.





Similar content being viewed by others
References
Gan AWT, Puhaindran ME, Pho RWH (2013) The reconstruction of large bone defects in the upper limb. Injury 44(3):313–317. https://doi.org/10.1016/j.injury.2013.01.014
Hu W, Le Nen D, Kerfant N et al (2020) Management of complex forearm defects: a multidisciplinary approach. Ann Chir Plast Esthétique 65(5–6):625–634. https://doi.org/10.1016/j.anplas.2020.06.011
Sackett DL (1993) Rules of evidence and clinical recommendations for the management of patients. Can J Cardiol 9(6):487–489. https://www.ncbi.nlm.nih.gov/pubmed/8221340
Suranigi S, Babu A, Pandian S, Ramdas A, Najimudeen S (2017) Application of the induced membrane technique for treatment of diaphyseal bone defect secondary to osteomyelitis of ulna: a modified approach. J Curr Res Sci Med 3(2):125. https://doi.org/10.4103/jcrsm.jcrsm_59_17
Litvina EA, Semenistyy AA (2020) A case report of extensive segmental defect of the humerus treated with Masquelet technique. J Shoulder Elb Surg 29(7):1368–1374. https://doi.org/10.1016/j.jse.2020.03.018
Allende C (2010) Cement spacers with antibiotics for the treatment of posttraumatic infected nonunions and bone defects of the upper extremity. In: Techniques in hand and upper extremity surgery. https://doi.org/10.1097/BTH.0b013e3181f42bd3
Kawakami R, Konno S-I, Ejiri S, Hatashita S (2015) Surgical treatment for infected long bone defects after limb-threatening trauma: application of locked plate and autogenous cancellous bone graft. Fukushima J Med Sci 61(2):141–148. https://doi.org/10.5387/fms.2015-17
Kyriakopoulos C, Trintafyllopoulos I, Kostakos T, Kostakos A (2016) Implementation of the Masquelet technique in complicated septic non-union of the Ulna—a case report. J Pharm Pharmacol. https://doi.org/10.17265/2328-2150/2016.07.002
Masquelet AC, Kishi T, Benko PE (2019) Very long-term results of post-traumatic bone defect reconstruction by the induced membrane technique. Orthop Traumatol Surg Res 105(1):159–166. https://doi.org/10.1016/j.otsr.2018.11.012
Micev AJ, Kalainov DM, Soneru AP (2015) Masquelet technique for treatment of segmental bone loss in the upper extremity. J Hand Surg Am 40(3):593–598. https://doi.org/10.1016/j.jhsa.2014.12.007
Anoumou NM, Traoré M, Kouamé M, Yepié A, Varango G (2017) Preliminary results of the induced membrane in upper limb. About 6 cases. Hand Surg Rehabil 36(1):53–57. https://doi.org/10.1016/j.hansur.2016.07.007
Kombate NK, Walla A, Ayouba G et al (2017) Reconstruction of traumatic bone loss using the induced membrane technique: preliminary results about 11 cases. J Orthop 14(4):489–494. https://doi.org/10.1016/j.jor.2017.06.009
Bourgeois M, Loisel F, Bertrand D et al (2020) Management of forearm bone loss with induced membrane technique. Hand Surg Rehabil 39(3):171–177. https://doi.org/10.1016/j.hansur.2020.02.002
Walker M, Sharareh B, Mitchell SA (2019) Masquelet reconstruction for posttraumatic segmental bone defects in the forearm. J Hand Surg Am 44(4):342.e1-342.e8. https://doi.org/10.1016/j.jhsa.2018.07.003
Gaillard J, Masquelet AC, Boutroux P, Cambon-Binder A (2020) Induced-membrane treatment of refractory humeral non-union with or without bone defect. Orthop Traumatol Surg Res 106(5):803–811. https://doi.org/10.1016/j.otsr.2020.02.015
Hanna W, Mueller CA (2013) RIA grafting for the treatment of a large bone defect in the distal radius—first case report of a new treatment option. Inj Extra 44(2):19–22. https://doi.org/10.1016/j.injury.2012.10.006
Dhar SA, Dar TA, Mir NA (2019) Management of infected nonunion of the forearm by the Masquelet technique. Strateg Trauma Limb Reconstr 14(1):1–5. https://doi.org/10.5005/jp-journals-10080-1411
Bech N, Kloen P (2020) Recalcitrant Septic Nonunion of the Ulna. Cureus. https://doi.org/10.7759/cureus.7195
Luo TD, Nunez FA, Lomer AA, Nunez FA (2017) Management of recalcitrant osteomyelitis and segmental bone loss of the forearm with the Masquelet technique. J Hand Surg Eur 42(6):640–642. https://doi.org/10.1177/1753193416650171
Giannoudis PV, Harwood PJ, Tosounidis T, Kanakaris NK (2016) Restoration of long bone defects treated with the induced membrane technique: protocol and outcomes. Injury 47:S53–S61. https://doi.org/10.1016/S0020-1383(16)30840-3
Vicenti G, Maruccia M, Carrozzo M, Elia R, Giudice G, Moretti B (2018) Free vascularized osteoseptocutaneous fibular flap for radius shaft nonunion: The final solution when the iliac crest autograft fails. A case report. Injury 49:S63–S70. https://doi.org/10.1016/j.injury.2018.11.030
Noaman HH (2013) Management of upper limb bone defects using free vascularized osteoseptocutaneous fibular bone graft. Ann Plast Surg 71(5):503–509. https://doi.org/10.1097/SAP.0b013e3182a1aff0
Monreal R (2017) free osteocutaneous fibular graft for infected bone defect of the ulna: case report. Juniper Online J Orthop Orthoplastic Surg 1(1):1–4. https://doi.org/10.19080/JOJOOS.2017.01.555551
ElSayed S, Sweed T, El Nakeeb R (2014) Vascularized fibular grafting for reconstruction of bone defect of the radius. Egypt Orthop J 49(3):193. https://doi.org/10.4103/1110-1148.148185
Soucacos PN, Korompilias AV, Vekris MD, Zoubos A, Beris AE (2011) The free vascularized fibular graft for bridging large skeletal defects of the upper extremity. Microsurgery 31(3):190–197. https://doi.org/10.1002/micr.20862
Windhofer C, Michlits W, Karlbauer A, Papp C (2011) Treatment of segmental bone and soft-tissue defects of the forearm with the free osteocutaneous lateral arm flap. J Trauma Inj Infect Crit Care 70(5):1286–1290. https://doi.org/10.1097/TA.0b013e3182095df5
Cavadas PC, Thione A (2014) Skeletal reconstruction of the forearm with a double-barrel fibular flap and second metatarsal head. Injury 45(12):2106–2108. https://doi.org/10.1016/j.injury.2014.10.014
Cano-Luís P, Andrés-Cano P, Ricón-Recarey FJ, Giráldez-Sánchez MA (2018) Treatment of posttraumatic bone defects of the forearm with vascularized fibular grafts. Follow up after fourteen years. Injury 49(Suppl 2):S27–S35. https://doi.org/10.1016/j.injury.2018.07.021
Gopisankar G, Justin ASV, Nithyananth M, Cherian VM, Lee VN (2011) Non-vascularised fibular graft as an intramedullary strut for infected non-union of the humerus. J Orthop Surg (Hong Kong) 19(3):341–345. https://doi.org/10.1177/230949901101900316
Wang C, Xu J, Wen G, Chai Y (2018) Reconstruction of complex tissue defect of forearm with a chimeric flap composed of a sural neurocutaneous flap and a vascularized fibular graft: a case report. Microsurgery 38(7):790–794. https://doi.org/10.1002/micr.30334
Molina AR, Ali E, van Rensburg L, Malata CM (2010) Successful reconstruction of a gunshot segmental defect of the radius with a free vascularised fibular osteocutaneous flap. J Plast Reconstr Aesthetic Surg 63(12):2181–2184. https://doi.org/10.1016/j.bjps.2010.03.022
Kashayi-Chowdojirao S, Vallurupalli A, Chilakamarri VK et al (2017) Role of autologous non-vascularised intramedullary fibular strut graft in humeral shaft nonunions following failed plating. J Clin Orthop Trauma 8:S21–S30. https://doi.org/10.1016/j.jcot.2016.12.006
Demir B, Ozkul B, Lapcin O, Beng K, Arikan Y, Yalcinkaya M (2019) A modification of internal bone transport method for reconstruction of nonunion of forearm. Indian J Orthop 53(1):196. https://doi.org/10.4103/ortho.IJOrtho_52_17
Birkholtz F, Greyling P (2016) Independent segmental bone transport of the radius and ulna: a case report. SA Orthop J. https://doi.org/10.17159/2309-8309/2016/v15n2a4
Liu T, Zhang X, Li Z, Zeng W (2012) Management of chronic radial head dislocation associated with segment bone defect in ulna after osteomyelitis. J Trauma Acute Care Surg 73(4):1014–1017. https://doi.org/10.1097/TA.0b013e318254a933
Zhang Q, Yin P, Hao M et al (2014) Bone transport for the treatment of infected forearm nonunion. Injury 45(12):1880–1884. https://doi.org/10.1016/j.injury.2014.07.029
Ditsios K, Iosifidou E, Kostretzis L et al (2017) Combined bone transportation and lengthening techniques for the treatment of septic nonunion of the forearm followed by tendon transfer. Case Rep Orthop 2017:1–4. https://doi.org/10.1155/2017/9672126
Liu T, Liu Z, Ling L, Zhang X (2013) Infected forearm nonunion treated by bone transport after debridement. BMC Musculoskelet Disord 14(1):273. https://doi.org/10.1186/1471-2474-14-273
Eljabu W, Fabian C, Wissmann K, Reichstein K (2013) Segmental bone transport with the monorail technique in reconstructing a bone defect in the forearm. JBJS Case Connect 3(3):e87. https://doi.org/10.2106/JBJS.CC.L.00298
Liu Y, Yushan M, Liu Z, Liu J, Ma C, Yusufu A (2020) Treatment of diaphyseal forearm defects caused by infection using Ilizarov segmental bone transport technique. BMC Musculoskelet Disord. https://doi.org/10.21203/rs.3.rs-97249/v1
Kliushin NM, Stepanenko P, Mekki WA (2019) Treatment of forearm diaphyseal defect by distraction compression bone transport and continued distraction for radial head reduction: A case study. Chinese J Traumatol = Zhonghua chuang shang za zhi 22(5):304–307. https://doi.org/10.1016/j.cjtee.2019.04.005
Ebied A, Elseedy A (2018) Treatment of infected nonunion of forearm bones by ring external fixator. Egypt Orthop J 53:341–347. https://doi.org/10.4103/eoj.eoj_71_18
Borzunov DY, Shastov AL (2019) Mechanical solutions to salvage failed distraction osteogenesis in large bone defect management. Int Orthop 43(5):1051–1059. https://doi.org/10.1007/s00264-018-4032-6
Devendra A, Velmurugesan PS, Dheenadhayalan J, Venkatramani H, Sabapathy SR, Rajasekaran S (2019) One-bone forearm reconstruction. J Bone Jt Surg 101(15):e74. https://doi.org/10.2106/JBJS.18.01235
Wang Y, Zhou M, Wu Y, Ma Y, Liu J, Rui Y (2020) One-bone forearm reconstruction and distal radioulnar joint fusion for emergency one-stage operation in traumatic major bone defect of forearm. Injury 51(8):1828–1833. https://doi.org/10.1016/j.injury.2020.06.024
Kim SY, Chim H, Bishop AT, Shin AY (2017) Complications and outcomes of one-bone forearm reconstruction. HAND 12(2):140–144. https://doi.org/10.1177/1558944716643305
Jacoby SM, Bachoura A, DiPrinzio EV, Culp RW, Osterman AL (2013) Complications following one-bone forearm surgery for posttraumatic forearm and distal radioulnar joint instability. J Hand Surg Am 38(5):976-982.e1. https://doi.org/10.1016/j.jhsa.2013.02.005
Attias N, Thabet AM, Prabhakar G, Dollahite JA, Gehlert RJ, DeCoster TA (2018) Management of extra-articular segmental defects in long bone using a titanium mesh cage as an adjunct to other methods of fixation. Bone Joint J 100-B(5):646–651. https://doi.org/10.1302/0301-620X.100B5.BJJ-2017-0817.R2
Kerfant N, Valenti P, Kilinc AS, Falcone MO (2012) Free vascularised fibular graft in multi-operated patients for an aseptic non-union of the humerus with segmental defect: Surgical technique and results. Orthop Traumatol Surg Res 98(5):603–607. https://doi.org/10.1016/j.otsr.2012.03.013
Kucukkaya M, Armagan R, Kuzgun U (2009) The new intramedullary cable bone transport technique. J Orthop Trauma 23(7):531–536. https://doi.org/10.1097/BOT.0b013e3181a2a8e7
Kusnezov N, Dunn JC, Stewart J, Mitchell JS, Pirela-Cruz M (2015) Acute limb shortening for major near and complete upper extremity amputations with associated neurovascular injury: a review of the literature. Orthop Surg 7(4):306–316. https://doi.org/10.1111/os.12213
Wang S, Li P, Xue Y, Yiu H, Li Y-C, Wang H (2013) Contralateral C7 nerve transfer with direct coaptation to restore lower trunk function after traumatic brachial plexus avulsion. J Bone Jt Surg 95(9):821–827. https://doi.org/10.2106/JBJS.L.00039
Brady RJ, Dean JB, Skinner TM, Gross MT (2003) Limb length inequality: clinical implications for assessment and intervention. J Orthop Sport Phys Ther 33(5):221–234. https://doi.org/10.2519/jospt.2003.33.5.221
Kiss S, Pap K, Vizkelety T, Terebessy T, Balla M, Szoke G (2008) The humerus is the best place for bone lengthening. Int Orthop 32(3):385–388. https://doi.org/10.1007/s00264-007-0327-8
Liu T, Zhang X, Li Z, Zeng W, Peng D, Sun C (2008) Callus distraction for humeral nonunion with bone loss and limb shortening caused by chronic osteomyelitis. J Bone Jt Surg Br 90(6):795–800. https://doi.org/10.1302/0301-620X.90B6.20392
Khan MS, Sahibzada AS, Khan MA, Sultan S, Younas M, Khan AZ (2005) Outcome of plating, bone grafting and shortening of non-union humeral diaphyseal fracture. J Ayub Med Coll Abbottabad 17(2):44–46. http://www.ncbi.nlm.nih.gov/pubmed/16092650
Brennan ML, Taitsman LA, Barei DP, Puttler E, Nork SE (2008) Shortening osteotomy and compression plating for atrophic humeral nonunions: surgical technique. J Orthop Trauma 22(9):643–647. https://doi.org/10.1097/BOT.0b013e318177eb23
Aronson J (1994) Temporal and spatial increases in blood flow during distraction osteogenesis. Clin Orthop Relat Res (301):124–131. http://www.ncbi.nlm.nih.gov/pubmed/8156663
Chauhan C, Howard A, Saleh M (1995) Severely comminuted forearm fracture treated with acute shortening. Injury 26(6):415–416. https://doi.org/10.1016/0020-1383(95)00036-9
Sharma H, Colleary G, Marsh D (2004) Acute forearm shortening. Injury 35(5):531–533. https://doi.org/10.1016/S0020-1383(02)00175-4
Masquelet AC, Fitoussi F, Begue T, Muller GP (2000) [Reconstruction of the long bones by the induced membrane and spongy autograft]. Ann Chir Plast Esthet 45(3):346–353. http://www.ncbi.nlm.nih.gov/pubmed/10929461
Karger C, Kishi T, Schneider L et al (2012) Treatment of posttraumatic bone defects by the induced membrane technique. Orthop Traumatol Surg Res 98(1):97–102. https://doi.org/10.1016/j.otsr.2011.11.001
Calori GM, Giannoudis PV, Mazzola S, Colombo M (2016) Application of the induced membrane technique for forearm bone defects. Tech Orthop 31(1):29–41. https://doi.org/10.1097/BTO.0000000000000139
Pincher B, Fenton C, Jeyapalan R, Barlow G, Sharma HK (2019) A systematic review of the single-stage treatment of chronic osteomyelitis. J Orthop Surg Res 14(1):4–11. https://doi.org/10.1186/s13018-019-1388-2
Mathieu L, Durand M, Demoures T, Steenman C, Masquelet A-C, Collombet J-M (2020) Repeated induced-membrane technique failure without infection: a series of three consecutive procedures performed for a single femur defect. Case Rep Orthop 2020:1–7. https://doi.org/10.1155/2020/8892226
Mathieu L, Durand M, Collombet J-M, de Rousiers A, de l’Escalopier N, Masquelet A-C (2020) Induced membrane technique: a critical literature analysis and proposal for a failure classification scheme. Eur J Trauma Emerg Surg. https://doi.org/10.1007/s00068-020-01540-9
Barbieri CH, Mazzer N, Aranda CA, Pinto MM (1997) Use of a bone block graft from the iliac crest with rigid fixation to correct diaphyseal defects of the radius and ulna. J Hand Surg Br 22(3):395–401. https://doi.org/10.1016/s0266-7681(97)80411-1
Song H-R, Kale A, Park H-B et al (2003) Comparison of internal bone transport and vascularized fibular grafting for femoral bone defects. J Orthop Trauma 17(3):203–211. https://doi.org/10.1097/00005131-200303000-00009
Dumont CE, Exner UG (2009) Reconstruction of large diaphyseal defects of the femur and the tibia with autologous bone. Eur J Trauma Emerg Surg 35(1):17–25. https://doi.org/10.1007/s00068-008-8224-4
Hollenbeck ST, Komatsu I, Woo S et al (2011) The current role of the vascularized-fibular osteocutaneous graft in the treatment of segmental defects of the upper extremity. Microsurgery 31(3):183–189. https://doi.org/10.1002/micr.20703
Hallock GG (2005) Free-flap monitoring using a chimeric sentinel muscle perforator flap. J Reconstr Microsurg 21(6):351–354. https://doi.org/10.1055/s-2005-915200
Ferreira N, Marais LC (2015) Bone transport through an induced membrane in the management of tibial bone defects resulting from chronic osteomyelitis. Strateg Trauma Limb Reconstr 10(1):27–33. https://doi.org/10.1007/s11751-015-0221-7
Allende C, Allende BT (2004) Posttraumatic one-bone forearm reconstruction. J Bone Jt Surg 86(2):364–369. https://doi.org/10.2106/00004623-200402000-00022
Javaid M, Haleem A (2018) Additive manufacturing applications in orthopaedics: a review. J Clin Orthop Trauma 9(3):202–206. https://doi.org/10.1016/j.jcot.2018.04.008
Javaid M, Haleem A (2019) Current status and challenges of additive manufacturing in orthopaedics: an overview. J Clin Orthop Trauma 10(2):380–386. https://doi.org/10.1016/j.jcot.2018.05.008
Tetsworth K, Woloszyk A, Glatt V (2019) 3D printed titanium cages combined with the Masquelet technique for the reconstruction of segmental femoral defects. OTA Int 2(1):e016. https://doi.org/10.1097/oi9.0000000000000016
O’Malley NT, Kates SL (2012) Advances on the Masquelet technique using a cage and nail construct. Arch Orthop Trauma Surg 132(2):245–248. https://doi.org/10.1007/s00402-011-1417-z
Attias N, Lehman RE, Bodell LS, Lindsey RW (2005) Surgical management of a long segmental defect of the humerus using a cylindrical titanium mesh cage and plates. J Orthop Trauma 19(3):211–216. https://doi.org/10.1097/00005131-200503000-00011
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The authors declare that this submission is in accordance with the principles laid down by the Responsible Research Publication Position Statements as developed at the 2nd World Conference on Research Integrity in Singapore, 2010.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ferreira, N., Saini, A.K., Birkholtz, F.F. et al. Management of segmental bone defects of the upper limb: a scoping review with data synthesis to inform decision making. Eur J Orthop Surg Traumatol 31, 911–922 (2021). https://doi.org/10.1007/s00590-021-02887-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-021-02887-4