Abstract
Background
The aim of this study is to compare 2 groups of total knee arthroplasties (TKAs): the bicruciate-retaining (BCR—group) and cruciate-retaining total knee arthroplasty (CR—group), evaluating the functional results in the short-term follow-up.
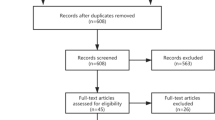
Methods
24 BCR were included in the study and were compared with a group of 24 TKAs performed with the same implant, but with sacrifice of the ACL and retention of the posterior cruciate ligament. For preoperative and postoperative clinical evaluation, the visual analogue score (VAS) and the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) were used. Radiological evaluation included weight-bearing long-leg view, a Rosemberg view, lateral view of the knee and tangential view of the patella. Hip-knee-ankle angle (HKA) was recorded pre and postoperatively. Radiolucent lines (RLLs) were evaluated according the Knee Society Roentgenographic Evaluation System (KSRES).
Results
At last follow-up the mean VAS score was 1.81 for BCR group and 1.43 for CR group (p = 0.61). The mean WOMAC score was 8.68 for BCR group and 12.81 for CR group (p = 0.33). As for the radiological evaluation, preoperative HKA angle was 0.53° varus for BCR group and 3.14° varus for CR group (p = 0.24); postoperative HKA was 0.72° valgus for BCR group and 0.38° valgus for CR group (p = 0.75). The percentage of RLLs was similar between the two groups (12% versus 15%).
Conclusions
BCR-TKA has showed to give similar functional and radiographic outcomes compared to conventional CR-TKA in a similar cohort of patients. An higher operative times and higher number of complications respect were found in BCR group. These results can be explained by the early learning curve experiences. Future randomized controlled trials should be performed to support new implant designs such as BCR.
Level of evidence
Level of evidence Case–control study, level III.
Similar content being viewed by others
References
Rivière C, Iranpour F, Auvinet E, Howell S, Vendittoli PA, Cobb J, Parratte S (2017) Alignment options for total knee arthroplasty: a systematic review. Orthop Traumatol Surg Res 103(7):1047–1056. https://doi.org/10.1016/j.otsr.2017.07.010
Klemt C, Drago J, Oganesyan R, Smith EJ, Yeo I, Kwon YM (2020) Gait and knee flexion in vivo kinematics of asymmetric tibial polyethylene geometry cruciate retaining total knee arthroplasty. J Knee Surg. https://doi.org/10.1055/s-0040-1718681
Koh IJ, Chalmers CE, Lin CC, Park SB, McGarry MH, Lee TQ (2020) Posterior stabilized total knee arthroplasty reproduces natural joint laxity compared to normal in kinematically aligned total knee arthroplasty: a matched pair cadaveric study. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-020-03624-y
Zhang Q, Chen Z, Zhang Z, Jin Z, Muratoglu OK, Varadarajan KM (2020) Leveraging subject-specific musculoskeletal modeling to assess effect of anterior cruciate ligament retaining total knee arthroplasty during walking gait. Proc Inst Mech Eng H. https://doi.org/10.1177/0954411920947204
Parcells BW, Tria AJ Jr (2016) The cruciate ligaments in total knee arthroplasty. Am J Orthop (Belle Mead NJ) 45:E153–E160
Arauz P, Klemt C, Limmahakhun S, An S, Kwon YM (2019) Stair climbing and high knee flexion activities in bi-cruciate retaining total knee arthroplasty. in vivo kinematics and articular contact analysis. J Arthroplasty 34:570–576. https://doi.org/10.1016/j.arth.2018.11.013
Relph N, Herrington L, Tyson S (2014) The effects of ACL injury on knee proprioception: a meta-analysis. Physiotherapy 100:187–195. https://doi.org/10.1016/j.physio.2013.11.002
Wodowski AJ, Swigler CW, Liu H, Nord KM, Toy PC, Mihalko WM (2016) Proprioception and knee arthroplasty: a literature review. Orthop Clin North Am 47:301–309. https://doi.org/10.1016/j.ocl.2015.09.005
Sabouret P, Lavoie F, Cloutier JM (2013) Total knee replacement with retention of both cruciate ligaments: a 22-year follow-up study. Bone Jt J 95-B(7):917–922. https://doi.org/10.1302/0301-620X.95B7.30904
Pritchett JW (2015) Bicruciate-retaining total knee replacement provides satisfactory function and implant survivorship at 23 years. Clin Orthop Relat Res 473:2327–2333. https://doi.org/10.1007/s11999-015-4219-8
Boese CK, Ebohon S, Ries C, De Faoite D (2020) Bi-cruciate retaining total knee arthroplasty: a systematic literature review of clinical outcomes. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-020-03622-0
Iriuchishima T, Ryu K (2019) Bicruciate substituting total knee arthroplasty improves stair climbing ability when compared with cruciate-retain or posterior stabilizing total knee arthroplasty. Indian J Orthop 53:641–645. https://doi.org/10.4103/ortho.IJOrtho_392_18
Huang W, Zhang Y, Yao Z, Ma L (2016) Clinical examination of anterior cruciate ligament rupture: a systematic review and meta-analysis. Acta Orthop Traumatol Turc 50:22–31. https://doi.org/10.3944/AOTT.2016.14.0283
De Faoite D, Ries C, Foster M, Boese CK (2020) Indications for bi-cruciate retaining total knee replacement: an international survey of 346 knee surgeons. PLoS ONE 15:e0234616. https://doi.org/10.1371/journal.pone.0234616
Haefeli M, Elfering A (2006) Pain assessment. Eur Spine J 15:S17-24. https://doi.org/10.1007/s00586-005-1044-x
Salaffi F, Leardini G, Canesi B, Mannoni A, Fioravanti A, Caporali R, Lapadula G, Punzi L; GOnorthrosis and Quality Of Life Assessment (GOQOLA) (2003) Reliability and validity of the Western Ontario and McMaster universities (WOMAC) osteoarthritis index in Italian patients with osteoarthritis of the knee. Osteoarthr Cartil 11:551–560. https://doi.org/10.1016/s1063-4584(03)00089-x
Clément J, Blakeney W, Hagemeister N, Desmeules F, Mezghani N, Lowry V, Vendittoli PA (2019) Hip-knee-ankle (HKA) angle modification during gait in healthy subjects. Gait Posture 72:62–68. https://doi.org/10.1016/j.gaitpost.2019.05.025
Costales TG, Chapman DM, Dalury DF (2020) The natural history of radiolucencies following uncemented total knee arthroplasty at 9 years. J Arthroplasty 35:127–131. https://doi.org/10.1016/j.arth.2019.08.032
Zhou K, Yu H, Li J, Wang H, Zhou Z, Pei F (2018) No difference in implant survivorship and clinical outcomes between full-cementless and full-cemented fixation in primary total knee arthroplasty: a systematic review and meta-analysis. Int J Surg 53:312–319. https://doi.org/10.1016/j.ijsu.2018.04.015
D’Elicio DG, Attanasio M, Ruffo G, Mogos S, Ursino N, D’Ambrosi R, Parente F (2020) Improving radiographic patello-femoral tracking in total knee arthroplasty with the use of a flexion spacer: a case-control study. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-020-05991-w
Okada Y, Teramoto A, Takagi T, Yamakawa S, Sakakibara Y, Shoji H, Watanabe K, Fujimiya M, Fujie H, Yamashita T (2018) ACL function in bicruciate-retaining total knee arthroplasty. J Bone Jt Surg Am 100:e114. https://doi.org/10.2106/JBJS.18.00099
Heyse TJ, Slane J, Peersman G, Dirckx M, van de Vyver A, Dworschak P, Fuchs-Winkelmann S, Scheys L (2017) Kinematics of a bicruciate-retaining total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25:1784–1791. https://doi.org/10.1007/s00167-016-4414-5
Tsai TY, Liow MHL, Li G, Arauz P, Peng Y, Klemt C, Kwon YM (2019) Bi-cruciate retaining total knee arthroplasty does not restore native tibiofemoral articular contact kinematics during gait. J Orthop Res 37:1929–1937. https://doi.org/10.1002/jor.24333
Planckaert C, Larose G, Ranger P, Lacelle M, Fuentes A, Hagemeister N (2018) Total knee arthroplasty with unexplained pain: new insights from kinematics. Arch Orthop Trauma Surg 138:553–561. https://doi.org/10.1007/s00402-018-2873-5
Flierl MA, Sobh AH, Culp BM, Baker EA, Sporer SM (2019) Evaluation of the painful total knee arthroplasty. J Am Acad Orthop Surg 27:743–751. https://doi.org/10.5435/JAAOS-D-18-00083
Lombardi AV, McClanahan AJ, Berend KR (2015) The bicruciate-retaining TKA: two is better than one. Semin Arthroplasty 26:51–58. https://doi.org/10.1053/J.SART.2015.08.004
Pritchett JW (2011) Patients prefer a bicruciate-retaining or the medial pivot total knee prosthesis. J Arthroplasty 26:224–228. https://doi.org/10.1016/j.arth.2010.02.012
Alnachoukati OK, Emerson RH, Diaz E, Ruchaud E, Ennin KA (2018) Modern day bicruciate-retaining total knee arthroplasty: a short-term review of 146 knees. J Arthroplasty 33:2485–2490. https://doi.org/10.1016/j.arth.2018.03.026
Baumann F, Bahadin Ö, Krutsch W, Zellner J, Nerlich M, Angele P, Tibesku CO (2017) Proprioception after bicruciate-retaining total knee arthroplasty is comparable to unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25:1697–1704. https://doi.org/10.1007/s00167-016-4121-2
Christensen JC, Brothers J, Stoddard GJ, Anderson MB, Pelt CE, Gililland JM, Peters CL (2017) Higher frequency of reoperation with a new bicruciate-retaining total knee arthroplasty. Clin Orthop Relat Res 475:62–69. https://doi.org/10.1007/s11999-016-4812-5
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Biazzo, A., D’Ambrosi, R., Staals, E. et al. Early results with a bicruciate-retaining total knee arthroplasty: a match-paired study. Eur J Orthop Surg Traumatol 31, 785–790 (2021). https://doi.org/10.1007/s00590-020-02834-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-020-02834-9