Abstract
Background
Infection is a truly devastating complication of total joint arthroplasty, causing most patients to undergo a revision surgery, and to bear significant psychological and financial burden. The purpose of this study is to systematically evaluate the literature to determine the efficacy and complication profile of local antibiotic application in primary total joint arthroplasty.
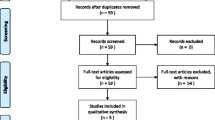
Methods
All studies of primary total joint arthroplasty which assessed local antibiotics in any form other than antibiotic-impregnated cement as an intervention were included. Studies that reported at least one outcome related to infection and were available in full text in English were eligible for inclusion. Studies which included both primary and revision cases but did not report the stratified data for each type of surgery and studies on fracture populations were excluded.
Results
A total of 9 studies involving 3,714 cases were included. The pooled deep infection rate was 1.6% in the intervention groups and 3.5% in the control groups. Meta-analysis revealed a RR of 0.53 (95%CI: 0.35–0.79, p = 0.002) with no heterogeneity (I2 = 0%) for infection in the intervention groups. Meta-analysis revealed a non-significant reduction in superficial infection rates in the intervention groups; however, there was a significant increase in aseptic wound complications in the intervention groups.
Conclusion
Local antibiotic application results in a moderate reduction in deep infection rates in primary total joint arthroplasty, with no significant impact on superficial infection rates. However, local antibiotic application may be associated with a moderate increase in aseptic wound complications.




Similar content being viewed by others
References
Riesgo AM, Liporace FA (2018) Strategies for management of periprosthetic joint infection. Bull Hosp Joint Dis 76(1):55–61
Kunutsor SK, Beswick AD, Peters TJ et al (2017) Health care needs and support for patients undergoing treatment for prosthetic joint infection following hip or knee arthroplasty: a systematic review. PLoS ONE. https://doi.org/10.1371/journal.pone.0169068
Eka A, Chen AF (2015) Patient-related medical risk factors for periprosthetic joint infection of the hip and knee. Ann Transl Med. https://doi.org/10.3978/j.issn.2305-5839.2015.09.26
Graves N, Wloch C, Wilson J et al (2016) A cost-effectiveness modelling study of strategies to reduce risk of infection following primary hip replacement based on a systematic review. Health Technol Assess (Rockv). https://doi.org/10.3310/hta20540
Hinarejos P, Guirro P, Leal J et al (2013) The use of erythromycin and colistin-loaded cement in total knee arthroplasty does not reduce the incidence of infection : a prospective randomized study in 3000 knees. J Bone Jt Surg Ser A. https://doi.org/10.2106/JBJS.L.00901
Zhang J, Zhang XY, Jiang FL et al (2019) Antibiotic-impregnated bone cement for preventing infection in patients receiving primary total hip and knee arthroplasty: a meta-analysis. Med (United States). https://doi.org/10.1097/MD.0000000000018068
Symonds T, Parkinson B, Hazratwala K et al (2018) Use of regional administration of prophylactic antibiotics in total knee arthroplasty. ANZ J Surg . https://doi.org/10.1111/ans.14816
Xie LL, Zhu J, Yang MS et al (2017) Effect of intra-wound vancomycin for spinal surgery: a systematic review and meta-analysis. Orthop Surg. https://doi.org/10.1111/os.12356
Watters WC, Baisden J, Bono CM et al (2009) Antibiotic prophylaxis in spine surgery: an evidence-based clinical guideline for the use of prophylactic antibiotics in spine surgery. Spine J. https://doi.org/10.1016/j.spinee.2008.05.008
Heckmann ND, Mayfield CK, Culvern CN et al (2019) Systematic review and meta-analysis of intrawound vancomycin in total hip and total knee arthroplasty: a call for a prospective randomized trial. J Arthroplasty. https://doi.org/10.1016/j.arth.2019.03.071
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (eds) (2019) Cochrane Handbook for Systematic Reviews of Interventions, 2nd edn. John Wiley & Sons, Chichester, UK
Moher D, Liberati A, Tetzlaff J et al (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. https://doi.org/10.1371/journal.pmed.1000097
Ouzzani M, Hammady H, Fedorowicz Z et al (2016) Rayyan-a web and mobile app for systematic reviews. Syst Rev. https://doi.org/10.1186/s13643-016-0384-4
Viswanathan M, Patnode C, Berkman ND, et al (2018) Assessing the risk of bias in systematic reviews of health care interventions. In: Methods guide for comparative effectiveness reviews (Prepared by the Scientific Resource Center under Contract No. 290-2012-0004-C). https://doi.org/10.23970/AHRQEPCMETHGUIDE2
Slim K, Nini E, Forestier D et al (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 73:712–716
McHugh ML (2012) Interrater reliability the kappa statistic. Biochem Medica. https://doi.org/10.1613/bm.2012.031
Cohen EM, Marcaccio S, Goodman AD et al (2019) Efficacy and cost-effectiveness of topical vancomycin powder in primary cementless total hip arthroplasty. Orthopedics. https://doi.org/10.3928/01477447-20190321-05
Hanada M, Nishikino S, Hotta K et al (2019) Intrawound vancomycin powder increases post-operative wound complications and does not decrease periprosthetic joint infection in primary total and unicompartmental knee arthroplasties. Knee Surg, Sport Traumatol Arthrosc. https://doi.org/10.1007/s00167-019-05498-z
Khatri K, Bansal D, Singla R et al (2017) Prophylactic intrawound application of vancomycin in total knee arthroplasty. J Arthrosc Jt Surg. https://doi.org/10.1016/j.jajs.2017.08.001
de Oliveira CLT, Elias FA, Ribacionka ADS et al (2019) Does topical use of gentamicin reduce the infection rate in primary total hip arthroplasty? Acta Ortop Bras. https://doi.org/10.1590/1413-785220192704219177
Patel NN, Guild GN, Kumar AR (2018) Intrawound vancomycin in primary hip and knee arthroplasty: a safe and cost-effective means to decrease early periprosthetic joint infection. Arthroplast Today. https://doi.org/10.1016/j.artd.2018.07.011
Winkler C, Dennison J, Wooldridge A et al (2018) Do local antibiotics reduce periprosthetic joint infections? a retrospective review of 744 cases. J Clin Orthop Trauma. https://doi.org/10.1016/j.jcot.2017.08.007
Assor M (2010) Noncemented total knee arthroplasty with a local prophylactic anti-infection agent: a prospective series of 135 cases. Can J Surg 53(1):47
Dial BL, Lampley AJ, Green CL et al (2018) Intrawound vancomycin powder in primary total hip arthroplasty increases rate of sterile wound complications. Hip Pelvis. https://doi.org/10.5371/hp.2018.30.1.37
Yavuz IA, Oken OF, Yildirim AO et al (2019) No effect of vancomycin powder to prevent infection in primary total knee arthroplasty: a retrospective review of 976 cases. Knee Surg, Sport Traumatol Arthrosc. https://doi.org/10.1007/s00167-019-05778-8
Youssef J, Orndorff D, Scott M et al (2014) Sterile seroma resulting from multilevel xlif procedure as possible adverse effect of prophylactic vancomycin powder: a case report. Evid Based Spine Care J. https://doi.org/10.1055/s-0034-1386754
Kurtz SM, Lau E, Watson H et al (2012) Economic burden of periprosthetic joint infection in the united states. J Arthroplasty. https://doi.org/10.1016/j.arth.2012.02.022
Rennert-May ED, Conly J, Smith S et al (2018) The cost of managing complex surgical site infections following primary hip and knee arthroplasty: a population-based cohort study in Alberta Canada. Infect Control Hosp Epidemiol. https://doi.org/10.1017/ice.2018.199
Abdullah K, Chen H, Lucas T (2016) Safety of topical vancomycin powder in neurosurgery. Surg Neurol Int. https://doi.org/10.4103/2152-7806.195227
Godil SS, Parker SL, O’Neill KR et al (2013) Comparative effectiveness and cost-benefit analysis of local application of vancomycin powder in posterior spinal fusion for spine trauma Presented at the 2013 joint spine section meeting clinical article. J Neurosurg Spine. https://doi.org/10.3171/2013.6.SPINE121105
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Author Mohit Bhandari is a consultant for Sanofi, Pendopharm, and Ferring Pharmaceuticals, and received research grants from Sanofi, Ferring Pharmaceuticals, DJ Orthopedics, Acumed, Anika Therapeutics, and Flexion Therapeutics. Other authors have no conflict of interest to disclose. No funds were received in support of this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1: Eligibility criteria
1. Inclusion criteria |
2. Adult population |
3. All primary surgical techniques (no revision) |
4. Clinical outcomes reported |
5. Human Studies |
6. Total knee and hip arthroplasty only |
7. Prophylactic local antibiotics in non-infected joint |
Exclusion criteria |
1. Inverse of inclusion criteria |
2. Review, technical, anatomic, pharmacologic, or otherwise non-prognostic articles |
3. Use of antibiotic impregnated cement |
4. Non-English studies |
5. Population >10% with previous surgery to joint of interest |
Appendix 2: Full search strategy. Search Date: November 3, 2019
Embase (1534) | Medline1(979) |
|---|---|
1. exp hip arthroplasty/ or exp knee arthroplasty/ or exp arthroplasty/ or exp total knee arthroplasty/ or exp replacement arthroplasty/ or exp total arthroplasty/ or ("total hip" or "total knee").ti,ab,kw. 2. (bacter* or antibio*).ti,ab,kw. or exp antibiotic agent/ 3. ("local" or regional* or powder* or topical* or tissue*).ti,ab,kw. 4. 1 and 2 and 3 | 1. Arthroplasty, Replacement, Knee/ or Arthroplasty, Replacement, Hip/ or ("total hip" or "total knee").ti,ab,kf. 2. exp Anti-Bacterial Agents/ (bacter* or antib*).ti,ab,kf. 3. ("local" or region* or topical* or powder* or wound* or tissue*).ti,ab,kf. 4. 1 and 2 and 3 |
-
1.
OVID Medline Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid MEDLINE(R) Daily and Ovid MEDLINE(R) 1946 to Present
Web of Science (8) |
|---|
TOPIC: (TOPIC: (("total hip" or "total knee")) AND TOPIC: ((antibact* or antibiot*)) AND TOPIC: ((local* or topical* or tissue* or regional*))) |
Timespan: All years. |
Indexes: SCI-EXPANDED. |
Rights and permissions
About this article
Cite this article
Saidahmed, A., Sarraj, M., Ekhtiari, S. et al. Local antibiotics in primary hip and knee arthroplasty: a systematic review and meta-analysis. Eur J Orthop Surg Traumatol 31, 669–681 (2021). https://doi.org/10.1007/s00590-020-02809-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-020-02809-w