Abstract
Aims
The safety and efficacy of tranexamic acid (TXA) in reducing blood loss after total joint arthroplasty and spinal fusion surgery has been well documented. However, little data exist regarding the effectiveness of intraoperative TXA in children with cerebral palsy (CP). The aim of this double cohort study is to investigate the safety and efficacy of intraoperative TXA in reducing blood loss and transfusion requirements for children with CP undergoing a proximal unilateral or bilateral femoral varus derotational osteotomy (VDRO).
Patients and methods
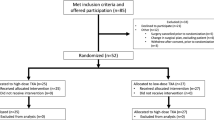
A retrospective review was performed of all paediatric theatre lists between May 2012 and January 2019 for all paediatric (< 16 years old) CP patients who underwent unilateral or bilateral VDRO combined with soft tissue release at our institution. Fifty-one patients were included in our study further subdivided into two individual groups, unilateral and bilateral VDRO.
Results
No statistically significant differences were found in demographics such as age, weight, ASA, GMFCS and antiepileptic medication between the groups. However, there were significant statistically differences in TBL and transfusion rates between the groups that received TXA and those that did not, both in unilateral [241 ml (TXA) vs. 369 ml (non-TXA)] and bilateral [287 ml (TXA) vs. 467 ml (non-TXA)] operations.
Conclusion
TXA successfully reduced TBL (in both TXA subgroups) and the transfusion rates without associated complications. TXA’s safety and efficacy should be explored further in adequately powered randomized controlled trials.




Similar content being viewed by others
References
Oskoui M, Coutinho F, Dykeman J, Jette N, Pringsheim T (2013) An update on the prevalence of cerebral palsy: a systematic review and meta-analysis. Dev Med Child Neurol 55(6):509–519
Alassaf N, Saran N, Benaroch T, Hamdy RC (2018) Combined pelvic and femoral reconstruction in children with cerebral palsy. J Int Med Res 46(1):475–484
Schwartz MH, Rozumalski A, Novacheck TF (2014) Femoral derotational osteotomy: surgical indications and outcomes in children with cerebral palsy. Gait Posture 39(2):778–783
Chambers HG, Weinstein CH, Mubarak SJ, Wenger DR, Silva PD (1999) The effect of valproic acid on blood loss in patients with cerebral palsy. J Pediatr Orthop 19(6):792–795
Majid I, Alshryda S, Somanchi B, Morakis E, Foster A (2015) The value of tranexamic acid in reducing blood loss following hip reconstruction in children with cerebral palsy. J Blood Transfus 2015:827027
Tzatzairis TK, Drosos GI, Kotsios SE, Ververidis AN, Vogiatzaki TD, Kazakos KI (2016) Intravenous vs topical tranexamic acid in total knee arthroplasty without tourniquet application: a randomized controlled study. J Arthroplas 31(11):2465–2470
Sui WY, Ye F, Yang JL (2016) Efficacy of tranexamic acid in reducing allogeneic blood products in adolescent idiopathic scoliosis surgery. BMC Musculoskelet Disord 17:187
Zhang Y, Zhang X, Wang Y, Shi J, Yuan S, Duan F et al (2019) Efficacy and safety of tranexamic acid in pediatric patients undergoing cardiac surgery: a single-center experience. Front Pediatr 7:181
Urban D, Dehaeck R, Lorenzetti D, Guilfoyle J, Poon MC, Steele M et al (2016) Safety and efficacy of tranexamic acid in bleeding paediatric trauma patients: a systematic review protocol. BMJ Open 6(9):e012947
Themistoklis T, Theodosia V, Konstantinos K, Georgios DI (2017) Perioperative blood management strategies for patients undergoing total knee replacement: where do we stand now? World J Orthop 8(6):441–454
Nazareth A, Shymon SJ, Andras L, Goldstein RY, Kay RM (2019) Impact of tranexamic acid use on blood loss and transfusion rates following femoral varus derotational osteotomy in children with cerebral palsy. J Child Orthop 13(2):190–195
Dhawale AA, Shah SA, Sponseller PD, Bastrom T, Neiss G, Yorgova P et al (2012) Are antifibrinolytics helpful in decreasing blood loss and transfusions during spinal fusion surgery in children with cerebral palsy scoliosis? Spine (Phila Pa 1976) 37(9):E549–E555
Davies P, Robertson S, Hegde S, Greenwood R, Massey E, Davis P (2007) Calculating the required transfusion volume in children. Transfusion 47(2):212–216
Batıbay S (2018) Is tranexamic acid safe and reliable after tibia intramedullary nailing? Turk J Trauma Emerg Surg 24:575
Iseki T, Tsukada S, Wakui M, Yoshiya S (2018) Intravenous tranexamic acid only versus combined intravenous and intra-articular tranexamic acid for perioperative blood loss in patients undergoing total knee arthroplasty. Eur J Orthop Surg Traumatol 28(7):1397–1402
Tzatzairis T, Drosos GI, Vogiatzaki T, Tilkeridis K, Ververidis A, Kazakos K (2019) Multiple intravenous tranexamic acid doses in total knee arthroplasty without tourniquet: a randomized controlled study. Arch Orthop Trauma Surg 139(6):859–868
Halanski MA, Cassidy JA, Hetzel S, Reischmann D, Hassan N (2014) The efficacy of amicar versus tranexamic acid in pediatric spinal deformity surgery: a prospective, randomized, double-blinded pilot study. Spine Deform 2(3):191–197
McNicol ED, Tzortzopoulou A, Schumann R, Carr DB, Kalra A (2016) Antifibrinolytic agents for reducing blood loss in scoliosis surgery in children. Cochrane Database Syst Rev 9:CD006883
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tzatzairis, T., McMahon, S., Shilpa, J. et al. Safety and efficacy of tranexamic acid in children with cerebral palsy undergoing femoral varus derotational osteotomy: a double cohort study. Eur J Orthop Surg Traumatol 30, 1039–1044 (2020). https://doi.org/10.1007/s00590-020-02663-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-020-02663-w