Abstract
Background
Tranexamic acid (TXA) is an anti-fibrinolytic effective in reducing blood loss in orthopedic surgery. The appropriate dosing protocol for adult spinal deformity (ASD) surgery is not known. The purpose of this study was to evaluate two TXA protocols [low dose (L): 10 mg/kg bolus, 1 mg/kg/hr infusion; high dose (H): 50 mg/kg, 5 mg/kg/hr] in complex ASD surgery.
Methods
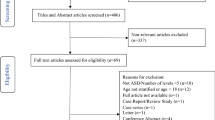
Inclusion criteria were ASD reconstructions with minimum 10 fusion levels or planned 3-column osteotomy (3CO). Standard demographic and surgical data were collected. Intraoperative estimated blood loss (EBL) was calculated by suction canisters minus irrigation plus estimated blood lost in sponges, estimated to the nearest 50 mL. Serious adverse events (SAE) were defined a priori as: venothromboembolic event (VTE), cardiac arrhythmia, myocardial infarction, renal dysfunction, and seizure. All SAE were recorded. Simple t tests compared EBL between groups. Mean EBL by total blood volume (TBV), transfusion volume, complications related to TXA were secondary outcomes.
Results
Sixty-two patients were enrolled and 52 patients completed the study; 25 were randomized to H and 27 to L. Demographic and surgical variables were not different between the two groups. EBL was not different between groups (H: 1596 ± 933 cc, L: 2046 ± 1105 cc, p = 0.12, 95% CI: − 1022 to 122 cc). EBL as a percentage of TBV was lower for the high-dose group (H: 29.5 ± 14.8%, L: 42.5 ± 26.2%, p = 0.03). Intraoperative transfusion volume (H: 961 ± 505 cc, L: 1105 ± 808 cc, p = 0.5) and post-operative transfusion volume (H: 513 ± 305 cc, L: 524 ± 245 cc, p = 0.9) were not different. SAE related to TXA were not different (p = 0.7) and occurred in 2 (8%) H and 3 (11%) L. There was one seizure (H), 2 VTE, and 2 arrhythmias.
Conclusion
No differences in EBL, transfusion volume, nor SAE were observed between H and L dose TXA protocols. High dose was associated with decreased TBV loss (13%). Further prospective study, with pharmacologic analysis, is required to determine appropriate TXA dosage in ASD surgeries.
Level of evidence
Therapeutic Level II.
Trial registration
The study was registered at Clinicaltrials.gov (NCT02053363) February 3, 2014.

Similar content being viewed by others
Availability of data
Data are not available for sharing.
References
Elgafy H, Bransford RJ, McGuire RA et al (2010) Blood loss in major spine surgery: are there effective measures to decrease massive hemorrhage in major spine fusion surgery? Spine 35:S47-56. https://doi.org/10.1097/BRS.0b013e3181d833f6
Raad M, Amin R, Jain A et al (2019) Multilevel arthrodesis for adult spinal deformity: when should we anticipate major blood loss? Spine Deform 7:141–145. https://doi.org/10.1016/j.jspd.2018.06.012
Baird EO, McAnany SJ, Lu Y et al (2015) Hemostatic agents in spine surgery: a critical analysis review. JBJS Rev. https://doi.org/10.2106/JBJS.RVW.N.00027
Berenholtz SM, Pham JC, Garrett-Mayer E et al (2009) Effect of epsilon aminocaproic acid on red-cell transfusion requirements in major spinal surgery. Spine 34:2096–2103. https://doi.org/10.1097/BRS.0b013e3181b1fab2
Elwatidy S, Jamjoom Z, Elgamal E et al (2008) Efficacy and safety of prophylactic large dose of tranexamic acid in spine surgery: a prospective, randomized, double-blind, placebo-controlled study. Spine 33:2577–2580. https://doi.org/10.1097/BRS.0b013e318188b9c5
Gill JB, Chin Y, Levin A et al (2008) The use of antifibrinolytic agents in spine surgery. A meta-analysis. J bone Joint Surg Am 90:2399–2407. https://doi.org/10.2106/JBJS.G.01179
Neilipovitz DT (2004) Tranexamic acid for major spinal surgery. Eur Spine J 13(Suppl 1):S62-65. https://doi.org/10.1007/s00586-004-0716-2
Okubadejo GO, Bridwell KH, Lenke LG et al (2007) Aprotinin may decrease blood loss in complex adult spinal deformity surgery, but it may also increase the risk of acute renal failure. Spine 32:2265–2271. https://doi.org/10.1097/BRS.0b013e31814ce9b0
Neilipovitz DT, Murto K, Hall L et al (2001) A randomized trial of tranexamic acid to reduce blood transfusion for scoliosis surgery. Anesth Analg 93:82–87
Sethna NF, Zurakowski D, Brustowicz RM et al (2005) Tranexamic acid reduces intraoperative blood loss in pediatric patients undergoing scoliosis surgery. Anesthesiology 102:727–732
Shapiro F, Zurakowski D, Sethna NF (2007) Tranexamic acid diminishes intraoperative blood loss and transfusion in spinal fusions for duchenne muscular dystrophy scoliosis. Spine 32:2278–2283. https://doi.org/10.1097/BRS.0b013e31814cf139
(2008) Cyklokapron (tranexamic acid tablets and tranexamic acid injection). http://media.pfizer.com/products/rx/rx_product_cyklokapron.jsp. Accessed 13 Feb 2020
Verma K, Errico T, Diefenbach C et al (2014) The relative efficacy of antifibrinolytics in adolescent idiopathic scoliosis: a prospective randomized trial. J Bone Joint Surg Am 96:e80. https://doi.org/10.2106/JBJS.L.00008
Xu C, Wu A, Yue Y (2012) Which is more effective in adolescent idiopathic scoliosis surgery: batroxobin, tranexamic acid or a combination? Arch Orthop Trauma Surg 132:25–31. https://doi.org/10.1007/s00402-011-1390-6
Cheriyan T, Maier SP 2nd, Bianco K et al (2015) Efficacy of tranexamic acid on surgical bleeding in spine surgery: a meta-analysis. Spine J 15:752–761. https://doi.org/10.1016/j.spinee.2015.01.013
Raman T, Varlotta C, Vasquez-Montes D et al (2019) The use of tranexamic acid in adult spinal deformity: is there an optimal dosing strategy? Spine J 19:1690–1697. https://doi.org/10.1016/j.spinee.2019.06.012
Goobie SM, Meier PM, Pereira LM et al (2011) Efficacy of tranexamic acid in pediatric craniosynostosis surgery: a double-blind, placebo-controlled trial. Anesthesiology 114:862–871. https://doi.org/10.1097/ALN.0b013e318210fd8f
Butterworth JF, Mackey DC, Wasnick JD (2020) Morgan and Mikhail’s clinical anesthesiology cases. McGraw Hill Lange, New York
Nadler SB, Hidalgo JH, Bloch T (1962) Prediction of blood volume in normal human adults. Surgery 51:224–232
Glassman SD, Hamill CL, Bridwell KH et al (2007) The impact of perioperative complications on clinical outcome in adult deformity surgery. Spine 32:2764–2770. https://doi.org/10.1097/BRS.0b013e31815a7644
Colomina MJ, Koo M, Basora M et al (2017) Intraoperative tranexamic acid use in major spine surgery in adults: a multicentre, randomized, placebo-controlled trial. Br J Anaesth 118:380–390. https://doi.org/10.1093/bja/aew434
Farrokhi MR, Kazemi AP, Eftekharian HR et al (2011) Efficacy of prophylactic low dose of tranexamic acid in spinal fixation surgery: a randomized clinical trial. J Neurosurg Anesthesiol 23:290–296. https://doi.org/10.1097/ANA.0b013e31822914a1
Goobie SM, Zurakowski D, Glotzbecker MP et al (2018) Tranexamic acid is efficacious at decreasing the rate of blood loss in adolescent scoliosis surgery: a randomized placebo-controlled trial. J Bone Joint Surg Am 100:2024–2032. https://doi.org/10.2106/JBJS.18.00314
Peters A, Verma K, Slobodyanyuk K et al (2015) Antifibrinolytics reduce blood loss in adult spinal deformity surgery: a prospective, randomized controlled trial. Spine 40:E443-449. https://doi.org/10.1097/BRS.0000000000000799
Raksakietisak M, Sathitkarnmanee B, Srisaen P et al (2015) Two doses of tranexamic acid reduce blood transfusion in complex spine surgery: a prospective randomized study. Spine 40:E1257-1263. https://doi.org/10.1097/BRS.0000000000001063
Yagi M, Hasegawa J, Nagoshi N et al (2012) Does the intraoperative tranexamic acid decrease operative blood loss during posterior spinal fusion for treatment of adolescent idiopathic scoliosis? Spine 37:E1336-1342. https://doi.org/10.1097/BRS.0b013e318266b6e5
Colomina MJ, Koo M, Basora M et al (2017) Intraoperative tranexamic acid use in major spine surgery in adults: a multicentre, randomized, placebo-controlled trialdagger. Br J Anaesth 118:380–390. https://doi.org/10.1093/bja/aew434
Yuan QM, Zhao ZH, Xu BS (2017) Efficacy and safety of tranexamic acid in reducing blood loss in scoliosis surgery: a systematic review and meta-analysis. Eur Spine J 26:131–139. https://doi.org/10.1007/s00586-016-4899-0
Li ZJ, Fu X, Xing D et al (2013) Is tranexamic acid effective and safe in spinal surgery? A meta-analysis of randomized controlled trials. Eur Spine J 22:1950–1957. https://doi.org/10.1007/s00586-013-2774-9
Sharma V, Katznelson R, Jerath A et al (2014) The association between tranexamic acid and convulsive seizures after cardiac surgery: a multivariate analysis in 11 529 patients. Anaesthesia 69:124–130. https://doi.org/10.1111/anae.12516
Hui S, Xu D, Ren Z et al (2018) Can tranexamic acid conserve blood and save operative time in spinal surgeries? A meta-analysis. Spine J 18:1325–1337. https://doi.org/10.1016/j.spinee.2017.11.017
Goobie SM, Faraoni D (2019) Tranexamic acid and perioperative bleeding in children: what do we still need to know? Curr Opin Anaesthesiol 32:343–352. https://doi.org/10.1097/ACO.0000000000000728
Lin JD, Lenke LG, Shillingford JN et al (2018) Safety of a high-dose tranexamic acid protocol in complex adult spinal deformity: analysis of 100 consecutive cases. Spine Deform 6:189–194. https://doi.org/10.1016/j.jspd.2017.08.007
Xie J, Lenke LG, Li T et al (2015) Preliminary investigation of high-dose tranexamic acid for controlling intraoperative blood loss in patients undergoing spine correction surgery. Spine J 15:647–654. https://doi.org/10.1016/j.spinee.2014.11.023
Bai J, Zhang P, Liang Y et al (2019) Efficacy and safety of tranexamic acid usage in patients undergoing posterior lumbar fusion: a meta-analysis. BMC Musculoskelet Disord 20:390. https://doi.org/10.1186/s12891-019-2762-2
Lu VM, Ho YT, Nambiar M et al (2018) The perioperative efficacy and safety of antifibrinolytics in adult spinal fusion surgery: a systematic review and meta-analysis. Spine 43:E949–E958. https://doi.org/10.1097/BRS.0000000000002580
Luo W, Sun RX, Jiang H et al (2018) The efficacy and safety of topical administration of tranexamic acid in spine surgery: a meta-analysis. J Orthop Surg Res 13:96. https://doi.org/10.1186/s13018-018-0815-0
Yerneni K, Burke JF, Tuchman A et al (2019) Topical tranexamic acid in spinal surgery: a systematic review and meta-analysis. J Clin Neurosci 61:114–119. https://doi.org/10.1016/j.jocn.2018.10.121
Zhang F, Wang K, Li FN et al (2014) Effectiveness of tranexamic acid in reducing blood loss in spinal surgery: a meta-analysis. BMC Musculoskelet Disord 15:448. https://doi.org/10.1186/1471-2474-15-448
Yang B, Li H, Wang D et al (2013) Systematic review and meta-analysis of perioperative intravenous tranexamic acid use in spinal surgery. PLoS ONE 8:e55436. https://doi.org/10.1371/journal.pone.0055436
Kalavrouziotis D, Voisine P, Mohammadi S et al (2012) High-dose tranexamic acid is an independent predictor of early seizure after cardiopulmonary bypass. Ann Thorac Surg 93:148–154. https://doi.org/10.1016/j.athoracsur.2011.07.085
Manji RA, Grocott HP, Leake J et al (2012) Seizures following cardiac surgery: the impact of tranexamic acid and other risk factors. Can J Anaesth 59:6–13. https://doi.org/10.1007/s12630-011-9618-z
Montes FR, Pardo DF, Carreno M et al (2012) Risk factors associated with postoperative seizures in patients undergoing cardiac surgery who received tranexamic acid: a case-control study. Ann Card Anaesth 15:6–12. https://doi.org/10.4103/0971-9784.91467
Murkin JM, Falter F, Granton J et al (2010) High-dose tranexamic Acid is associated with nonischemic clinical seizures in cardiac surgical patients. Anesth Analg 110:350–353. https://doi.org/10.1213/ANE.0b013e3181c92b23
Levine M, Ensom MH (2001) Post hoc power analysis: an idea whose time has passed? Pharmacotherapy 21:405–409. https://doi.org/10.1592/phco.21.5.405.34503
Funding
Direct support was received from AO Spine North America.
Author information
Authors and Affiliations
Contributions
JCC: analyzed data, drafted initial manuscript, approved final manuscript, interpretation; MHD, RCW, EF: assisted with data collection, data analysis and interpretation, approved final manuscript; LGL: design, acquisition of data, conceived initial study, assisted with data collection, approved final manuscript; MPK: conceived initial study, collected and analyzed data, critically revised manuscript, approved final manuscript, drafting, interpretation.
Corresponding author
Ethics declarations
Conflict of interest
Drs. Clohisy, El Dafrawy, Frazier, and Ms. Wolfe report no conflicts of interest. Dr. Kelly reports research funding support to his institution paid by the Setting Scoliosis Straight Foundation. Dr. Lenke reports being a consultant for Medtronic (money donated to charity); receiving royalties from Medtronic and Quality Medical Publishing; receiving reimbursement for airfare and hotels from Broadwater, the Seattle Science Foundation, Stryker Spine, the Spinal Research Foundation, AOSpine, and the Scoliosis Research Society; receiving grant support from the Scoliosis Research Society (money to his institution), EOS Imaging (money to his institution), the Setting Scoliosis Straight Foundation (money to his institution); and receiving grant and fellowship support from AOSpine (money to his institution).
Ethical standards
Washington University IRB # 201312010.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Clohisy, J.C.F., Lenke, L.G., Dafrawy, M.H.E. et al. Randomized, controlled trial of two tranexamic acid dosing protocols in adult spinal deformity surgery. Spine Deform 10, 1399–1406 (2022). https://doi.org/10.1007/s43390-022-00539-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-022-00539-z