Abstract
Introduction
Reverse shoulder arthroplasty (RSA) is a common treatment for proximal humeral fractures (PHFs) in the elderly. This study evaluates the influence of tuberosity healing (TH) on functional outcome following a 135° humeral inclination RSA for PHFs.
Methods
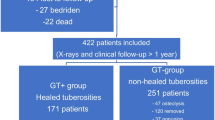
Retrospectively, all patients with an acute PHF treated with a 135° humeral inclination RSA at four centers during a three-year period were followed up. Constant score (CS), TH and glenoid notching were analyzed.
Results
Sixty-four of 100 patients (64%) with a mean age of 76 ± 7 years were available for follow-up at 22 ± 8 months. The mean-adjusted CS was 72%. TH of the greater tuberosity (GT) was 77% and resulted in significantly improved forward flexion (128° vs. 92°; p = 0.003), external rotation (33° vs. 17°; p = 0.03) and adjusted CS (78% vs. 54%, p < 0.005). GT healing rate was 86% with neutral, 70% with lateralized and 33% with an inferior eccentric glenosphere. TH of the lesser tuberosity was 79%. There was 8% complication and 3% revision rate; implant survival was 100%.
Conclusion
RSA with 135° humeral inclination for PHFs leads to good functional outcome, reproducible results and a high rate of TH. The short-term revision rate is low. TH is associated with improved ROM and functional outcome.
Level of evidence
III.



Similar content being viewed by others
References
Murray IR, Amin AK, White TO, Robinson CM (2011) Proximal humeral fractures: current concepts in classification, treatment and outcomes. J Bone Jt Surg Br 93:1–11. https://doi.org/10.1302/0301-620X.93B1.25702
Ockert B (2019) Die komplexe proximale Humerusfraktur. Obere Extremität 14:83–92. https://doi.org/10.1007/s11678-019-0510-8
Bastian JD, Hertel R (2009) Osteosynthesis and hemiarthroplasty of fractures of the proximal humerus: outcomes in a consecutive case series. J Shoulder Elb Surg 18:216–219. https://doi.org/10.1016/j.jse.2008.09.015
Krause FG, Huebschle L, Hertel R (2007) Reattachment of the tuberosities with cable wires and bone graft in hemiarthroplasties done for proximal humeral fractures with cable wire and bone graft: 58 patients with a 22-month minimum follow-up. J Orthop Trauma 21:682–686. https://doi.org/10.1097/BOT.0b013e31815917e0
Reineck JR, Krishnan SG, Burkhead WZ (2007) Four-part proximal humerus fractures: evaluation and treatment. Hand Clin 23:415–424. https://doi.org/10.1016/j.hcl.2007.09.006
Kettler M, Biberthaler P, Braunstein V et al (2006) Treatment of proximal humeral fractures with the PHILOS angular stable plate. Presentation of 225 cases of dislocated fractures. Unfallchirurg 109:1032–1040
Warnhoff M, Lill H, Jensen G et al (2019) Proximale Humerusfraktur – was sagt die aktuelle Literatur? Obere Extremität 14:9–17. https://doi.org/10.1007/s11678-018-0496-7
Cuff DJ, Pupello DR (2013) Comparison of hemiarthroplasty and reverse shoulder arthroplasty for the treatment of proximal humeral fractures in elderly patients. J Bone Jt Surg 95:2050–2055. https://doi.org/10.2106/JBJS.L.01637
Gallinet D, Clappaz P, Garbuio P et al (2009) Three or four parts complex proximal humerus fractures: hemiarthroplasty versus reverse prosthesis: a comparative study of 40 cases. Orthop Traumatol Surg Res 95:48–55. https://doi.org/10.1016/j.otsr.2008.09.002
Sebastiá-Forcada E, Cebrián-Gómez R, Lizaur-Utrilla A, Gil-Guillén V (2014) Reverse shoulder arthroplasty versus hemiarthroplasty for acute proximal humeral fractures: a blinded, randomized, controlled, prospective study. J Shoulder Elb Surg 23:1419–1426. https://doi.org/10.1016/j.jse.2014.06.035
Lévigne C, Boileau P, Favard L et al (2008) Scapular notching in reverse shoulder arthroplasty. J Shoulder Elb Surg 17:925–935. https://doi.org/10.1016/j.jse.2008.02.010
Worland RL, Kim DY, Arredondo J (1999) Periprosthetic humeral fractures: management and classification. J Shoulder Elb Surg 8:590–594
Crosby LA, Hamilton A, Twiss T (2011) Scapula fractures after reverse total shoulder arthroplasty: classification and treatment. Clin Orthop Relat Res 469:2544–2549. https://doi.org/10.1007/s11999-011-1881-3
Demirhan M, Kilicoglu O, Altinel L et al (2003) Prognostic factors in prosthetic replacement for acute proximal humerus fractures. J Orthop Trauma 17:181–189
Boileau P, Krishnan SG, Tinsi L et al (2002) Tuberosity malposition and migration: reasons for poor outcomes after hemiarthroplasty for displaced fractures of the proximal humerus. J Shoulder Elb Surg 11:401–412
Neer CS 2nd (1955) Indications for replacement of the proximal humeral articulation. Am J Surg 89:901–907
Greiner SH, Diederichs G, Kröning I et al (2009) Tuberosity position correlates with fatty infiltration of the rotator cuff after hemiarthroplasty for proximal humeral fractures. J Shoulder Elb Surg 18:431–436. https://doi.org/10.1016/j.jse.2008.10.007
Torrens C, Alentorn-Geli E, Mingo F et al (2018) Reverse shoulder arthroplasty for the treatment of acute complex proximal humeral fractures: influence of greater tuberosity healing on the functional outcomes. J Orthop Surg 26:230949901876013. https://doi.org/10.1177/2309499018760132
Chun YM, Kim DS, Lee DH, Shin SJ (2017) Reverse shoulder arthroplasty for four-part proximal humerus fracture in elderly patients: Can a healed tuberosity improve the functional outcomes? J Shoulder Elb Surg 26:1216–1221. https://doi.org/10.1016/j.jse.2016.11.034
Gallinet D, Adam A, Gasse N et al (2013) Improvement in shoulder rotation in complex shoulder fractures treated by reverse shoulder arthroplasty. J Shoulder Elb Surg 22:38–44. https://doi.org/10.1016/j.jse.2012.03.011
Ohl X, Bonnevialle N, Gallinet D et al (2018) How the greater tuberosity affects clinical outcomes after reverse shoulder arthroplasty for proximal humeral fractures. J Shoulder Elb Surg 27:2139–2144. https://doi.org/10.1016/j.jse.2018.05.030
Schmalzl J, Jessen M, Sadler N, Lehmann LJ, Gerhardt C (2020) High tuberosity healing rate associated with better functional outcome following primary reverse shoulder arthroplasty for proximal humeral fractures with a 135° prosthesis. BMC Musculoskelet Disord. 21(1):35
Funding
This work was supported by Arthrex. Drs. Lehmann, Cohen, Steinbeck and Denard are consultants for Arthrex, Inc.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Schmalzl, J., Jessen, M., Holschen, M. et al. Tuberosity healing improves functional outcome following primary reverse shoulder arthroplasty for proximal humeral fractures with a 135° prosthesis. Eur J Orthop Surg Traumatol 30, 909–916 (2020). https://doi.org/10.1007/s00590-020-02649-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-020-02649-8