Abstract
Introduction
Revision total knee arthroplasty (TKA) procedures performed secondary to periprosthetic joint infection (PJI) are associated with significant morbidity and mortality. These poor outcomes may be further complicated by postoperative infection requiring antibiotics. However, antibiotic overuse may suppress patients’ bacterial flora, leading to Clostridium difficile infection (CDI). Therefore, we aimed to study the: (1) incidence; (2) costs; and (3) risk factors associated with CDI in revision TKA patients.
Methods
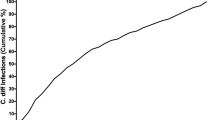
The National Inpatient Sample database was queried for individuals diagnosed with PJI who underwent revision TKA between 2009 and 2013 (n = 83,806). Patients who developed CDI during their inpatient stay were identified (n = 799). Logistic regression analysis was conducted to assess the association between hospital- and patient-specific characteristics and the development of CDI.
Results
The incidence of CDI after revision TKA was 1.0%. These patients were older (mean age 69.05 vs. 65.52 years), had greater LOS (median 11 vs. 5 days) and greater costs ($30,612.93 vs. 18,873.75), and experienced higher in-hospital mortality (3.6 vs. 0.5%; p < 0.001 for all) compared to those without infection. Patients with CDI were more likely to be treated in urban, not-for-profit, medium/large hospitals in the Northeast or Midwest (p < 0.05 for all) and to have underlying depression (OR 4.267; p = 0.007) or fluid/electrolyte disorders (OR 3.48; p = 0.001).
Conclusion
Although CDI is rare following revision TKA, it can have detrimental consequences. We demonstrate that CDI is associated with longer LOS, higher costs, and greater in-hospital mortality. With increased legislative pressure to lower healthcare expenditures, it is crucial to identify means of preventing costly complications.


Similar content being viewed by others
References
Delanois RE, Mistry JB, Gwam CU et al (2017) Current epidemiology of revision total knee arthroplasty in the United States. J Arthroplasty. https://doi.org/10.1016/j.arth.2017.03.066
Bozic KJ, Kurtz SM, Lau E et al (2010) The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop Relat Res 468:45–51. https://doi.org/10.1007/s11999-009-0945-0
Kurtz S, Mowat F, Ong K et al (2005) Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am 87:1487–1497. https://doi.org/10.2106/JBJS.D.02441
Kurtz S, Ong K, Lau E et al (2007) Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 89:780–785. https://doi.org/10.2106/JBJS.F.00222
Kurtz SM, Lau E, Watson H et al (2012) Economic burden of periprosthetic joint infection in the United States. J Arthroplasty 27:61.e1–65.e1. https://doi.org/10.1016/j.arth.2012.02.022
Tande AJ, Patel R (2014) Prosthetic joint infection. Clin Microbiol Rev 27:302–345. https://doi.org/10.1128/CMR.00111-13
Alexander PharmD BT, Babic M, Brause BD et al (2014) Antibiotic treatment and timing of reimplantation. J Orthop Res 32:136–140. https://doi.org/10.1002/jor.22557
Chaussade H, Uçkay I, Vuagnat A et al (2017) Antibiotic therapy duration for prosthetic joint infections treated by Debridement and Implant Retention (DAIR): similar long-term remission for 6 weeks as compared to 12 weeks. Int J Infect Dis. https://doi.org/10.1016/j.ijid.2017.08.002
Mazzucchelli L, Rosso F, Marmotti A et al (2015) The use of spacers (static and mobile) in infection knee arthroplasty. Curr Rev Musculoskelet Med 8:373–382. https://doi.org/10.1007/s12178-015-9293-8
O’Connor JR, Johnson S, Gerding DN (2009) Clostridium difficile infection caused by the epidemic BI/NAP1/027 strain. Gastroenterology 136:1913–1924. https://doi.org/10.1053/j.gastro.2009.02.073
BI/NAP1/027: Putting a strain on healthcare-associated infections
Ghose C (2013) Clostridium difficile infection in the twenty-first century. Emerg Microbes Infect 2:e62. https://doi.org/10.1038/emi.2013.62
Abdelsattar ZM, Krapohl G, Alrahmani L et al (2015) Postoperative burden of hospital-acquired Clostridium difficile infection. Infect Control Hosp Epidemiol 36:40–46. https://doi.org/10.1017/ice.2014.8
NIS database documentation
Benjamini Y, Hochberg Y (1995) Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Ser B 57:289–300
Hegazy MAM, Fayez YM (2015) Mean centering of ratio spectra and concentration augmented classical least squares in a comparative approach for quantitation of spectrally overlapped bands of antihypertensives in formulations. Spectrochim Acta Part A Mol Biomol Spectrosc 140:210–215. https://doi.org/10.1016/j.saa.2014.12.103
Iacobucci D, Schneider MJ, Popovich DL, Bakamitsos GA (2016) Mean centering helps alleviate “micro” but not “macro” multicollinearity. Behav Res Methods 48:1308–1317. https://doi.org/10.3758/s13428-015-0624-x
Causation and Observational Studies » Biostatistics » College of Public Health and Health Professions » University of Florida
Maltenfort MG, Rasouli MR, Morrison TA, Parvizi J (2013) Clostridium difficile colitis in patients undergoing lower-extremity arthroplasty: rare infection with major impact. Clin Orthop Relat Res 471:3178–3185. https://doi.org/10.1007/s11999-013-2906-x
Kurd MF, Pulido L, Joshi A et al (2008) Clostridium difficile infection after total joint arthroplasty: who is at risk? J Arthroplasty 23:839–842. https://doi.org/10.1016/j.arth.2007.10.033
Aggarwal VK, Rasouli MR, Parvizi J (2013) Periprosthetic joint infection: current concept. Indian J Orthop 47:10–17. https://doi.org/10.4103/0019-5413.106884
Stevens V, Dumyati G, Fine LS et al (2011) Cumulative antibiotic exposures over time and the risk of Clostridium difficile infection. Clin Infect Dis 53:42–48. https://doi.org/10.1093/cid/cir301
Miller AC, Polgreen LA, Cavanaugh JE, Polgreen PM (2016) Hospital Clostridium difficile infection rates and prediction of length of stay in patients without C. difficile infection. Infect Control Hosp Epidemiol 37:404–410. https://doi.org/10.1017/ice.2015.340
Song X, Bartlett JG, Speck K et al (2008) Rising economic impact of Clostridium difficile-associated disease in adult hospitalized patient population. Infect Control Hosp Epidemiol 29:823–828. https://doi.org/10.1086/588756
Rogers MAM, Greene MT, Young VB et al (2013) Depression, antidepressant medications, and risk of Clostridium difficile infection. BMC Med 11:121. https://doi.org/10.1186/1741-7015-11-121
Frank JM, Kayupov E, Moric M et al (2017) The mark coventry, MD, award: oral antibiotics reduce reinfection after two-stage exchange: a multicenter, randomized controlled trial. Clin Orthop Relat Res 475:56–61. https://doi.org/10.1007/s11999-016-4890-4
Lipp MJ, Nero DC, Callahan MA (2012) Impact of hospital-acquired Clostridium difficile. J Gastroenterol Hepatol 27:1733–1737. https://doi.org/10.1111/j.1440-1746.2012.07242.x
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Gwam, C.U., George, N.E., Etcheson, J.I. et al. Clostridium difficile infection in the USA: incidence and associated factors in revision total knee arthroplasty patients. Eur J Orthop Surg Traumatol 29, 667–674 (2019). https://doi.org/10.1007/s00590-018-2319-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-018-2319-3