Abstract
Purpose
The purpose of this cross-sectional, observational study was to establish the relationship between standing lumbar lordosis (LL) and lateral decubitus LL.
Methods
Forty-nine subjects, 24 male and 25 female, were prospectively enrolled. Patients with pre-existing spinopelvic pathology were excluded. Standing, relaxed-seated, and lateral decubitus lateral radiographs were obtained. Radiographic variables measured included LL and lordosis change at each lumbar level (e.g. L1-L2). The change in LL when going from a standing to a lateral decubitus position (ΔLL), the correlation between standing and sitting LL compared to lateral decubitus LL, and the correlation between ΔLL and standing pelvic incidence (PI), pelvic tilt (PT), PI-LL mismatch, pelvic femoral angle (PFA), and sacral slope (SS) were calculated.
Results
Subjects had an average age of 25.7 ± 2.3 years and body mass index of 24.1 ± 3.0 kg/m2. On average, 11.9°±8.2° (range − 7° to 29°) of LL was lost when transitioning from a standing to the lateral decubitus position. Lateral decubitus LL had a higher correlation with standing LL (R = 0.725, p < 0.001) than with relaxed-seated LL (R = 0.434, p < 0.001). Standing PT and PI-LL mismatch had moderately negative correlations with ΔLL (R=-0.58 and R=-0.59, respectively, both p < 0.05). Standing PI and standing PFA had a low negative correlation with ΔLL (R=-0.31 and R=-0.44, respectively, both p < 0.05) Standing SS and LL had no correlation with ΔLL.
Conclusions
Standing LL was strongly correlated to lateral decubitus LL, although subjects lost an average of 11.9° from the standing to the lateral decubitus position. This has important implications for fusion in the lateral position.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lateral lumbar interbody fusion (LLIF) has been increasing in popularity since the original description of the minimally invasive technique by Ozgur et al. in 2006 [1]. Due to the large surface area that lateral interbody fusion provides, it is thought that this may increase fusion rates compared to posterior techniques, such as posterior or transforaminal lumbar interbody fusion (PLIF or TLIF) [2]. Additionally, the lateral approach has the potential to have less morbidity as compared to an open anterior approach [3]. While there is potential to injure the psoas and lumbar plexus during the lateral approach [4,5,6,7,8], recent advances in intraoperative electromyography monitoring have decreased the risk of such complications [9].
Furthermore, increased attention has been placed on restoring sagittal alignment in recent years. In the adult spinal deformity population, Schwab et al. recognized the importance of sagittal alignment and restoring specific radiographic parameters such as pelvic tilt (PT) and sagittal vertical axis (SVA) [10]. These principles have been recognized to be important in lumbar degenerative disease as well, with some suggesting that segmental lumbar lordosis (LL) be carefully calculated even in short segment lumbar fusion to prevent adjacent segment disease [11].
It therefore follows that sagittal alignment should be considered in LLIF. To date, several studies have shown that LL increases in the prone position compared to the standing position [12,13,14]. Additionally, segmental LL has been compared between prone and lateral positions, with several studies finding increased segmental lordosis in the prone position compared to the lateral decubitus position [15, 16]. To date, however, there have been no studies comparing standing LL to lateral LL. Therefore, the purpose of this study was to establish the correlation between standing LL and LL in the lateral decubitus position amongst healthy volunteers.
Methods
Data collection
Forty-nine subjects, 24 male and 25 female, were prospectively recruited to participate in this study. Inclusion criteria included age between 18- and 35-years. Exclusion criteria included back or hip pain, inability to stand upright or sit with hips flexed to 90°, a history of ankylosing spondylitis, femoroacetabular impingement, and prior hip or spine surgery. The present study was conducted as approved by the Institutional Review Board (IRB HS-22-00214).
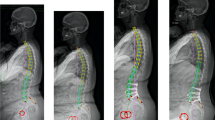
Three lateral radiographs were obtained for each subject: standing, relaxed-seated, and lateral decubitus. (Fig. 1) For the standing lateral radiograph, subjects were instructed to stand straight up and rested their arms on a bar in front of them with approximately 90° of shoulder flexion. For the relaxed-seated radiograph, subjects were instructed to sit down in a comfortable position with their hips and knees flexed to 90° with their hands resting on their knees. For the lateral decubitus radiograph, subjects were positioned in a lateral decubitus position on a table in the x-ray suite. To simulate intraoperative positioning, one pillow was placed under the head, two pillows were placed between the arms, and two pillows were placed between the legs. The arms and legs were positioned by a senior orthopaedic surgery resident (E.S.M.) and research staff to best approximate intraoperative positioning.
Radiographic variables measured included LL, segmental lordosis at each lumbar level (L1-L2, L2-L3, L3-L4, L4-L5, L5-S1), pelvic incidence (PI), pelvic tilt (PT), and pelvic femoral angle (PFA) (Fig. 2) PFA is an established measure of hip flexion in the arthroplasty literature [17]. PI-LL mismatch was calculated as the difference between PI and LL. The lordosis change at each lumbar segment was calculated as the change in angle in the segment between a standing position and the lateral decubitus position. Each segment’s contribution to overall LL was calculated as the ratio of the individual segment divided by the overall LL.
Radiographic measurements including (A) lumbar lordosis (angle between the superior endplate of L1 and then superior endplate of S1); (B) segmental lumbar lordosis (angle between inferior and superior endplate of each respective lumbar level); (C) pelvic incidence (the anterior-posterior dimension of the pelvis measured by the relationship between the femoral heads and the sacrum); (D) pelvic tilt (the difference between the pelvic incidence and the sacral slope); and (E) pelvic femoral angle (the angle of the femur relative to the sacrum)
Statistical analysis
Descriptive statistics are reported as mean ± standard deviation. Pearson correlations were calculated to determine the correlation between various parameters. The correlations between standing LL and sitting LL compared to lateral LL were calculated. The correlations between standing PI, PT, PI-LL mismatch, SS, and LL and the change in LL when going from standing to lateral decubitus (ΔLL) were calculated to determine if there are any standing radiographic factors that correlated with an increased ΔLL. Finally, the correlation between PFA and LL in the lateral position was calculated. All statistics were completed using SPSS version 26 (IBM, Armonk, NY, USA). A p-value of < 0.05 was considered statistically significant.
Results
The cohort had an average age of 25.7 ± 2.3 years and body mass index (BMI) of 24.1 ± 3.0 kg/m2. While standing, subjects had an average LL of 53.3°±10.7°. When in the relaxed-seated position, subjects had an average LL of 24.6°±12.1°. When in the lateral decubitus position, subjects had an average LL of 42.3°±11.1°.
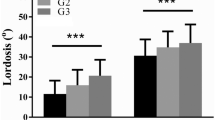
On average, 11.9°±8.2° (22.2%, range − 7° to 28°) of LL was lost when transitioning from the standing to the lateral decubitus position. Forty-five (91.8%) subjects lost lordosis, three (6.1%) gained lordosis, and one (2.0%) had no change when going from standing to the lateral decubitus position (Fig. 3)
Standing PT and PI-LL mismatch had moderately negative correlations with ΔLL (R=-0.58 and R=-0.59, respectively, both p < 0.05). Standing PI and standing PFA had a low negative correlation with ΔLL (R=-0.31 and R=-0.44, respectively, both p < 0.05) (Fig. 4). Standing SS and LL had no correlation with ΔLL. Regarding demographics, age and BMI were not correlated with ΔLL and there was no significant difference in ΔLL between gender.
Lateral decubitus LL had a higher correlation with standing LL (R = 0.725, p < 0.001) than with relaxed-seated LL (R = 0.434, p < 0.001). (Fig. 5). The segment with the maximal change in lordosis when transitioning from a standing to the lateral decubitus position was most often at the segment where maximal lordosis occurred when standing (25/49, 51.0%), although there was significant variability. The segment of maximal change was most commonly L4-L5 (11/49, 22.4%) (Fig. 6).
Seventeen subjects were excluded from the hip flexion angle analysis due to poor radiographic quality (i.e. proximal femurs were not visible in the radiograph). Therefore, 32 subjects were included. Hip flexion (PFA) in the lateral decubitus position was weakly correlated with ΔLL. Patients with a higher PFA, i.e. more hip extension, had less change in lordosis when going from the standing to the lateral decubitus position (R=-0.33, p < 0.05). Additionally, there was a moderately positive correlation between lateral LL and lateral PFA (R = 0.58, p < 0.05) (Fig. 7).
Discussion
In this prospective study of healthy individuals without hip- or spine-related pathology, subjects lost on average 11.9°±8.2°, or 22.2%, of LL when transitioning from a standing to lateral decubitus position. PT and PI-LL mismatch were moderately negatively correlated with ΔLL, indicating that lower PT and lower PI-LL mismatch when standing were associated with increased changes in LL when going from a standing to lateral decubitus position. The lateral position had a stronger correlation with standing LL than sitting lordosis. The lumbar segment with the most lordosis while standing most often corresponded with the segment of maximal change when transitioning from a standing to lateral position, although there was significant variability.
Previous studies have looked at positioning in the lateral versus prone position, with one meta-analysis finding no change in overall LL between the two groups, but an increase in segmental lordosis in the prone positioning group compared to the lateral positioning group [7]. Several studies have assessed the difference in LL between standing and prone positioning. Fei et al. studied intraoperative prone positioning and found no difference compared to preoperative standing radiographs in a population undergoing adult spinal deformity correction [12]. Yasuda et al. found that LL greatly increases in prone positioning compared to preoperative standing images [13]. Harimaya et al. studied 44 adult spinal deformity patients and found that patients with hypolordosis had an increase in lordosis during prone positioning, whereas patients with significant preoperative lordosis did not have a significant intraoperative change [14]. While these studies have done an excellent job at assessing the difference between LL in the standing and prone positions, this is the first study we are aware of to quantify the difference in LL when transitioning from a standing to lateral position.
Additionally, we found a weak correlation between hip flexion and the change in LL when going from a standing to lateral position. Subjects who had less hip flexion maintained more lordosis in the lateral position. While this was only found to have a weak correlation (R=-0.33), this indicates that hip extension while positioning patients in the lateral position may increase LL. Previous studies have found a relationship between motion through the lumbar spine, pelvis, and hip [18, 19]. Both the hip and spine contribute to flexion through the pelvis [20]; therefore, it is logical that decreased hip flexion leads to a compensatory increase in LL in the lateral position.
There are several limitations to our study. First, this was a young, healthy population without degenerative spinal disease. These findings therefore may not be generalizable to operative patients. Further research is needed to determine if our present findings remain true in patients with degenerative disease. Second, the lateral radiograph was taken on a table in the x-ray suite with the subjects awake, not in the operating room while under anesthesia. As such, it is possible we did not accurately capture intraoperative lateral LL. Third, we were only able to include 32 patients in our analysis correlating hip flexion with lateral LL due to poor radiographic quality that was unable to capture the upper lumbar segment and proximal femur in the same view. Future studies should attempt to validate our findings with a larger cohort of patients with degenerative disease.
Conclusion
Normal, healthy individuals lost on average 11.9°±8.2°, or 22.2%, of LL when transitioning from standing to lateral positioning. Lower PT and lower PI-LL mismatch when standing are associated with a lower ΔLL. The segment with maximal lordosis while standing was most often the segment that had the largest change in lordosis. These findings establish important normative values for LL in the lateral position as well as ΔLL when transitioning from a standing to lateral decubitus position and may assist surgeons in preoperative planning for lateral fusion surgery. Positioning the hip in extension may help minimize the decrease in lordosis observed amongst patients undergoing surgery in the lateral decubitus position.
References
Ozgur BM, Aryan HE, Pimenta L, Taylor WR (2006) Extreme lateral Interbody Fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. Spine J 6:435–443
Laws CJ, Coughlin DG, Lotz JC, Serhan HA, Hu SS (2012) Direct lateral approach to lumbar fusion is a biomechanically equivalent alternative to the anterior approach: an in vitro study. Spine 37:819–825
Kwon B, Kim DH (2016) Lateral lumbar Interbody Fusion: indications, outcomes, and complications. J Am Acad Orthop Surg 24:96–105
Davis TT, Bae HW, Mok JM, Rasouli A, Delamarter RB (2011) Lumbar plexus anatomy within the psoas muscle: implications for the transpsoas lateral approach to the L4-L5 disc. J Bone Joint Surg Am 93:1482–1487
Lykissas MG, Aichmair A, Hughes AP, Sama AA, Lebl DR, Taher F et al (2014) Nerve injury after lateral lumbar interbody fusion: a review of 919 treated levels with identification of risk factors. Spine J 14:749–758
Hijji FY, Narain AS, Bohl DD, Ahn J, Long WW, DiBattista JV et al (2017) Lateral lumbar interbody fusion: a systematic review of complication rates. Spine J 17:1412–1419
Mills ES, Treloar J, Idowu O, Shelby T, Alluri RK, Hah RJ (2021) Single position lumbar Fusion: a systematic review and Meta Analysis. Spine J. https://doi.org/10.1016/j.spinee.2021.10.012
Pumberger M, Hughes AP, Huang RR, Sama AA, Cammisa FP, Girardi FP (2012) Neurologic deficit following lateral lumbar interbody fusion. Eur Spine J 21:1192–1199
Uribe JS, Isaacs RE, Youssef JA, Khajavi K, Balzer JR, Kanter AS et al (2015) Can triggered electromyography monitoring throughout retraction predict postoperative symptomatic neuropraxia after XLIF? Results from a prospective multicenter trial. Eur Spine J 24(Suppl 3):378–385
Schwab F, Ungar B, Blondel B, Buchowski J, Coe J, Deinlein D et al (2012) Scoliosis Research Society-Schwab adult spinal deformity classification: a validation study. Spine 37:1077–1082
Zheng G, Wang C, Wang T, Hu W, Ji Q, Hu F et al (2020) Relationship between postoperative lordosis distribution index and adjacent segment disease following L4-S1 posterior lumbar interbody fusion. J Orthop Surg Res 15:129
Fei H, Li W-S, Sun Z-R, Jiang S, Chen Z-Q (2017) Effect of patient position on the lordosis and scoliosis of patients with degenerative lumbar scoliosis. Medicine 96:e7648
Yasuda T, Hasegawa T, Yamato Y, Togawa D, Kobayashi S, Yoshida G et al (2018) Effect of position on lumbar lordosis in patients with adult spinal deformity. J Neurosurg Spine 29:530–534
Harimaya K, Lenke LG, Mishiro T, Bridwell KH, Koester LA, Sides BA (2009) Increasing lumbar lordosis of adult spinal deformity patients via intraoperative prone positioning. Spine 34:2406–2412
Agarwal V, Wildstein M, Tillman JB, Pelkey WL, Alamin TF (2009) Lumbar intersegmental spacing and angulation in the modified lateral decubitus position versus variants of prone positioning. Spine J 9:580–584
Smith TG, Pollina J, Joseph SA Jr, Howell KM Effects of Surgical Positioning on L4-L5 accessibility and lumbar lordosis in lateral transpsoas lumbar Interbody Fusion: a comparison of Prone and lateral decubitus in asymptomatic adults. World Neurosurg 2021. https://doi.org/10.1016/j.wneu.2021.01.113
Heckmann ND, Lieberman JR (2021) Spinopelvic Biomechanics and total hip arthroplasty: a primer for clinical practice. J Am Acad Orthop Surg 29:e888–903
Mills ES, Wang JC, Sanchez J, Ton A, Alluri RK, Heckmann ND et al (2023) The correlation between pelvic motion and lumbar motion in patients presenting with a lumbar spinal Pathology: implications for assessing dislocation risk in total hip arthroplasty. Arthroplast Today 20:101105
Heckmann N, McKnight B, Stefl M, Trasolini NA, Ike H, Dorr LD (2018) Late dislocation following total hip arthroplasty: Spinopelvic Imbalance as a causative factor. J Bone Joint Surg Am 100:1845–1853
Stefl M, Lundergan W, Heckmann N, McKnight B, Ike H, Murgai R et al (2017) Spinopelvic mobility and acetabular component position for total hip arthroplasty. Bone Joint J 99–B:37–45
Funding
Open access funding provided by SCELC, Statewide California Electronic Library Consortium
Author information
Authors and Affiliations
Contributions
R.K.A. - Consulting Fees: EcentialRobotics, HIA Technologies; Stock or Stock Options: HIA Technologies; Speaking and/or Teaching Arrangements: Nuvasive; Research Support (not for this work): Alphatec Spine; Leadership or Fiduciary Role: Global Spine Journal, IJSS.R.J.H. – Consulting Fees: Nuvasive; Trips/Travel Fees: North American Spine Society; Research Support (not for this work): SI-Bone; Leadership or Fiduciary Role: Clinical Spine Surgery, Global Spine Journal, Lumbar Spine Research Society, North American Spine Society. N.D.H. - Royalties: Corin U.S.A.; Consulting Fees: MicroportOrthopaedics, Intellijoint Surgical, Zimmer, Corin U.S.A.; Leadership or Fiduciary Role: AAOS, AJRR, AAHKS; Stock or Stock Options: Intellijoint Surgical.
Corresponding author
Ethics declarations
Competing interests
E.S.M., J.C.W., M.K.R., B.C.C, L.W.M., and M.C.G. have no interests to disclose.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mills, E.S., Wang, J.C., Richardson, M.K. et al. The change in lumbar lordosis from the standing to the lateral position: implications for lateral interbody fusion. Eur Spine J (2024). https://doi.org/10.1007/s00586-024-08493-2
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00586-024-08493-2