Abstract
Purpose
The study aims to establish the diagnostic accuracy of community spine x-rays for brace candidates.
Methods
A review of adolescent idiopathic scoliosis patients seen for initial visit at a tertiary care pediatric hospital was conducted (n = 170). The index test was the pre-referral community spine x-ray interpreted by a community radiologist. Measures of diagnostic accuracy for the index test were determined against the reference standard if images were obtained within 90 days (n = 111). The reference standard was the 3-foot standing EOS spine x-ray evaluated by spine specialists. Diagnostic criterion for a brace candidate was dichotomized by Cobb angle range (25–40°) according to Scoliosis Research Society criteria. Risser stage was not included given significant missing data in index reports. To mitigate the uncertainty around true progression, sensitivity analyses were conducted on a sub-sample of data when index test was within 60 days of the reference standard (n = 67).
Results
Accuracy of the community spine x-ray to detect a brace candidate was 65.8% (95% CI 56.2–74.5). Sensitivity of the index test was 65.4% with a false negative rate of 34.6%. Specificity was 66.1% with a false positive rate of 33.9%. Positive and negative predictive values were 63.0% and 68.4%, respectively. Of the total number of brace candidates (n = 52), 32.7% were missed because of underestimation in Cobb angle (95% CI 21.5–46.2). The proportion of missed brace candidates because of underestimation was unchanged with 60-day data (p = 0.37).
Conclusions
Inaccuracies in community spine radiology may lead to missed opportunities for non-operative treatment.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Introduction
Adolescent idiopathic scoliosis (AIS) is the most prevalent pediatric spine condition affecting 1–3% of youth [1]. Growth presents the highest risk of curve progression leading to increased lateral deformity and vertebral rotation [1, 2]. This progressive spine deformity can affect respiratory capacity and produce significant concerns regarding trunk shape, with subsequent physical and psychosocial distress in youth [3, 4]. Therefore, in severe cases, the deformity is stabilized by spine surgery through posterior spinal instrumented fusion (PSIF) with risks of infection, hardware failure, neurologic injury, and revision surgery [5].
Early diagnosis of AIS allows for effective management through brace treatment, significantly decreasing the risk for surgery. Bracing decreases curve progression to surgical range by 72%, according to a randomized control trial [6]. Brace treatment, however, is time-limited, reserved only for children who are skeletally immature with moderate-sized curves [7]. Concerningly, in the absence of universal screening programs or well-defined and implemented wellness visits, AIS is commonly missed during periods of rapid growth since AIS patients are unlikely to present symptomatically to their primary care physician (PCP) [8]. This has led to an epidemic of AIS patients presenting with large deformities on initial consultation with a spine specialist. Approximately one third of patients are late referrals with curves at high risk of surgical intervention and less than 20% are ideal brace candidates at initial presentation [9, 10]. This referral pattern substantially increases the number of avoidable spine surgeries, places enormous burden on a publicly funded health care system, and leads to surgical wait times well beyond recommendations, resulting in less than optimal patient outcomes [11].
Timely AIS detection first requires opportune PCP physical examination. Following that, the primary imaging method for spine deformity is the 3-foot standing plain radiograph with diagnosis, referral and triage consideration relying on its accurate interpretation [2]. For the vast majority of patients, this imaging initially occurs in the community. Pre-referral community spine x-rays can be of inadequate quality, necessitating re-imaging for 74% of patients [12].
Pediatric musculoskeletal radiographs are prone to misinterpretation leading to diagnostic error, however, current literature has focused on extremity injuries [13]. There are no current studies examining the diagnostic value of community spine radiographs and their interpretation. Inaccuracies in community spine radiology may result in delayed AIS diagnosis, referral, and/or misinformed triage thereby precluding opportunities for brace management. This study aims to establish the diagnostic accuracy of community spine radiology for AIS brace candidates.
Methods
Study design
A retrospective chart and radiographic review of AIS patients seen for initial visit at a university-affiliated tertiary-care pediatric hospital was conducted. The index test of community spine x-ray and its report, which is used for community AIS diagnosis, was compared to the reference standard, 3-foot standing spine x-ray, obtained at the initial orthopaedic visit and evaluated by orthopaedic spine specialists. The target diagnosis was an AIS patient who is a brace candidate, according to Scoliosis Research Society (SRS) criteria. Study methods and reporting follow the Statement for Reporting Studies of Diagnostic Accuracy [14]. The study was approved by the Research Ethics Board at the study institution and the affiliated university.
Setting
The study institution is the largest pediatric spine center in the country, specializing in non-operative and surgical management of spine deformity. The spine clinic receives over 900 referrals per year and treats approximately 1500 children for spine deformity per year, with approximately 80% of these being idiopathic scoliosis. For triage purposes, all patients referred to our center are required to have pre-referral imaging obtained to determine the need and urgency for specialist review. Those patients who have reported Cobb angles larger than 20° with suspected growth remaining (≤ Risser 2, < 18 months post-menarchal) OR approaching 20° with peak growth potential (e.g. Risser 0, pre-menarche status) are accepted for review in the spine clinic, under the assumption they are likely brace candidates [7]. The clinical assessment of these patients is typically expedited, and they are seen within 6 weeks to maximize opportunity for bracing.
Study patients
All patients seen in our spine program for initial consult in 2021 by a surgeon or advanced practice physical therapy practitioner were identified by diagnoses. The etiology of their scoliosis was verified from available referral information or initial consultation note, if necessary. A study cohort of AIS patients was obtained using consecutive sampling beginning January 1, 2021, until reaching the required sample size for the study.
Sample size calculation for categorical agreement analysis with expected proportions of management for observation, brace and surgery resulted in 93 patients [9]. Another calculation for detecting expected difference of Cobb angle of 6° (SD = 8°) resulted in 80 patients. Both sample size calculations were based on type I and type II error rates of 0.05 and 0.80, respectively. Given the results of these calculations, we set the target sample size as 100 patients.
Patient charts were reviewed for demographic, clinical and radiographic data (n = 281). Those with unreported index Cobb angle or with index imaging from our tertiary care institution were not eligible for the study. Patients younger than 10 years old, those with non-idiopathic etiologies, and those who had previous AIS consult were also excluded.
Diagnostic test definitions
The index test was the community spine x-ray obtained prior to referral and interpreted by community radiologist. Index images were considered community obtained if acquired at a community-based private practice clinic or at a hospital other than our own pediatric institution. Community radiology experience was obtained in years after residency and retrieved from the College of Physicians and Surgeons website. The Cobb angle of the largest curve, the imaging location and reporting radiologist were recorded from the community radiology report.
The reference standard was the three-foot standing EOS spine x-ray (EOS Imaging, Paris, France) obtained on initial visit and evaluated by orthopaedic spine specialists. The orthopaedic spine specialists included 3 staff orthopaedic spine surgeons, with an average of 18 years of experience, and 2 advanced practice physical therapy practitioners, with an average of 8.5 years of experience. Reference standard interpretations were made on a Picture Archiving and Communications System (PACS; Sectra Workstation IDS7, Version 23.1; Sectra AB, Linkoeping, Sweden) and recorded from the initial consultation note. Experienced pediatric orthopaedic specialist evaluation was considered the reference standard over the pediatric radiology report to most accurately reflect clinical practice. Current radiology reporting practices at our institution defer Cobb angle measurements to the orthopaedic department. Additional readers of the reference standard were not commissioned for consensus, as this study was designed to reflect clinical practice.
Radiographic interpretations were analyzed against clinical cut-off points. According to SRS criteria, patients who present with curves between 25–40° and Risser stage ≤ 2 are brace candidates [7]. We were unable to include Risser stage in diagnostic criteria given significant missing data in index reports. Therefore, a positive test to detect a brace candidate was dichotomized by Cobb angle, with curves below 25° and above 40° being outside bracing criteria.
Patient demographics and clinical characteristics
In addition to Cobb angle magnitude, age, sex, menarche status, Risser stage, referring specialty, index/reference image date, index image location (hospital or private practice) and index image quality were obtained. Menarche status was categorized by pre-menarche, 6 month intervals of post-menarche, and greater than 2 years post-menarche status to capture pubertal indicators related to peak growth velocity. Image quality was considered to be of insufficient quality if the entirety of the curve, sagittal profile, or pelvis were not visualized [15].
Characterization of AIS patients at initial presentation was determined by reference standard interpretation of Cobb angle and Risser stage according to SRS management guidelines: 0–24° (observation), 25–40° and Risser stage 0–2 (brace treatment), and 50° or more (surgical) [7]. Those with curves under 50° and with a Risser stage greater than 2 were considered skeletally mature. Late referrals were defined as those who present as likely surgical candidates at initial consult based on initial orthopaedic evaluation (Cobb angle ≥ 50° OR Cobb angle > 40° and Risser stage 0–2) [9].
Statistical analysis
Descriptive statistics were used for patients’ demographic and clinical profile. Means and standard deviations were calculated for patient age in years, index Cobb angle in degrees and radiology experience in years after residency. Frequencies and percentages were calculated for categorical data: sex, menarche status, Risser stage, referring specialty, index image quality issues, index imaging location, and presence of measurement discrepancy.
The accuracy, sensitivity, specificity, and predictive values of the index diagnosis were assessed against the reference standard through contingency table analysis if radiographs were obtained within 90 days (n = 111). Positive likelihood ratios were also calculated. Additional figures in Online Resource 1 illustrate diagnostic accuracy definitions and the mathematical equations utilized to compute these measures.
A true positive result represented a case where both the index test and the reference standard identified a curve magnitude within range for brace consideration. Conversely, a false negative result represented a case where the index test failed to identify a 25–40° Cobb angle that was interpreted as such on the reference standard. A true negative result represented a case where both the index test and the reference standard agreed that the curve magnitude was outside SRS bracing criteria. Conversely, a false positive result represented a case where the index test classified the patient as within range for brace consideration, when they were either suited for observation or surgical management given curve magnitude on the reference standard evaluation.
A 90-day interval between images was utilized based on the likelihood of true progression during that period [2]. To mitigate the uncertainty around true progression, all analyses were repeated on a sub-sample of data when index test was within 60 days of the reference standard (n = 67). Proportions of patients that were misdiagnosed based on index evaluation were compared for equality with precision of estimates reported as 95% confidence intervals, calculated using the Wilson method.
A p-value less than 0.05 was considered as statistically significant. Data were analyzed using the web-based R statistical programming language (R version 2021.9.1.372, https://www.R-project.org).
Results
Of the 281 AIS patients reviewed, 170 patients met the inclusion criteria. Of these, 111 had corresponding index imaging that were within 90-days of the reference standard. See flow diagram for inclusion/exclusion criteria. (Fig. 1)
The study cohort was typical of an AIS population: mostly female (76.6%) with an average age of 13.7 years (SD = 1.6). Most patients (69.1%, n = 76) had index imaging obtained from a private community clinic. From index images that were available on our PACS for evaluation, the majority (83.0%, n = 73) had at least one quality issue. Of these, most were of detriment to AIS evaluation with over half (n = 43) precluding full visualization of the curve and over one third (n = 32) without pelvic views. Skeletal maturity through Risser staging was not commonly evaluated on index reports (n = 110). Community radiology experience ranged from 2 to 46 years after residency. See Table 1 for patient demographic and clinical characteristics.
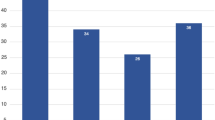
At initial evaluation, the mean Cobb angle of the major curve recorded was 33.2° (range = 14–60°, SD = 10.7) from index community reports and 38.8° (range = 10–79°, SD = 14.3) on the reference standard. (Fig. 2) From reference standard evaluations, the percentage of patients who presented as ideal brace candidates was 17.1% and the percentage of patients who presented as late referrals was 31.6%. (Fig. 3) Comparatively, based on the index evaluation of Cobb angle magnitude alone, the percentage of patients who presented as ideal brace candidates was 30.6% (p = 0.03).
Bar chart of initial presentation based on reference standard and SRS management indications. There were 17.1% of patients who presented as ideal brace candidates. The majority of patients (77.5%) presented outside bracing indications with 31.6% presenting as likely surgical candidates and another 45.9% who were skeletally mature with curves under 50°. A small number of patients (5.4%) presented with mild curves and were suitable for observation at initial consult
Measures of diagnostic accuracy
The accuracy of community spine radiology to detect a brace candidate was 65.8% (95% CI 56.5–73.9). The sensitivity of the index test was 65.4% (95% CI 51.8–76.8) with a false negative rate of 34.6% (95% CI 23.2–48.2). The specificity was 66.1% (95% CI 53.4–76.9) with a false positive rate of 33.9% (95% CI 23.1–46.6). Positive and negative predictive values were 63.0% (95% CI 49.62–74.6) and 68.4% (95% CI 55.5–79.0), respectively. [See Table 2] The positive likelihood ratio was 1.99, marginally increasing post-test probability. Further depiction of pre- and post-test probabilities utilizing a Fagan nomogram is available in Online Resource 2 [16].
Out of the total cohort (n = 111), there were 38 misdiagnoses and 89.5% (n = 34) of these were due to underestimation (95% CI 75.9–95.8). Of the total number of brace candidates (n = 52), 32.7% (n = 17) were missed because of underestimation (95% CI 21.5–46.2). From those that were misclassified as brace candidates (false positive), 35.3% (95% CI 18.1–56.7) of these were underestimated by ≥ 10° and were surgical candidates on initial orthopaedic exam despite being diagnosed as brace candidates on index evaluation.
When analyses were repeated with index images within 60 days of the reference standard (n = 67), the accuracy was similar: 67.2% (95% CI 55.3–77.2). The sensitivity of the index test was 75.9% (95% CI 57.9–87.8) with a false negative rate of 24.1% (95% CI 12.2–42.1). The specificity was 60.5% (95% CI 44.7–74.4) with a false positive rate of 39.5% (95% CI 25.6–55.3). Positive and negative predictive values were 59.5% (95% CI 43.5–73.7) and 76.7% (95% CI 59.1–88.2), respectively. The positive likelihood ratio was 2.55. The proportion of missed brace candidates because of underestimation was unchanged when looking at 60-day data (p = 0.37).
Discussion
This study demonstrated that there is poor diagnostic accuracy of community spine radiology for potential AIS brace candidates, with a considerable miss rate, otherwise known as the false negative rate, of 34.6%. This indicates that misinterpretations in community spine x-rays may contribute to missed opportunities for brace treatment. If patients are not properly identified as having a curve magnitude within a range for brace consideration, they are at risk for inappropriate triage that may result in denied or delayed access to treatment. Notably, nearly 90% of discrepancies were attributed to an underestimation of Cobb angle magnitude in index reports.
As the most common pediatric spine condition, AIS affects 1–2 in every 50 children [1]. Brace treatment significantly mitigates the risk of requiring spine surgery for youth with AIS [6]. Thus, the ramifications of the index test miss rate for possible AIS brace candidates are serious.
Over 30% of our study patients presented as near surgical candidates at initial presentation, a trend consistent with previous literature [9, 10]. The current standard for the surgical treatment of AIS continues to be PSIF. Aside from the peri-operative risks, spine surgery places significant economic burden on a publicly funded health care system with the cost of a single AIS surgery averaging nearly $60,000 [11].
Although Larson et al. recently reported no differences in the long-term health related quality of life (QoL) of AIS patients treated non-operatively or surgically, all patients with curves below 35° were excluded [17]. By failing to align brace treatment with SRS criteria, the authors introduced a significant selection bias. Conversely, the health-related QoL was higher in those adolescents who were diagnosed earlier and with curves under 40°, compared with those diagnosed after 13 years of age and with severe curvatures (> 40°) [18]. A meta-analysis, incorporating 7 studies that utilized only SRS-22 scores, compared braced patients to untreated patients. Satisfaction and overall QoL was higher in those treated with a brace [19].
Most experts agree there is good reason to limit the magnitude of spine deformity and to diagnose AIS patients when they are eligible brace candidates. The SRS clinical care guidelines for brace management delineate thresholds that can be appropriately utilized if the diagnostic tests that inform these measures are comprehensive and accurate. Using these guidelines, we found that community radiology had low diagnostic accuracy (65.8%) with over one third of patients being misdiagnosed (n = 38). Community radiology provides crucial diagnostic information along a patient’s journey from PCP to spine specialist. Most patients have pre-referral imaging obtained in the community and it is this index report that is primarily used for referral and triage decisions in our spine program [12].
Previous literature has demonstrated that delays in diagnosis and subsequent management in tertiary care can be attributed to misinterpreted or incomplete imaging results from the community [20]. To our knowledge, there is little literature specifying the error rate and its impact in pediatric spine imaging. In pediatric patients with cervical spine injuries, there was increased diagnostic error attributed to a non-pediatric radiologist compared to a pediatric radiologist interpreting computed tomography [21]. Authors, however, did not examine the clinical impact of reduced accuracy. Specific to AIS radiography, Cheung et al. determined that when the Cobb angle of a major curve was underestimated, due to postural variation, 14.3% of patients may have been overlooked for brace treatment [22]. Our study establishes novel information about the diagnostic accuracy of community spine radiology, but, whether this impedes AIS diagnosis and management is yet to be determined.
The SRS bracing guidelines are in the context of a growing child (Risser 0–2). We found that only 1 of 111 index reports evaluated skeletal maturity and nearly 30% of all index images did not visualize the pelvis, precluding any assessment of the iliac apophysis. Evaluating skeletal maturity in pediatric orthopaedics is vital to clinical decision making, particularly in adolescents to discern the timing of peak growth velocity [23]. The marked absence of Risser staging in community radiology reports implies triage and management projections lack meaningful reference. The proportion of predicted brace candidates on index test was higher than on the reference standard (30.6% vs. 17.1%) and this can be attributed to the requisite inclusion of Risser staging in the reference standard image. A 2024 systematic review examining AIS skeletal markers suggested that because growth indicators provide such key prognostic information, multiple indices could be employed for accurate predictions in progression [23]. Still, Risser staging continues to be the most common index used amongst clinicians because it is easily accessible on a standard spine radiograph [15].
The observed false positive rate of 33.9% indicates those patients initially identified within range for brace consideration were, in fact, outside the established SRS bracing criteria upon re-evaluation with the reference standard. In our clinical environment, the triage of potential brace candidates is expedited to maximize bracing efforts on a rapidly growing skeleton. The inaccuracies informing these decisions place a significant burden on the finite human health care resources within our publicly funded health care system. The significance of a nonessential pediatric orthopaedic referral has been well-described by other authors [24]. Specifically, the cost of an unnecessary AIS referral in 2019 has been estimated to be $780, including both patient and provider costs [25]. Based on the pediatric fracture population, discordant radiographic interpretation has been shown to affect an increase in specialty clinic visits to amend initial diagnostic information [13]. For a meaningful group of our patients, this resulted in receiving a surgical plan when unexpected, creating an anxiety provoking initial consultation and the potential for a mistrusting relationship with the orthopaedic specialist.
Ultimately for a diagnostic test to be clinically useful, it must have valid results that are helpful for decision-making as it relates to a patient’s health and management plan. Currently, community spine radiology is neither sensitive (65.4%) nor specific (66.1%) in its ability to detect AIS brace candidates and provides little applicability for clinical decision-making. Given potential radiation risks, a spine x-ray should provide beneficial results beyond confirming a clinical diagnosis which can be made on physical examination alone. Acknowledging that universal access to the reference standard is not feasible, improving community spine imaging is imperative given its role in AIS diagnosis.
Limitations
The limitations of this study include the methodological shortcomings of a retrospective review, including the potential for diagnostic review bias. The comparative reference standard evaluations were obtained from the initial orthopaedic consultation and were not reassessed by any additional readers. The reference standard measurements were made in the clinical setting, without blinding patient demographics, clinical history, or results of the index test. However, given this is a more accurate representation of the patient’s lived experience and closely reflects decision-making in clinical practice, the results are not likely to be significantly skewed. The interval time between images was selected to be 3 months (90 days) based on the plausibility of true progression and while additional analyses were completed for a shorter interval, this decreased the sample size from 111 to 67 participants. Despite that, the measures of diagnostic accuracy were very similar and the same proportions of underestimation were observed in both samples.
Another limitation of this study is related to the diagnostic criteria for a brace candidate as outlined by the SRS. The SRS has two main clinical parameters for the ideal brace candidate: (1) a Cobb angle between 25–40° and (2) a Risser stage of 0–2. However, by using a dichotomous cut-off point on an otherwise continuous measure with an accepted error of 5°, inherent measurement bias was introduced [7]. Nevertheless, with triage and clinical decision making, these internationally accepted guidelines are followed on the foundation that there is accuracy in diagnostic imaging evaluations. We were unable to include Risser staging as part of the diagnostic criteria in our study due to its absence in community radiology evaluations. If inclusion of skeletal maturity measures in reporting was standardized, then the inter-rater reliability of this should be evaluated both in community and tertiary care. Moreover, this would require spine x-rays to include visualization of the pelvis as standard practice.
Finally, this study was isolated to a single tertiary care pediatric center with comparison to index imaging from a wide catchment area. Index imaging location was not further differentiated between private clinic to hospital. Community acquired hospital images may have been obtained at an adult tertiary care center. Thus, results may be underestimated since this distinction is likely to have improved the accuracy of index imaging. Our results may not be generalizable to settings where pre-referral imaging is standardized. Furthermore, positive and negative predictive values depend on the prevalence of AIS and vary with pre-test probability in different healthcare settings. Our results may not be extrapolated to non-tertiary care centers.
Conclusion
With appropriate diagnosis, the majority of AIS patients can be successfully managed with brace treatment, thus avoiding surgery. Our results demonstrated that inaccuracies in measurement by community radiology result in underestimating the magnitude of the deformity leading to a notable miss rate for potential AIS brace candidates.
Data availability
The datasets generated and analyzed for the current study are available from the corresponding author upon reasonable request.
References
Weinstein SL, Dolan LA, Cheng JC, Danielsson A, Morcuende JA (2008) Adolescent idiopathic scoliosis. Lancet 371:1527–1537. https://doi.org/10.1016/S0140-6736(08)60658-3
Janicki JA, Alman B (2007) Scoliosis: review of diagnosis and treatment. Paediatr Child Health 9:771–776. https://doi.org/10.1093/pch/12.9.771
Kempen DHR, Heemskerk JL, Kaçmaz G et al (2022) Pulmonary function in children and adolescents with untreated idiopathic scoliosis: a systematic review with meta-regression analysis. Spine J 22(7):1178–1190. https://doi.org/10.1016/j.spinee.2021.12.011
Gallant JN, Morgan CD, Stoklosa JB et al (2018) Psychosocial difficulties in adolescent idiopathic scoliosis: body image, eating behaviors, and Mood disorders. World Neurosurg 116:421–432e1. https://doi.org/10.1016/j.wneu.2018.05.104
Murphy RF, Mooney JF (2016) Complications following spine fusion for adolescent idiopathic scoliosis. Curr Rev Musculoskelet Med 9(4):462–469. https://doi.org/10.1007/s12178-016-9372-5
Weinstein SL, Dolan LA, Wright JG, Dobbs MB (2013) Effects of bracing in adolescents with idiopathic scoliosis. N Engl J Med 369(16):1512–1521. https://doi.org/10.1056/NEJMoa1307337
Richards BS, Bernstein RM, D’Amato CR, Thompson GH (1979) Standardization of criteria for adolescent idiopathic scoliosis brace studies: SRS Committee on Bracing and Nonoperative Management. Spine 30:2068–2207. https://doi.org/10.1097/01.brs.0000178819.90239.d0
US Preventive Services Task Force, Grossman DC, Curry SJ et al (2018) Screening for adolescent idiopathic scoliosis: US preventive services task force recommendation statement. JAMA 319(2):165–172. https://doi.org/10.1001/jama.2017.19342
Anthony A, Zeller R, Evans C, Dermott JA (2021) Adolescent idiopathic scoliosis detection and referral trends: impact treatment options. Spine Deformity 9(1):75–84. https://doi.org/10.1007/s43390-020-00182-6
Hartley L, Jones C, Lui D, Bernard J, Bishop T, Herzog J, Chan D, Stokes O, Gardner A (2023) An examination of the number of adolescent scoliotic curves that are Braceable at First Presentation to a Scoliosis Service. Healthc (Basel) 11(3):445. https://doi.org/10.3390/healthcare11030445
Conference Board of Canada, The (2023) No Child Elects to Wait: Timely Access to Pediatric Spinal Surgery. Ottawa: The Conference Board of Canada
Kim DJ, Dermott JA, Lebel DE, Howard AW (2023) How useful is pre-referral spine imaging? Spine Deformity 51065–1070. https://doi.org/10.1007/s43390-023-00687-w
Al-Sani F, Prasad S, Panwar J, Stimec J, Khosroawshahi A, Mizzi T, Camp M, Colaco K, Kramer A, Boutis K (2020) Adverse events from Emergency Physician Pediatric Extremity Radiograph interpretations: a prospective cohort study. Acad Emerg Med 27(2):128–138. https://doi.org/10.1111/acem.13884
Cohen JF, Korevaar DA, Altman DG et al (2016) STARD 2015 guidelines for reporting diagnostic accuracy studies: explanation and elaboration. BMJ Open 6:e012799. https://doi.org/10.1136/bmjopen-2016-012799
O’Brien MF, Kuklo TR, Blanke KM et al (2004) Radiographic measurement manual. Spinal deformity study group (SDSG). Medtronic Sofamor Danek, Memphis
Côté P, Kreitz BG et al (1998) A study of the diagnostic accuracy and reliability of the Scoliometer and Adam’s forward bend test. Spine (Phila Pa 1976) 23(7):796–802. https://doi.org/10.1097/00007632-199804010-00011
Larson AN, Baky F, Ashraf A, Baghdadi YM, Treder V, Polly DW Jr, Yaszemski MJ (2019) Minimum 20-Year Health-Related Quality of Life and Surgical Rates after the treatment of adolescent idiopathic scoliosis. Spine Deform 7(3):417–427. https://doi.org/10.1016/j.jspd.2018.09.003
Lee H, Choi J, Hwang JH, Park JH (2016) Health-related quality of life of adolescents conservatively treated for idiopathic scoliosis in Korea: a cross-sectional study. Scoliosis Spinal Disord 11:11. https://doi.org/10.1186/s13013-016-0071-1
Meng ZD, Li TP, Xie XH, Luo C, Lian XY, Wang ZY (2017) Quality of life in adolescent patients with idiopathic scoliosis after brace treatment: a meta-analysis. Med (Baltim) 96(19):e6828. https://doi.org/10.1097/MD.0000000000006828
Eakins C, Ellis WD, Pruthi S, Johnson DP, Hernanz-Schulman M, Yu C, Kan JH (2012) Second opinion interpretations by specialty radiologists at a pediatric hospital: rate of disagreement and clinical implications. AJR Am J Roentgenol 199(4):916–920. https://doi.org/10.2214/AJR.11.7662
Hassan N, Butler C, DeCou J, Crumb T, Flohr S, Reischman D, Junewick J (2020) Pediatric cervical spine injuries on CT: difference in accuracy of interpretations by pediatric versus non-pediatric radiologists. Emerg Radiol 27(2):185–190. https://doi.org/10.1007/s10140-019-01743-7
Cheung PWH, Wong HL, Lau DSL, Cheung JPY (2023) Directed Versus Nondirected Standing postures in adolescent idiopathic scoliosis: its impact on curve magnitude, alignment, and clinical decision-making. Spine (Phila Pa 1976) 48(19):1354–1364. https://doi.org/10.1097/BRS.0000000000004731
Manzetti M, Ruffilli A, Barile F et al (2024) Is there a skeletal age index that can predict accurate curve progression in adolescent idiopathic scoliosis? A systematic review. Pediatr Radiol 54(2):299–315. https://doi.org/10.1007/s00247-023-05834-z
Hsu EY, Schwend RM, Julia L (2012) How many referrals to a pediatric orthopaedic hospital specialty clinic are primary care problems? J Pediatr Orthop 32(7):732–736. https://doi.org/10.1097/BPO.0b013e31826994a4
Meirick T, Shah AS, Dolan LA, Weinstein SL (2019) Determining the prevalence and costs of unnecessary referrals in adolescent idiopathic scoliosis. Iowa Orthop J 39(1):57–61
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data collection and analysis were performed by Dorothy Kim and Aya Mitani. The first draft of the manuscript was written by Dorothy Kim and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the Research Ethics Board at The Hospital for Sick Children and at the University of Toronto (#1000079131).
Conflict interests
None of the authors have any conflict of interest to declare related to the publication of this article. Dorothy Kim received graduate funding for this study from SickKids Clinician Scientist Training Program-Master’s, Canadian Institutes of Health Research Canada Graduate Scholarships-Master’s, and jointly funded Province of Ontario and University of Toronto Ontario Graduate Scholarship.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, D.J., Dermott, J.A., Mitani, A.A. et al. The diagnostic accuracy of community spine radiology for adolescent idiopathic scoliosis brace candidates. Eur Spine J (2024). https://doi.org/10.1007/s00586-024-08389-1
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00586-024-08389-1