Abstract
Purpose
We aimed to investigate surgical outcomes in octogenarians with subaxial cervical spine injuries and determine the predictors of complications and mortality.
Methods
Eligible for inclusion were all patients surgically treated between 2006 and 2018, with either anterior or posterior fixation for subaxial spine injuries. A cohort of octogenarians was identified and matched 1:1 to a corresponding cohort of younger adults. Primary outcomes were perioperative complications and mortality.
Results
Fifty-four patients were included in each of the octogenarian and younger groups (median age: 84.0 vs. 38.5). While the risks for surgical complications, including dural tears and wound infections, were similar between groups, the risks of postoperative medical complications, including respiratory or urinary tract infections, were significantly higher among the elderly (p < 0.05). Additionally, there were no differences in operative time (p = 0.625) or estimated blood loss (p = 0.403) between groups. The 30 and 90-day mortality rates were significantly higher among the elderly (p = 0.004 and p < 0.001). These differences were due to comorbidities in the octogenarian cohort as they were revoked when propensity score matching was performed to account for the differences in American Society of Anesthesiology (ASA) grade. Multivariable logistic regression revealed age and ASA score to be independent predictors of complications and the 90-day mortality, respectively.
Conclusions
Octogenarians with comorbidities were more susceptible to postoperative complications, explaining the increased short-term mortality in this group. However, octogenarians without comorbidities had similar outcomes compared to the younger patients, indicating that overall health, including comorbidities, rather than chronological age should be considered in surgical decision-making.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
During the past decades, the world’s population has witnessed an increase in life expectancy. In Western Europe, life expectancy has risen by around ten years since 1960, now reaching beyond 80 years [1]. As a result, a group of older and healthier patients has entered physicians’ daily practices [2,3,4,5]. Surgical consultations and admissions of octogenarians are increasingly common [3, 4, 6]. However, surgical outcomes associated with this group of patients have been poorly studied. Recently, the neurosurgical community has been actively questioning the efficacy and safety of surgery as a treatment option for octogenarians [3, 5, 7, 8]. This surge of interest has resulted in numerous publications, shedding light on the risks associated with neurosurgical interventions in this age group [4, 9,10,11,12]. Subaxial cervical spine injuries are known to frequently occur in the elderly and are classically associated with same-level falls [13, 14]. Larger studies have reported the overall incidence of traumatic cervical spine fractures to vary between 3 and 5% [14,15,16]. In the Norwegian population, Fredø et al. reported that nearly 25% of all cervical spine fractures occurred in patients older than 75 years [17]. Due to the associated risks, surgery is not always the primary option, and the patient may instead receive non-surgical treatments including immobilization and stiff neck collars [18,19,20]. Nonetheless, there are only a few studies targeting octogenarians and their clinical outcome after surgery for traumatic subaxial cervical spine fractures [21]. The aim of this study was to review the institutional experience at a primary neurosurgical referral center, of surgically treated octogenarians with subaxial cervical spine injuries, and to compare the outcomes with a matched cohort of younger adult patients with the same extent of injury. The intention was to identify predictors of complications and mortality to improve safety and aid in surgical decision-making.
Methods
Patient selection and variables
The study was approved by the Regional Ethical Review Board (Dnr: 2016/1708–31/4) that waived the need for informed consent. This study is also in line with the STROBE as well as the STROCSS criteria [22]. The study hospital is a publicly funded tertiary care center serving a region of approximately 2.3 million inhabitants and the region’s only level 1 trauma center. Patients were identified through the surgical management software Orbit (Evry Healthcare Systems, Solna, Sweden). Medical records and imaging data from digital hospital charts were retrospectively reviewed using the health record software TakeCare (CompuGroup Medical Sweden AB, Farsta, Sweden). The inclusion criteria were traumatic subaxial cervical spine injury, treated with anterior cervical discectomy and fusion (ACDF) or posterior fusion (PF) [23]. The exclusion criteria were non-traumatic cases, and cases with incomplete records. All patients surgically treated for subaxial cervical spine injuries during the period of 2006–2018 were screened, 354 ACDF and 188 PF cases were identified. Among these cases, 54 octogenarians (aged ≥ 80) were identified. The control group was defined as adult matched cases sorted by age and starting with the youngest. Matching was performed 1:1 based on AIS, surgical approach, and number of fused levels. The primary study outcomes included peri- and postoperative surgical and medical complications, and mortality. A composite outcome considering any type of complication including any medical or surgical complication was created and investigated as one of the primary outcomes. Estimated blood loss, and operative time were secondary outcomes.
Surgical technique
The surgical approach was determined by the senior surgeon based on the extent of injury and patient anatomy. All surgeries were performed by a senior neurosurgeon.
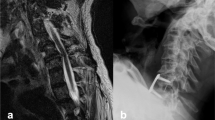
For ACDF, a standard right-sided Smith-Robinson approach was performed. Discectomy and osteophyte removal was performed with microsurgical technique to ensure spinal cord decompression. When the attending surgeon did not suspect any sub-ligamental fragments of disc or bone based on both imaging and the intraoperative view, the posterior longitudinal ligament (PLL) was not routinely opened. However, upon suspicion of cord compression due to disc, bone fragment, or hematoma, the PLL was opened to ensure complete cord decompression. PEEK cages were used in all cases. Adequate alignment and correct position of the cage was confirmed by fluoroscopy. An anterior plate was then positioned, bridging the vertebrae above and below the cage(s) and stabilized with bicortical screws under fluoroscopic guidance.
A PF was performed with the patient in the prone position and the head fixed in a Mayfield clamp. A midline incision was used to expose the posterior aspects of the spine. Lateral mass screws were placed, typically 2 levels above and below the injury. When needed, fixations were extended to the upper thoracic levels, where pedicle screws were placed. Cross-links were used when fixations extended 4 levels or more.
Postoperative follow-up
Patients were mobilized without collars after surgery. Postoperative clinical controls were usually performed within the first 24 h. In adherence with routine protocols, all patients underwent a postoperative CT scan within 24 h from surgery and follow-up CT scans at approximately four weeks and three months after the initial surgery. All patients were scheduled for clinical evaluation by their surgeon after three months. Additional imaging was performed when clinically indicated.
Matching and statistics
Case–control matching (1:1) considering the American Spinal Cord Injury Association (ASIA) Impairment Scale (AIS) at admission, surgical approach (anterior or posterior), and number of fused levels was performed to obtain two groups with similar injury severity profiles and surgical approaches. Tolerance factors were 0 for both AIS at admission and fixation approach and 1 for the number of fused levels. Other confounders such as the American Society of Anesthesiologists score (ASA) or underlying comorbidities were not accounted for to maintain external validity and generalizability of the findings, as elderly patients tend to have higher ASA scores and present with more comorbidities. Instead, multivariable regression was performed to adjust for the effect of other confounders on the primary outcomes. Propensity score matching using the K-nearest technique (caliper 0.2) and including all baseline variables was also performed to obtain balanced groups and validate the results of the multivariable analysis. The normality of continuous data was evaluated using the Shapiro–Wilk test. Since the distribution of continuous data deviated significantly from a normal distribution pattern, medians with interquartile ranges (IQR) were used. For descriptive purposes, categorical data are presented as numbers and proportions. Chi-square or Fisher exact tests were used as appropriate to compare proportions between groups, while the Mann–Whitney U or Kruskal–Wallis tests were used to compare medians between groups. Statistical significance was set to p < 0.05. Analyses were conducted using R software and SPSS.
Results
Baseline data
In total 542 patients were screened, and 54 octogenarians (median age: 84; IQR: 5) were identified and included. Case–control matching (1:1) was performed yielding a younger group of 54 patients (median age: 38.5; IQR: 25), with similar extent and severity of injuries. The two groups differed such that a higher frequency of Diffuse Idiopathic Skeletal Hyperostosis (DISH) (p < 0.001), and a higher ASA grade were found among octogenarians (p = 0.001). The trauma mechanism among octogenarians was primarily same-level falls (44%), while the younger group were more commonly involved in motor vehicle and bike accidents (49% combined; p < 0.001; Table 1). All patients had preoperative CT and MRI exams and did not differ in the level and extent of injury (p ≥ 0.05), apart from a higher frequency of facet joint fractures in the younger group (57% vs. 32%; p = 0.007; Table 2).
Outcome
In the matched cohort, surgery was performed on average within 48 h of the trauma and the majority of cases were treated with ACDF (72%) compared to PF (28%) (Table 3). There were no differences in operating time (140 vs. 150 min; p = 0.625) or the estimated blood loss (100 vs. 100 ml; p = 0.403) between octogenarians and the control group. The distribution of AIS on admission, short follow-up (median: four months; IQR: 3–5), and long-term follow-up (median: 73 months; IQR: 41–106) is represented in Fig. 1A for the younger cohort and Fig. 1B for the elderly. In the elderly cohort, 16% improved in AIS, while 13% experienced deterioration while in the younger cohort, 33% improved and 6% experienced deterioration (Table 3). However, these differences did not reach statistical significance (p = 0.144).
AIS distribution of the younger (A) and older (B) cohorts on admission (preop), at short-term follow-up (short FU; median: Four months; IQR: 3–5), and long-term follow-up (long FU; median: 73 months; IQR: 41–106). Preoperatively, AIS E represented patients who were neurologically intact, while patients who died before follow-up are classified as “na”
The frequency of postoperative medical complications was significantly higher among octogenarians, mainly respiratory and urinary tract infections requiring antibiotic therapy (61% vs. 18%; p < 0.05). Wound infections (p = 0.495) and other complications including thromboembolic events (n = 3), delirium (n = 3), dysphagia (n = 2), atrial fibrillation (n = 2), iatrogenic dural tear (n = 1) were equally prevalent in the groups (p = 0.221). Screw loosening detected on follow-up imaging was significantly more common in octogenarians (11% vs. 0%; p = 0.027; Table 3).
The mortality rate at 30- and 90-day after surgery, as well as at the end of the study period was significantly higher among octogenarians (p < 0.001). During a median follow-up period of 87 months (IQR: 67–141), 19 octogenarians died due to their cervical spine injury compared to only one patient in the younger group (40% vs. 11%; p < 0.001).
Among octogenarians, there were 15 patients (median age: 84) who died within 90-day postoperatively, and of whom 93% were males. They had a higher ASA score compared to those who remained alive at 90 days postoperatively (median ASA score 4 vs. 3). An anterior approach was performed in 80% of the patients who died and 69% of those who remained alive at 90 days. Also, the preoperative AIS tended to be significantly worse in patients who later died. The overall rate of complications was remarkably higher among patients who died with almost all these patients having experienced at least one complication (93% vs. 56%; Supplementary File, Table A).
Moreover, none of the octogenarians with an ASA score of 2 died within 30 or 90 days from the surgery. The 30- and 90-day mortality rates for octogenarians with an ASA score of 3 were 16% and 16%, and for an ASA score of 4 were 31% and 63%. Similarly, the end of study proportion of mortality attributable to the cervical injury were 0%, 27%, and 75% for octogenarians with ASA scores of 2, 3 and 4, respectively (p < 0.001).
On univariable logistic regression, variables that significantly predicted the occurrence of postoperative complications were age (> 80 years), the ASA score, previous history of malignancy, the presence of DISH, myelomalacia, concomitant traumatic brain injury (TBI), preoperative neurological impairment (AIS), posterior approach, higher number of fixated segments, and larger estimated blood loss. However, only age remained significant on multivariable regression, such that an age > 80 was an independent and significant risk factor for postoperative complications (OR: 6.6; CI 95%: 1.7–25.3; p = 0.006). Variables that significantly predicted 90-day postoperative mortality on univariable logistic regression were age (80 years), the ASA score, the presence of DISH, concurrent TBI, preoperative neurological impairment (AIS), as well as the occurrence of postoperative complications. However, only the ASA remained as an independent and significant risk factor for 90-day postoperative mortality (OR: 8.6; CI 95%: 2.3–31.8; p = 0.001; Table 4).
Propensity score matching yielded a balanced cohort of 42 patients, with 21 patients in each of the octogenarian and younger groups (Supplementary File, Table B). A love plot of standardized mean differences (SMD) is also provided as supplementary material (Supplementary File, Fig. A). Using this cohort, the results from the regression were validated as only the overall rate of complications significantly differed among the groups (p = 0.011), while the mortality rates at both 30- and 90-day were similar among groups (p > 0.999).
Discussion
The aim of this study was to review the outcomes of surgery in a cohort of octogenarians with traumatic subaxial cervical spine injuries. In the first part of the study, after adjusting for injury severity and surgical approach, it was found that octogenarians, in comparison to the younger cohort, had significantly higher rates of both postoperative medical complications and early mortality. According to data provided by the Swedish Statistical Central Bureau (SCB), the 90-day mortality rate among octogenarians in the general Swedish population during the same period of time was 2.69%. Our findings show a 90-day postoperative mortality rate of 28%, which is ten times higher than the expected mortality rate and arguably related to their trauma and surgery rather than age. We also found that the proportion of deaths attributable to the cervical spine injury was significantly higher among octogenarians (p < 0.001). There was only one mortality in the younger cohort, and it was related to other multitrauma injuries, not the cervical spine injury.
In this part of the study, other potential confounders such as the ASA score (a measure of comorbidity) or other comorbidities were not accounted for in the matching process to maintain an externally valid population of octogenarians. Therefore, while injury severity and surgical approach are unlikely to explain the worsened prognoses in this group of patients, the initial medical status of the patient may be an important factor. The second part of the study aimed to address this aspect by investigating the risk factors of the 90-day mortality using regression models. Adjusting for factors including age, preoperative neurological impairment, and the occurrence of postoperative medical complications, only ASA remained as a significant predictor of the 90-day mortality in the multivariable model (p = 0.001). This indicates that the medical status of patients, mainly reflected by the presence and severity of comorbidities, was superior to age itself, when predicting early mortality. Although caution may be advisable when surgically treating octogenarians, these results highlight the importance of considering overall health, including comorbidities, rather than chronological age in surgical decision-making. In other words, elderly patients with a favorable health status have a good potential for recovery with relatively low mortality risk. Accordingly, we found that 100% of octogenarians with an ASA score of 2 survived within the first 90-days after the surgery, as opposed to 84% and 37%, of those with ASA 3 and 4 scores, respectively (p < 0.001). In fact, in terms of mortality, octogenarians with an ASA score of 2 had outcomes comparable to the younger cohort. These findings were confirmed by the propensity score matched analysis revealing that, in a completely balanced cohort with similar baseline conditions, elderly and younger patients had similar mortality rates (p > 0.05). This suggests that the high mortality in elderly is mainly driven by confounders, of which the baseline health status, measured as ASA score, is the most prominent. These results corroborate the findings by Bernstein et al. identifying ASA score as a major and significant predictor of mortality [24]. In a study on cervical spine fractures among elderly (> 70 years), Tarawneh et al. also found that older patients with higher comorbidity rates were at a higher risk of mortality [25]. Similarly, Tan et al. studied the risk factors of mortality among elderly patients undergoing spine surgery and found the presence of comorbidities to be a key factor in the prediction of postoperative mortality [8, 25].
Manku et al. analyzed the impact of perioperative complications and their significance on long-term mortality in patients ≥ 70 years [26]. The study underlined the importance of postoperative complications in the octogenarian population since the estimated relative risk of death increased to 6.2 with complications in comparison to 1.7 in patients without complications. This is supported by the results of this study, showing postoperative complications to significantly predict mortality on univariable regression (p = 0.002). Poorer baseline health status and higher rates of comorbidity decrease the ability to tolerate postoperative complications such as infections, thromboembolic, and cardiopulmonary events, resulting in worse survival outcomes. One third of octogenarians (33%) with an ASA score of 2 developed postoperative complications, as opposed to 63%, and 88% of those with scores of 3 and 4, respectively (p = 0.041), indicating a tendency for complications to occur in patients with comorbidities. Multiple studies show that complication rates after undergoing spinal surgery in the elderly increase with number and severity of comorbidities [27,28,29]. However, while the ASA score was found to be a strong and independent predictor of mortality, the same could not be said for postoperative complications, where the ASA score was only significant on univariable but not multivariable analysis, probably due to the small sample size. This suggests that age is a stronger predictor than ASA score in predicting the occurrence of postoperative complications. In a large study on patients undergoing spinal fusion, Boakye et al. concluded that both comorbidities and age played a significant role in determining the postoperative complication risk [28]. The authors determined that octogenarians with no comorbidities had similar complication risks as 40-year-olds with two comorbidities.
In a study by Mao et al. it was reported that the rate of postoperative complications after any kind of spinal surgery was significantly higher among patients undergoing surgery for traumatic injuries compared to those undergoing elective procedures, and included deep venous thrombosis/pulmonary embolism, major respiratory events, and increased mortality [30]. In this study traumatic injuries in the octogenarian population were compared to a cohort of younger adults with similar extent of injury, revealing a significantly increased complication and mortality risk in the former. Considering the above, one can assume that octogenarians with several comorbidities are poor surgical candidates in the context of traumatic spine injuries. In addition, a higher frequency of screw loosening was detected on postoperative follow-up imaging among octogenarians when compared to the younger cohort (p = 0.027). This may be explained by differences in bone density [31]. The rate of reoperations did not significantly differ among groups (p = 0.495), and no case of screw loosening was considered clinically relevant.
Fasett et al. reported that patients older than 65 years of age were more likely to have less severe spinal cord injuries, with a higher percentage of AIS C and D injuries, compared to the younger population [30, 32]. This finding may stem from the higher incidence of central cord injuries in the elderly population, generally occurring after same-level falls with neck hyperextension, rather than high velocity trauma which is more commonly seen in younger patients [30, 32, 33]. In our cohort the main trauma mechanism in the octogenarian population was same-level falls (65%), as opposed to motor vehicle accidents in the younger population (37%). Patients aged 18–64 years have been shown to experience larger improvements in AIS over time when compared to patients aged 65 and above [34]. However, this could not be seen in our study as there were no differences in terms of long-term AIS outcome and improvement between the matched groups.
Strengths and limitations
This study is to the best of our knowledge one of the first to examine the short- and long-term outcomes after surgical treatment of subaxial cervical spine injuries in an octogenarian population. The study limitations include its retrospective and single-center design. Moreover, there was a considerable loss in sample size and subsequently power in the propensity score matched analysis which may have affected the significance of the results. Patient-reported outcome measures were not available, not allowing for health-related quality-of-life aspects to be studied in this population. Finally, we lacked data on conservatively treated patients since the study center does not have a searchable record of this.
Conclusion
Surgically treated octogenarians with subaxial cervical spine injuries were at a significantly higher risk of postoperative medical complications and short-term mortality compared to a younger group of controls. However, while age was an independent risk factor for postoperative medical complications, only comorbidities (ASA score), were identified as an independent predictor of postoperative mortality. Surgery was shown to be safe in octogenarians with lower ASA scores. For patients with higher ASA scores, strategies to prevent the occurrence of postoperative medical complications must be developed to ensure safety of the procedure and minimize postoperative mortality. In conclusion, overall health status rather than chronological age should be considered in surgical decision-making regarding octogenarians.
Data availability
The data may be provided upon reasonable request.
References
Murthi M (2016) In Europe, life gets shorter for some, World Bank Group. https://www.worldbank.org/en/news/opinion/2015/04/22/in-europe-life-gets-shorter-for-some. Accessed 30 Aug 2023
United Nations (2019) World Population Ageing 2019 Highlights, United Nations
Chibbaro S, Di Rocco F, Makiese O, Mirone G, Marsella M, Lukaszewicz AC, Vicaut E, Turner B, Hamdi S, Spiriev T, Di Emidio P, Pirracchio R, Payen D, George B, Bresson D (2010) Neurosurgery and elderly: analysis through the years. Neurosurg Rev 34:229–234
Whitehouse KJ, Jeyaretna DS, Wright A, Whitfield PC (2016) Neurosurgical care in the elderly: increasing demands necessitate future healthcare planning. World Neurosurg 87:446–454
Edlmann E, Whitfield PC (2020) The changing face of neurosurgery for the older person. J Neurol 267:2469–2474
Yoshihara H, Yoneoka D (2014) Trends in the incidence and in-hospital outcomes of elective major orthopaedic surgery in patients eighty years of age and older in the United States from 2000 to 2009. J Bone Jt Surg Am 96:1185–1191
Schär RT, Tashi S, Branca M, Söll N, Cipriani D, Schwarz C, Pollo C, Schucht P, Ulrich CT, Beck J, Z’Graggen WJ, Raabe A (2020) How safe are elective craniotomies in elderly patients in neurosurgery today? A prospective cohort study of 1452 consecutive cases. J Neurosurg 134:1113–1121
Tan JY-W, Kaliya-Perumal A-K, Oh JY-L (2019) Is spinal surgery safe for elderly patients aged 80 and above? Predictors of Mortality and Morbidity in an Asian Population. Neurospine 16:764–769
Steinberger J, Bronheim RS, Vempati P, Oermann EK, Ladner TR, Lee NJ, Kothari P, Caridi JM, Shrivastava RK (2018) Morbidity and mortality of meningioma resection increases in octogenarians. World Neurosurg 109:e16–e23
Stovell MG, Jenkinson MD (2014) Neurosurgery in octogenarians. Br J Neurosurg 28:611–615
Eichberg DG, Di L, Shah AH, Luther E, Richardson AM, Sarkiss CA, Ivan ME, Komotar RJ (2019) Brain tumor surgery is safe in octogenarians and nonagenarians: a single-surgeon 741 patient series. World Neurosurg 132:e185–e192
Ahmed N, Kuo Y, Shin S (2022) Octogenarian survival after neurosurgical procedures to treat severe head trauma. World Neurosurg 159:e425–e430
Asemota AO, Ahmed AK, Purvis TE, Passias PG, Goodwin CR, Sciubba DM (2018) Analysis of cervical spine injuries in elderly patients from, 2001 to 2010 using a nationwide database: increasing incidence. Overall Mortality, and Inpatient Hospital Charges, World Neurosurg 120:e114–e130
Passias PG, Poorman GW, Segreto FA, Jalai CM, Horn SR, Bortz CA, Vasquez-Montes D, Diebo BG, Vira S, Bono OJ, De La Garza-Ramos R, Moon JY, Wang C, Hirsch BP, Zhou PL, Gerling M, Koller H, Lafage V (2018) Traumatic fractures of the cervical spine: analysis of changes in incidence, cause, concurrent injuries, and complications among 488,262 patients from 2005 to 2013. World Neurosurg. 110:e427–e437
Wang H, Xiang Q, Li C, Zhou Y (2013) Epidemiology of traumatic cervical spinal fractures and risk factors for traumatic cervical spinal cord injury in China. J Spinal Disord Tech 26:E306–E313
Milby AH, Halpern CH, Guo W, Stein SC (2008) Prevalence of cervical spinal injury in trauma. Neurosurg Focus 25:E10
Fredø HL, Bakken IJ, Lied B, Rønning P, Helseth E (2014) Incidence of traumatic cervical spine fractures in the Norwegian population: a national registry study. Scand J Trauma Resusc Emerg Med 22:78
Nikhil JN, Lim JW-A, Yeo W, Yue W-M (2017) Elderly patients achieving clinical and radiological outcomes comparable with those of younger patients following minimally invasive transforaminal lumbar interbody fusion. Asian Spine J. 11(2):230–242
Delcourt T, Bégué T, Saintyves G, Mebtouche N, Cottin P (2015) Management of upper cervical spine fractures in elderly patients: current trends and outcomes. Injury 46(Suppl 1):S24–S27
Daentzer D, Flörkemeier T (2009) Conservative treatment of upper cervical spine injuries with the halo vest: an appropriate option for all patients independent of their age? J Neurosurg Spine 10:543–550
Sokolowski MJ, Jackson AP, Haak MH, Meyer PR Jr, Sokolowski MS (2007) Acute mortality and complications of cervical spine injuries in the elderly at a single tertiary care center. J Spinal Disord Tech 20:352–356
Mathew G, Agha R, Albrecht J, Goel P, Mukherjee I, Pai P, D’Cruz AK, Nixon IJ, Roberto K, Enam SA, Basu S, Muensterer OJ, Giordano S, Pagano D, Machado-Aranda D, Bradley PJ, Bashashati M, Thoma A, Afifi RY, Johnston M, Challacombe B, Ngu JC-Y, Chalkoo M, Raveendran K, Hoffman JR, Kirshtein B, Lau WY, Thorat MA, Miguel D, Beamish AJ, Roy G, Healy D, Ather HM, Raja SG, Mei Z, Manning TG, Kasivisvanathan V, Rivas JG, Coppola R, Ekser B, Karanth VL, Kadioglu H, Valmasoni M, Noureldin A (2021) STROCSS Group, STROCSS 2021: strengthening the reporting of cohort, cross-sectional and case-control studies in surgery. Int J Surg 96:106165
El-Hajj VG, Singh A, Blixt S, Edström E, Elmi-Terander A, Gerdhem P (2023) Evolution of patient-reported outcome measures, 1, 2, and 5 years after surgery for subaxial cervical spine fractures, a nation-wide registry study. Spine J 23:1182–1188
Bernstein DN, Thirukumaran C, Saleh A, Molinari RW, Mesfin A (2017) Complications and readmission after cervical spine surgery in elderly patients: an analysis of 1786 patients. World Neurosurg 103:859–868
Tarawneh A, Taqvi S, Salem K, Sahota O (2020) Cervical spine fragility fractures in older people: 5-year experience at a regional spine centre. Age Ageing 49:1102–1104
Manku K, Bacchetti P, Leung JM (2003) Prognostic significance of postoperative in-hospital complications in elderly patients. II. Long-term survival. Anesth Analg 96:590–594
Boakye M, Patil CG, Santarelli J, Ho C, Tian W, Lad SP (2008) Cervical spondylotic myelopathy: complications and outcomes after spinal fusion. Neurosurgery 62(2):455–462
Shen Y, Silverstein JC, Roth S (2009) In-hospital complications and mortality after elective spinal fusion surgery in the United States: a study of the nationwide inpatient sample from 2001 to 2005. J Neurosurg Anesthesiol 21:21–30
Wang MY, Green BA, Shah S, Vanni S, Levi ADO (2003) Complications associated with lumbar stenosis surgery in patients older than 75 years of age. Neurosurg Focus 14:e7
Mao G, Gigliotti MJ, Tomycz N, Altman DT, Philp FH (2019) Clinical outcomes after spine surgery for traumatic injury in the octogenarian population. World Neurosurg 129:e97–e103
Burger H, van Daele PL, Algra D, van den Ouweland FA, Grobbee DE, Hofman A, van Kuijk C, Schütte HE, Birkenhäger JC, Pols HA (1994) The association between age and bone mineral density in men and women aged 55 years and over: The Rotterdam Study. Bone Miner 25:1–13
Fassett DR, Harrop JS, Maltenfort M, Jeyamohan SB, Ratliff JD, Anderson DG, Hilibrand AS, Albert TJ, Vaccaro AR, Sharan AD (2007) Mortality rates in geriatric patients with spinal cord injuries. J Neurosurg Spine 7:277–281
Fancher TT, Król E, Rasmussen RW, Panait L, Dudrick SJ (2011) Cervical spine injuries; an outcome analysis. Pol Prz Chir 83:583–587
Wilson JR, Cadotte DW, Fehlings MG (2012) Clinical predictors of neurological outcome, functional status, and survival after traumatic spinal cord injury: a systematic review. J Neurosurg Spine 17:11–26
Acknowledgements
None
Funding
Open access funding provided by Karolinska Institute.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors report any financial or conflict of interest disclosure. AET was supported by Region Stockholm in a clinical research appointment.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
El-Hajj, V.G., Singh, A., Fletcher-Sandersjöö, A. et al. Long-term outcomes after surgery for subaxial cervical spine injuries in octogenarians, a matched population-based cohort study. Eur Spine J (2024). https://doi.org/10.1007/s00586-024-08312-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00586-024-08312-8