Abstract
Purpose
The global population is ageing rapidly. As a result, an increasing number of older patients with traumatic spine injuries are seen in hospitals worldwide. However, it is unknown how the incidence of traumatic spinal injury has developed over the past decade. Therefore, this study aimed to determine the incidence and characteristics of traumatic spinal injury in patients aged under and above 65 years.
Methods
During three time periods: 2009–2010, 2014–2015 and 2019–2020, all adult patients with traumatic spinal injury in the Netherlands were identified from the Dutch National Trauma Registry. Patient-related characteristics and 1-year mortality were collected from a subgroup of patients treated at a level-1 trauma centre, and patients aged ≥ 65 years were compared to patients aged < 65 years.
Results
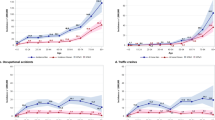
In the Dutch National Trauma Registry 25,737 patients with traumatic spinal injury were identified. The incidence of spine injury in patients > 65 years was 49.5/100,000/yr in 2009–2010, 68.8 in 2014–2015 and 65.9 in 2019–2020. The percentage of patients ≥ 65 years increased from 37% in 2009–2010, to 43% in 2014–2015, and to 47% in 2019–2020. In the subgroup of 1054 patients treated in a level-1 trauma centre, a similar increasing incidence was seen in patients aged ≥ 65 years. In these patients low energy falls were the most common trauma mechanism and the cervical spine was the most commonly injured region. Moreover, patients ≥ 65 years had significantly higher 1-year mortality compared with patients aged < 65 years, 22.7% versus 9.2%.
Conclusion
The incidence of traumatic spinal injury in older patients in the Netherlands has increased over the last 12 years. Almost half of the patients with traumatic spinal injury are currently aged ≥ 65 years. The increasing incidence and the high 1-year mortality highlight the need to modify existing treatment protocols for these patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The global population is ageing rapidly due to prosperity and better healthcare [1]. In 2050, the World Health Organisation estimates the proportion of the population aged ≥ 60 years to be 30% worldwide [1]. At present, almost one in five Dutch people is aged ≥ 65 years [2]. To assure a healthy and self-sufficient population, it’s advised to maintain an active lifestyle. The downside of remaining physically active is that older adults have an increased risk of traumatic events because of reduced motor and cognitive functions [3]. Moreover, in older patients a low energy fall can already result in spinal injury [4]. Additionally, comorbidities like osteoporosis and a stiff spine due to diffuse idiopathic skeletal hyperostosis (DISH) even further increase the risk of traumatic spine fractures [5]. Consequently, an increasing number of older patients are being seen in emergency rooms with spinal fractures worldwide. The absolute number of spinal fractures among patients aged 65 years or older has increased by 44% between 2007 and 2016[6]. However, it is currently unknown how the incidence of traumatic spinal injury has evolved during the last decade. Moreover, little is known regarding the differences in patient- and injury characteristics and trauma mechanisms between patients younger and older than 65 years of age. Differences between both age groups may require adjustment of current treatment protocols. The aim of this study was to describe patient characteristics, injury characteristics, trauma mechanisms, incidence and 1-year mortality rate of patients with traumatic spinal injury subdivided ≥ 65 and < 65 years of age in three time periods during the last 12 years.
Materials and methods
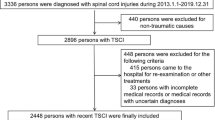
Study design/population
The Dutch National Trauma Registry (DNTR) collects data from trauma patients who visit an emergency department in the Netherlands within 48 h of trauma and were subsequently admitted to a ward [7]. To analyse a larger time-period without having to assess an unreasonably large number of patients a pragmatic study design with three time periods of 2 years was chosen. All patients with a spine fracture, spinal cord injury (SCI), or traumatic disc herniation (Injury coded following the Abbreviated Injury Scale 2008, supplementary material 1) from 2009–2010, 2014–2015 and 2019–2020 were identified from the DNTR [7] (Supplementary material 1). The incidence of spinal injury is determined with demographic information of the general Dutch population obtained from the Dutch national statistics office [2].
For further in-depth analysis, we identified from the DNTR patients those treated within the Erasmus MC University Medical Centre in Rotterdam (EMC), a large level-1 trauma centre in the Netherlands. Patient and injury characteristics were obtained from the electronic medical records (EMR) and diagnostic imaging.
Inclusion criteria were: spinal injury (spine fracture or SCI, or traumatic disc herniation) in patients aged ≥ 18 years. Exclusion criteria were: traumatic spinal injury without evident fractures and without objective neurological deficit.
All obtained data was stratified by < 65 and ≥ 65 years of age. Mortality rate was compared with the general Dutch population for both age groups and each time period. One-year mortality rates of the general Dutch population were obtained from the Dutch national statistics office [2].
The study was approved by the medical ethical committee of the EMC, MEC-2022–0032.
Outcome variables main analysis Dutch National Trauma Registry (DNTR)
Patients with spinal injury of both age groups were identified from the DNTR, of which 30-day mortality rate was obtained.
Outcome variables in-depth analysis from the EMC
The following variables were obtained from EMR and diagnostic imaging: age at time of injury, sex, cause of accident, location of injury, fracture type according to the AO (Arbeitgemeinschaft fur Osteosynthesefragen) Spine classification, Injury Severity Score (ISS), neurological deficit using the ASIA impairment score, type of treatment, complications, and 1-year mortality rate [8,9,10]. Polytrauma was defined as an ISS ≥ 16.
Non-surgical treatment included analgesia, mobilization as tolerated, thoracolumbar orthosis, cervical collar or halo vest. Surgical treatments included open spondylodesis or percutaneous stabilization, both with or without decompression. The level of each fractured vertebra was noted and scored according the most severe AO spine score for that level.
Statistical analysis
Statistical analyses were performed using SPSS 24, IBM.
Normality of continuous variables (age and ISS) was tested using the Shapiro–Wilk test. Both had a non-normal distribution and therefore descriptive statistics are presented as median with interquartile range (IQR). Dichotomous and categorical variables are presented as counts and percentages. Percentage of patients ≥ 65 years for each time period were compared with chi-square tests, for both DNTR and EMC data. Injury type, location of injury, treatment and complications in both age groups was compared with chi-square tests. Mortality rate in each time period was compared between both age groups by chi-square tests. Additionally each age group was compared to the general population by chi-square tests. A Bonferroni correction was used to correct for multiple comparisons, p-value < 0.05 after correction was considered as statistical significant.
Results
National incidence of traumatic spinal injury (DNTR)
On a national level, 25,737 patients with traumatic spinal injury were identified from the DNTR in the selected time periods. The percentage of patients ≥ 65 years with traumatic spinal injury significantly increased from 37.3% in 2009–2010 to 42.5% in 2014–2015 (p < 0.01), and to 46.5% in 2019–2020 (p < 0.001; Table 1). Thirty-day mortality was significantly higher in patients aged ≥ 65 years when compared to patients < 65 years (p < 0.001; Table 1).
In-depth analysis of patients from the Erasmus MC University Medical Centre in Rotterdam
Of all patients in the DNTR, we identified 1054 patients who were treated in the EMC. Of this group, 737 were male (69.9%), median age was 52.8 years (IQR 34.8), and 30.9% was aged 65 years or older. No statistical differences were observed between time periods in terms of age, sex, ISS or SCI (Table 2). Between 2009–2019 and 2019–2020, a trend towards increase of percentage of patients aged ≥ 65 years with traumatic spinal injury was found, 26.1% versus 33.9%, respectively (p = 0.066; Table 3).
Cause of spinal injury
The most common trauma mechanism in patients aged ≥ 65 years was a low-energy fall, defined as fall from standing height, ranging from 59.5 to 74.6% in the three time periods. The most common cause of spinal injury in younger patients was a traffic accident, ranging from 39.5 to 44.8% in the three time periods (Table 4).
Location of spinal injury
The cervical spine was the most commonly injured region of the spine in both age groups. In patients ≥ 65 years, 45.5 to 55.2% had a least on injured segment located in the cervical spine. In patients < 65 years, this was 30.0 to 32.8%. (Table 5). The most common fractured vertebra in patients aged ≥ 65 years was C2 (13.0%), and L1 in patients aged < 65 years (8.4%) (Fig. 1).
Type of fracture
The most common type of fracture in both age groups was the AO type A injury, ranging from 50.3 to 76.7% in patients ≥ 65 years and from 58.1 to 70.3% in patients < 65 years. The incidence of multiple type fractures in patients ≥ 65 years significantly increased from 4.5% in 2009–2010 to 12.1% in 2014–2015, and 32.2% in 2019–2020 (p < 0.001, Table 6).
Treatment
Non-surgical treatment was the most common treatment modality in both age groups in all time periods, ranging from 69.5 to 85.1% (Table 7).
Complications
The total proportion of complications was 26.6% for surgical treatment and 10.2% for non-surgical treatment. In patients aged ≥ 65 years, 18.3% had complications. In patients aged < 65 years this was 13.7%. More information regarding complications can be found in supplementary material 2.
Mortality
The 1-year mortality rate was significantly higher in patients aged ≥ 65 years compared to those aged < 65 years in 2014–2015 25.0% versus 7.7% (p < 0.001); 22.4% versus 10.8% 2019–2020, (p < 0.001). The 1-year mortality rate in patients with spinal injury was significantly higher for both age groups and in all study periods when compared to the general Dutch population (p < 0.001, Table 8).
Polytrauma patients (ISS ≥ 16) had a significantly higher 1-year mortality rate than non-polytrauma patients (ISS < 16) in all study periods and for both age groups. In 2014–2015 and 2019–2020 the 1-year mortality rate was significantly higher in polytrauma patients (ISS ≥ 16) > 65 years when compared to polytrauma patients (ISS > 16) < 65 years, 34.3% versus 12.0% (p = 0.007) and 29.9% versus 15.1% (p = 0.024) respectively (Table 8).
Discussion
Main findings
In this study we found a significant increase of spine injuries from 2009 to 2020 in patients aged ≥ 65 years, up to almost 69 per 100.000/year. In 2019–2020 almost half of all spine injuries occurred in patients aged ≥ 65 years, of which 1 out of 5 died within the first year after injury. In the patients aged ≥ 65 years, the most common trauma mechanism was a low energy fall, whereas in patients < 65 years this was traffic accident. Cervical fractures were the most common location of spinal injury in both age groups, this was stable over time. Spine injuries in patients older than 65 years became more complex over time, with more often multiple AO type fractures. Patients ≥ 65 years also had a higher 1-year mortality rate compared to patients < 65 years.
Incidence of traumatic spinal injury
Two Dutch epidemiological studies of traumatic spinal injury between 2007–2016 and 2010–2017 showed a similar increase in incidence in patients aged ≥ 65 years as found in the current study [6, 11]. Those studies described a larger increase in spinal fracture incidence using linear regression analysis, however no absolute or relative numbers were described [6, 11]. The increase in spinal injury in older patients was also suggested by several studies from European countries, the United States and China [12,13,14,15]. Nevertheless, only two studies report the actual increase. Zheng et al. [15] reported a 79% increase in incidence in spine fractures from 2013 to 2017. Additionally Blecher et al. [12] reported a 73% increase between 2003–2005 to 2015–2017. Both studies are in line with the 78% increase in absolute numbers found in the current study between 2009–2010 to 2019–2020.
The increase in spinal injury in patients aged ≥ 65 years appears to be related to both a higher incidence and growth of the population at risk. During the current study period, the Dutch population of ≥ 65 years increased from 2.5 million to 3.4 million [2]. However, the cause of increasing incidence among this population remains unclear. The current preference of many people to live independently at old age could play a role since low energy falls remain the most common cause of injury and frequently occur at home. Other presumed lifestyle changes or higher physical activity levels of patients ≥ 65 years seem not a cause of this increase, because no rise in sports or traffic related injuries was observed in this study.
Previously reported incidence of spinal injury ranges widely, from 21.5/100.000/y to 355/100.000/year [11, 15]. Reported incidence is highly dependent on the data source. Insurance or diagnosis code based registries often include both traumatic spine injuries and osteoporotic fractures. Difficulties to report these injuries separately result in very high incidence rates [14, 15]. Whereas incidence rates from databases on emergency room visits and hospital admissions result in much lower incidence rates [6, 11]. Moreover, we found different percentages of patients ≥ 65 years with spinal injury using the national data registry vs. the data obtained from the EMC, a level-1 trauma centre, 46.5% and 33.9% respectively. This demonstrates that it is important to interpret the incidence, patient and fracture characteristics with care and take the type of hospital(s) and source of data into account.
In the current study C2 was by far the most common injury location in patients ≥ 65 years. This phenomenon is frequently reported in literature and particularly odontoid fractures are well known for their high incidence in patients > 65 years of age due to the anatomical characteristic of the odontoid, osteoporosis and high risk of pseudoarthrosis [16].
Mortality rates
Thirty-day or in-hospital mortality rates for patients with spinal injury ranges from 2.0–9.6%, which is in line with the 2.1–10.9% 30-day mortality rates obtained from the DNTR in our study [11, 14]. One-year mortality rates after spinal injury are not commonly reported, while it may be a relevant outcome. Park et al. [17] report a 5.7% 1-year mortality rate based on a Korean insurance database (2007–2016). Additionally, they describe an increase in 1-year mortality for each decade in life, starting with 1.7% at 50–59 years and up to 10.5% at 80–89 years [17]. Nevertheless, this is still considerably lower than our 1-year mortality of 19.4–25% in patients ≥ 65 years. This may be due to the fact that the study by Park et al. is based on an insurance database with predominantly osteoporotic fractures, whereas the current study is based on a trauma registry of a level-1 trauma centre, consequently resulting in a higher mortality rate. Moreover, risk factors for mortality in patients ≥ 65 years are not well known. However frailty, BMI < 18.5 and older age (≥ 70 and ≥ 80) have been associated with higher mortality in this patient group, especially for surgically treated patients [18, 19]. Polytrauma (ISS ≥ 16) is a well known risk factor for mortality in trauma patients. The statistically significantly higher mortality rate is polytrauma patients with spine injury ≥ 65 years age found in the current study needs further research to identify if an ISS ≥ 16 is an independent risk factor for mortality in this patient group.
Strengths and limitations
A strength of this study is that we used prospectively collected data from the DNTR to calculate national incidence and mortality of spine injuries. Additionally, we supplemented the DNTR data with an in-depth analysis including detailed information of patients treated in our level-1 trauma centre. A limitation of the in-depth analysis is that younger patients with more severe trauma might have been overrepresented which could result in a lower percentage of patients with spinal injury ≥ 65 years of age and possibly a higher mortality rate. Additionally, COVID-19 could have influenced our results in the cohort 2019–2020, with less spine injuries due to less commuter traffic.
Implication for clinical practice
This study reports a clear increase in spine injuries in patients ≥ 65 years. With global aging, strategies are needed to avoid preventable adverse events and maintain quality of life of older patients. Older patients are at risk for postoperative complications, functional decline and mortality due to pre-existing medical conditions, medication effects, and frailty [20]. However non-operative management could lead to immobilization, pseudoarthrosis and other complications as well. Finding the right balance between these options is a difficult challenge. Early identification of pre-fracture frailty in older patients with a spinal fracture could be important for prognostic counselling, and medical-decision making to prevent adverse health outcomes [21].
Similar to hip fractures, geriatric co-management in spinal fractures may lead to a reduction of mortality, length of hospital stay, delirium, and other complications, and improve the long-term restoration of functionality in older adults [22]. This was already reported in a before-after intervention study in older patients with lumbar spine surgery, that showed a 30% reduction in mean length of in-hospital stay, a shorter time period between surgery and first mobilization, and a higher (54 vs 24%) proportion of patients that was discharged to home [23]. Furthermore, implementation of an ortho-geriatric pathway in a level-1 trauma centre, led to a 46% reduction of delirium in non-surgically treated patients aged ≥ 65 years [24]. Finally, a large British registry study in patients with acute surgery showed that postoperative geriatric medicine review was associated with significantly lower 30-day and 90-day mortality in patients aged ≥ 70 years [25].
Conclusions
The incidence of spinal injury in patients ≥ 65 years has increased significantly over the last 12 years in the Netherlands. Older patients have a higher risk of complications and 20% of the patients dies within 1 year after injury. The increasing incidence and high mortality highlight the need to modify existing treatment protocols for older patients with spinal injury. Early identification of pre-injury frailty and ortho-geriatric co-management may improve outcomes in older patients.
References
World Health Organization (2015) World report on ageing and health. World Health Organization
Statistics Netherlands (2022) Central Bureau for Statistics. https://opendata.cbs.nl/statline/#/CBS/en/navigatieScherm/thema?themaNr=5410
Callaway DW, Wolfe R (2007) Geriatric trauma. Emerg Med Clin North Am 25(837–860):x. https://doi.org/10.1016/j.emc.2007.06.005
Singh A, Tetreault L, Kalsi-Ryan S, Nouri A, Fehlings MG (2014) Global prevalence and incidence of traumatic spinal cord injury. Clin Epidemiol 6:309–331. https://doi.org/10.2147/clep.S68889
Westerveld LA, Verlaan JJ, Oner FC (2009) Spinal fractures in patients with ankylosing spinal disorders: a systematic review of the literature on treatment, neurological status and complications. Eur Spine J 18:145–156. https://doi.org/10.1007/s00586-008-0764-0
den Ouden LP, Smits AJ, Stadhouder A, Feller R, Deunk J, Bloemers FW (2019) Epidemiology of spinal fractures in a level one Trauma Center in the Netherlands: A 10 years review. Spine (Phila Pa 1976) 44:732–739. https://doi.org/10.1097/brs.0000000000002923
Driessen MLS, Sturms LM, Bloemers FW, Ten Duis HJ, Edwards MJR, den Hartog D, de Jongh MAC, Leenhouts PA, Poeze M, Schipper IB, Spanjersberg WR, Wendt KW, de Wit RJ, van Zutphen S, Leenen LPH (2020) The Dutch nationwide trauma registry: the value of capturing all acute trauma admissions. Injury 51:2553–2559. https://doi.org/10.1016/j.injury.2020.08.013
AO Spine calcification system (2023) https://aospine.aofoundation.org/clinical-library-and-tools/aospine-classification-systems
Roberts TT, Leonard GR, Cepela DJ (2017) Classifications in brief: American Spinal Injury Association (ASIA) impairment scale. Clin Orthop Relat Res 475:1499–1504. https://doi.org/10.1007/s11999-016-5133-4
Baker SP, O’Neill B, Haddon W Jr, Long WB (1974) The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma 14:187–196
Smits AJ, Ouden LPD, Deunk J, Bloemers FW (2020) Incidence of traumatic spinal fractures in the Netherlands: analysis of a nationwide database. Spine (Phila Pa 1976) 45:1639–1648. https://doi.org/10.1097/brs.0000000000003658
Blecher R, Yilmaz E, Ishak B, von Glinski A, Moisi M, Oskouian RJ, Dettori J, Kramer M, Drexler M, Chapman JR (2020) Uptrend of cervical and sacral fractures underlie increase in spinal fractures in the elderly, 2003–2017: analysis of a state-wide population database. Eur Spine J 29:2543–2549. https://doi.org/10.1007/s00586-020-06498-1
Dong Y, Peng R, Kang H, Song K, Guo Q, Zhao H, Zhu M, Zhang Y, Guan H, Li F (2022) Global incidence, prevalence, and disability of vertebral fractures: a systematic analysis of the global burden of disease study 2019. Spine J 22:857–868. https://doi.org/10.1016/j.spinee.2021.12.007
Lang S, Walter N, Freigang V, Neumann C, Loibl M, Alt V, Rupp M (2023) Increased incidence of vertebral fractures in German adults from 2009 to 2019 and the analysis of secondary diagnoses, treatment, costs, and in-hospital mortality. Sci Rep 13:6984. https://doi.org/10.1038/s41598-023-31654-0
Zheng XQ, Xu L, Huang J, Zhang CG, Yuan WQ, Sun CG, Zhang ZS, Wei C, Wang JX, Cummings SR, Xia WB, Wang SF, Zhan SY, Song CL (2023) Incidence and cost of vertebral fracture in urban China: A 5-year population-based cohort study. Int J Surg 109:1910–1918. https://doi.org/10.1097/js9.0000000000000411
Delcourt T, Bégué T, Saintyves G, Mebtouche N, Cottin P (2015) Management of upper cervical spine fractures in elderly patients: current trends and outcomes. Injury 46(Suppl 1):S24-27. https://doi.org/10.1016/s0020-1383(15)70007-0
Park SM, Ahn SH, Kim HY, Jang S, Ha YC, Lee YK, Chung HY (2020) Incidence and mortality of subsequent vertebral fractures: analysis of claims data of the Korea National Health Insurance Service from 2007 to 2016. Spine J 20:225–233. https://doi.org/10.1016/j.spinee.2019.09.025
Kweh BTS, Lee HQ, Tan T, Tew KS, Leong R, Fitzgerald M, Matthew J, Kambourakis A, Liew S, Hunn M, Tee JW (2023) Risk stratification of elderly patients undergoing spinal surgery using the modified frailty index. Global Spine J 13:457–465. https://doi.org/10.1177/2192568221999650
Lee SB, Park Y, Kim DW, Kwon JW, Ha JW, Yang JH, Lee BH, Suk KS, Moon SH, Kim HS, Lee HM (2021) Association between mortality risk and the number, location, and sequence of subsequent fractures in the elderly. Osteoporos Int 32:233–241. https://doi.org/10.1007/s00198-020-05602-x
Kessler RA, De la Garza RR, Purvis TE, Ahmed AK, Goodwin CR, Sciubba DM, Abd-El-Barr MM (2018) Impact of frailty on complications in patients with thoracic and thoracolumbar spinal fracture. Clin Neurol Neurosurg 169:161–165. https://doi.org/10.1016/j.clineuro.2018.04.014
Pulido LC, Meyer M, Reinhard J, Kappenschneider T, Grifka J, Weber M (2022) Hospital frailty risk score predicts adverse events in spine surgery. Eur Spine J 31:1621–1629. https://doi.org/10.1007/s00586-022-07211-0
Hafner T, Kollmeier A, Laubach M, Knobe M, Hildebrand F, Pishnamaz M (2021) Care of geriatric patients with lumbar spine, pelvic, and acetabular fractures before and after certification as a Geriatric Trauma Center DGU(®): a retrospective cohort study. Medicina (Kaunas) 57:794. https://doi.org/10.3390/medicina57080794
Adogwa O, Elsamadicy AA, Vuong VD, Moreno J, Cheng J, Karikari IO, Bagley CA (2017) Geriatric comanagement reduces perioperative complications and shortens duration of hospital stay after lumbar spine surgery: a prospective single-institution experience. J Neurosurg Spine 27:670–675. https://doi.org/10.3171/2017.5.Spine17199
Park C, Bharija A, Mesias M, Mitchell A, Krishna P, Storr-Street N, Brown A, Martin M, Lu AC, Staudenmayer KL (2022) Association between implementation of a geriatric trauma clinical pathway and changes in rates of delirium in older adults with traumatic injury. JAMA Surg 157:676–683. https://doi.org/10.1001/jamasurg.2022.1556
Oliver CM, Bassett MG, Poulton TE, Anderson ID, Murray DM, Grocott MP, Moonesinghe SR (2018) Organisational factors and mortality after an emergency laparotomy: multilevel analysis of 39 903 National Emergency Laparotomy Audit patients. Br J Anaesth 121:1346–1356. https://doi.org/10.1016/j.bja.2018.07.040
Association for the Advancement of Automotive Medicine (1998) The Abbreviated Injury Scale 1990 revision, update 1998. Des Plaines: AAAM
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors had a confict of interest with regards to the current study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bruggink, C., van de Ree, C.L.P., van Ditshuizen, J. et al. Increased incidence of traumatic spinal injury in patients aged 65 years and older in the Netherlands. Eur Spine J (2024). https://doi.org/10.1007/s00586-024-08310-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00586-024-08310-w