Abstract
Objective
To develop posterior reduction forceps for atlantoaxial dislocation and evaluate the preliminary clinical application of this forceps in assisting simple posterior screw-rod system reduction and fixation in the treatment of irreducible atlantoaxial dislocation.
Methods
Based on the posterior atlantoaxial screw-rod system, posterior reduction forceps was developed to assist simple posterior screw-rod system for the treatment of irreducible atlantoaxial dislocation. From January 2021 to October 2022, 10 cases with irreducible atlantoaxial dislocation were treated with this technique. The Japanese Orthopaedic Association (JOA) score was applied before and after surgery to evaluate the neurological status of the patient, and the Atlanto-dental interval (ADI) was measured before and after surgery to evaluate the atlantoaxial reduction. X-ray and CT were performed to evaluate internal fixation, atlantoaxial sequence and bone graft fusion during regular follow-up. MRI was performed to evaluate the status of atlantoaxial reduction and spinal cord compression after surgery.
Results
All 10 patients were successfully operated, and there were no complications such as spinal nerve and vascular injury. Postoperative clinical symptoms were significantly relieved in all patients, and postoperative JOA score and ADI were significantly improved compared with those before surgery (P < 0.05).
Conclusions
The developed posterior reduction forceps for atlantoaxial dislocation can assist the simple posterior screw-rod system in the treatment of irreducible atlantoaxial dislocation to avoid the release in anterior or posterior approach and reduce the difficulty of surgery. The preliminary results of this technique are satisfactory and it has a good application prospect.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Clinically, atlantoaxial dislocation can be divided into reducible, irreducible and bony irreducible types according to the degree of difficulty in reduction [1, 2]. For reducible dislocation, the focus of treatment is anatomical reduction, reliable fixation and fusion. Both the traditional Magerl screw fixation technique [3] and the current Goel-Harms screw-rod fixation technique [4, 5] can achieve this goal. For bony irreducible dislocation, since there is bony fusion between the atlas and axis during dislocation, reduction can only be achieved after complete osteotomy of all bony fusion sites, which is technically demanding during surgery, so the focus of treatment is decompression rather than reduction [6]; For irreducible dislocation, due to scar tissue formation between C1–C2 which causes great resistance to reduction, reduction cannot be achieved by traction under anesthesia and the limited reduction forces provided by current screw-rod systems, so release of scar tissue between C1–2 by anterior or posterior approach is often required first to decrease the resistance before reduction can be achieved using plate or screw-rod systems [7, 8]. However, the release also prolongs surgical time and increases surgical difficulty and risks.
Therefore, we designed a posterior reduction forceps for atlantoaxial dislocation (patent number: ZL201821593350.3) based on C1–2 posterior screw-rod system fixation, in order to overcome the resistance to reduction by the forceps without the need for release, aiming to greatly decrease surgical difficulty. The preliminary clinical application of this technique has achieved satisfactory results, which are reported as follows.
Methods
Design and components of the posterior atlantoaxial reduction forceps
The forceps has an “X” shaped design with two inverted “U” shaped arms crossing at the midpoint (Fig. 1). The distal ends of the two arms serve as handles for opening and closing by rotating around the crossing point as a pivot. The distance between the proximal ends of the two arms can be fixed by a bolt and nut on the handle end of arm 2. Arm 1 is the supporting arm with a hollow cylindrical structure. Its proximal end has a slot to clamp on the screw head of C2 pedicle screw and connecting rod. Arm 2 is the reduction arm, also in a cylindrical shape. Inside there is a movable screw structure that can push or pull. Its proximal end has hooks to attach to the upper and lower sides of the C1 screw rod slots. By rotating the nut at the distal end of the screw, the screw structure moves forward or backward to pull the C1 screw and achieve reduction of C1–2 dislocation.
Clinical data
General information
10 Patients were included, with 5 males and 5 females, aged 27–66 years old (mean 48.2 ± 15.6 years) (Table 1). All patients had different degrees of neurological deficits such as limb numbness and weakness. Preoperative imaging including cervical X-ray (neutral, flexion and extension), cervical CT and MRI were routinely performed. X-ray and CT showed C1–2 dislocation in all patients, with 2 combined old odontoid fractures and 4 combined free odontoid process. MRI showed different degrees of spinal cord compression at C1–2 level. All patients received skull traction for 1 week preoperatively but failed to achieve reduction, confirming the irreducible C1–2 dislocation. Mean preoperative JOA score was 10.3 ± 2.1, and preoperative ADI was 7.45 ± 0.6 mm (Table 2).
Surgical techniques
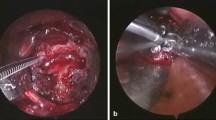
After tracheal intubation for general anesthesia, the patient was placed in a prone position with mild neck flexion. Intraoperative skull traction at 1/6 body weight was maintained. A posterior midline incision of about 6–8 cm was made from inion to C2 spinous process. The subperiosteal dissection exposed the posterior arch of C1, C2 lateral masses, while preserving the semispinalis capitis insertion on C2 spinous process. C1 pedicle screws were placed at least 3 mm above the C1 posterior arch midline, with an medial angulation of 5° and superior angulation of 5°. C2 pedicle screws were placed at the upper inner quadrant of the C2 lateral mass, exposing and identifying the medial and superior edge of C2 pedicle. The trajectory was 20°–25° medial angulation and 25°–30° superior angulation under direct visualization. C1 and C2 screws were placed (C1 screw can be pedicle screw or partial pedicle screw based on preoperative images and intraoperative findings. C2 screw can be pedicle screw, lamina screw or C2–3 transarticular screw). Appropriately contoured connecting rods were placed into the slots of unilaterally placed C1 and C2 screws. C1 screw nuts were first tightened to the rod. The supporting arm of the reduction forceps was then clamped onto the C2 screw head and rod. The hooks at the proximal end of the reduction arm were then attached to the upper and lower sides of C1 screw rod (Figs. 2D, 3I, J). The movable screw was gradually retracted to pull the C1 screw and C1 posteriorly under fluoroscopic guidance until satisfactory reduction was achieved (Figs. 2E, 3K). The C2 screw nuts were then tightened through the hollow supporting arm to complete reduction and fixation. The connecting rod was then placed on the contralateral side (Figs. 2F, 3L). Decortication of C1 posterior arch and C2 lamina was performed to prepare fusion bed. Autologous iliac bone graft was placed followed by wound closure over a drain.
A case of 61-year-old female, prognosed with free odontoid with irreducible atlantoaxial dislocation. A (CT) and B (MRI) showed obvious atlantoaxial dislocation and spinal cord compression. C The atlantoaxial could not be reduced used intraoperative traction after anesthesia. D The placement of posterior reduction forceps in the surgery. E The X-ray showed the status of reduction. F The X-ray showed the fixation of the rod. G (X-ray) and H (CT) showed the satisfactory atlantoaxial reduction, good internal fixation, no fracture or loosening. I (MRI) showed the decompression of spinal cord
A case of 66-year-old man, diagnosed with free odontoid with irreducible atlantoaxial dislocation. A and B (over flexion-extension position X-ray) and C (CT) showed the atlantoaxial dislocation. D (MRI) showed the compression of spinal cord. E–H The 3D-print model before the surgery. I, J The placement of the posterior reduction forceps in the surgery. K The X-ray showed the status of reduction. L The X-ray showed the fixation of the rod. M (anteroposterior X-ray), N (lateral X-ray) and O (CT) showed the satisfactory atlantoaxial reduction, good internal fixation, no fracture or loosening. P (MRI) showed the reduced spinal cord compression
Postoperative management
Intravenous antibiotics were routinely used for 1 day postoperatively. Drainage tube was removed 48 h after surgery. Patients were allowed to ambulate with cervical collar. Symptom relief was observed. Cervical X-ray, CT and MRI were obtained at 3–7 days after surgery to evaluate reduction, fixation and spinal cord decompression. Periodic follow-up with cervical X-ray and CT were conducted to assess fixation, atlantoaxial alignment and fusion.
Outcome evaluations
Japanese Orthopaedic Association (JOA) score for neurological status. Atlanto-dental interval (ADI) for assessing atlantoaxial reduction.
Statistical analysis
SPSS 26.0 was used for statistical analysis. Measurement data were expressed as mean ± standard deviation. Pre- and postoperative JOA scores were compared using Wilcoxon rank sum test. ADI was compared using paired t-test. P < 0.05 was considered statistically significant.
Results
The surgeries were successfully performed in all 10 patients, with mean surgical time of 114.9 ± 20.6 min, mean blood loss of 79.0 ± 41.4 ml (Table 1). There were no complications such as spinal cord or vertebral artery injuries Clinical symptoms were significantly improved in all patients postoperatively. Mean postoperative JOA score (14.5 ± 2.0) and ADI (2.15 ± 0.4 mm) were significantly improved compared to preoperative values (both P < 0.05) (Table 2). All patients were followed up for 3–24 months (mean 9.3 ± 6.2 months) (Table 1). X-ray and CT during follow-up showed no internal fixation failure or atlantoaxial redislocation. Bone fusion was achieved.
Discussion
For irreducible atlantoaxial dislocation, satisfactory reduction cannot be obtained simply relying on traditional internal fixation instruments. Although wire fixation techniques have some reduction capability, the reduction forces are insufficient to overcome scar tissue resistance in irreducible dislocations. The rigidity is also poor in all directions [9]. The Magerl transarticular screw technique has good 3-dimensional rigidity [10, 11] but cannot provide reduction forces and requires reduction to be achieved before screw placement. The C1–2 posterior screw-rod system [12,13,14] has some reduction capability, and separate screw placement in C1 and C2 is convenient. But its limited reduction forces are still insufficient to overcome the resistance in irreducible dislocations, so satisfactory reduction cannot be obtained in some cases with simple screw-rod fixation. Therefore, the focus has been on how to achieve release to decrease the resistance to reduction. Release can be achieved by anterior transoral approach directly, followed by reduction and plate fixation [15], or posterior screw-rod fixation [7]. Transoral release, reduction and fixation through single approach has the advantage of achieving release, reduction, fixation, decompression and fusion [16]. But it is a type II wound with higher infection risks compared to type I posterior wound. Therefore more surgeons prefer transoral release first, followed by posterior screw-rod fixation. However, intraoperative position change is complex after release when C1–2 is extremely unstable, posing risks of spinal cord injury [17]. For anterior release, some chose transmandibular approach or minimally invasive tubular access for release before posterior reduction and fixation to decrease infection risks and trauma [18, 19]. But the exposure and release are limited compared to extensive transoral release. Position change is still required. To avoid position change, some achieved release through simple posterior approach by opening C1–2 facet joints followed by screw-rod reduction and fixation [20]. However, the posterior venous plexus around the C1–2 joints poses difficulties in exposure and hemostasis. Also, variations like the vertebral artery entering spinal canal below C1 posterior arch can lead to vertebral artery injuries during release. Only the facet joints can be released through posterior approach. In summary, currently existing release techniques before reduction and fixation all have some limitations—higher infection risks for transoral approach; limited exposure and release for minimally invasive anterior release; risk of bleeding and vertebral artery injuries for posterior release; and the need for intraoperative position change for anterior followed by posterior approach. If reduction can be obtained without release, surgical difficulty can be remarkably decreased by avoiding release, reducing surgical time and blood loss.
For irreducible C1–2 dislocation, there is only soft tissue scar formation rather than bony fusion between the dislocated C1 and C2. So reduction without release is theoretically possible if sufficient reduction forces can be generated to overcome the resistance from scar tissue. However, the reduction forces provided by traditional screw-rod systems are insufficient. How can greater reduction forces be achieved? Our designed posterior reduction forceps for atlantoaxial dislocation uses C2 pedicle screw as the fulcrum to pull C1 screw and C1 by mechanical forces, providing additional external reduction forces for C1–2 reduction. As long as C1 screw does not get pulled out and C2 screw does not break during reduction, the scar tissue resistance can be overcome to achieve reduction without release. Our early clinical experience indicates that the forceps is easy to use during surgery, and the large reduction forces generated by rotating the screw can overcome scar tissue resistance. Satisfactory C1–2 reduction can be obtained without release in irreducible dislocations, remarkably decreasing the difficulty of surgery for such cases.
However, the design of the reduction forceps relies on fixation with C1 and C2 pedicle screws, so it cannot be used if pedicle screw placement in C1 and C2 is not feasible. For C1, the screw can be pedicle screw, partial pedicle screw, lateral mass screw or posterior arch hook, as long as the proximal end of the reduction arm can be attached. But C1 posterior arch screw cannot be used based on current C1 fixation techniques. For C2, the screw can be pedicle screw, pars screw, lateral mass screw or C2–3 transarticular screw, as long as the supporting arm can be clamped onto the screw head. This device is currently not suitable for the C2 laminar screw. Because the application of the posterior reduction forceps requires a fulcrum, and the force at this fulcrum is transmitted downwards. If the C2 laminar screw is used as the reduction fulcrum, the downward force may cause spinal cord compression, C2 laminar splitting, or fracture.
During surgery, pedicle screws satisfying the above criteria do not have to be placed bilaterally. Unilateral screw placement allowing use of the reduction forceps is sufficient to achieve reduction from one side, while the contralateral side just needs auxiliary fixation. Considering that the high riding VA cannot be treated with cervical pedicle screws as the reduction fulcrum, we propose the following solutions. If one side is high riding VA, the other side can be selected to apply posterior reduction forceps. If both sides are high riding VA, the option is to insert C2 pars screws or C3 pedicle screws as the reduction fulcrum. Cases with bilaterally unsuitable screw placement are extremely rare. Therefore, the reduction forceps can be applied in most clinical scenarios. The reduction capability is limited by the maximal anti-breaking strength of C2 screw and the maximal anti-pullout strength of C1 screw. So the C2 screw needs to withstand bending forces and the C1 screw needs high anti-pullout strength. In severe osteoporosis cases, screw augmentation with bone cement and improved screw design can enhance screw anti-pullout and anti-breaking capabilities to meet surgical reduction requirements. These will be important aspects for future research.
Our early results suggest that satisfactory C1–2 reduction can be obtained without release using the designed forceps and traditional screw-rod system, even with only unilateral forceps application. This indicates that the reduction capability of the forceps is powerful and may eliminate the need for release, remarkably decreasing surgical risks and difficulty in irreducible atlantoaxial dislocation. However, the case number is still limited and further application is needed to summarize the outcomes.
References
Xu J, Yin Q, Xia H et al (2013) New clinical classification system for atlantoaxial dislocation. Orthopedics 36:e95–e100
Yin Q, Liu J, Xia H et al (2003) Clinical classification, surgical treatment and outcome evaluation of atlantoaxial dislocation. Chin J Spine Spinal Cord 13(1):38–41
Meyer B, Kuhlen D (2013) Atlantoaxial fusion: transarticular screws versus screw-rod constructs. World Neurosurg 80(5):516–517
Goel A, Laheri V (1994) Plate and screw fixation for atlanto-axial subluxation. Acta Neurochir (Wien) 129(1):47–53
Harms J, Melcher RP (2001) Posterior C1–C2 fusion with polyaxial screw and rod fixation. Spine 26(22):2467–2471
Ma XY, Yang JC, Qiu F et al (2015) Clinical classification and surgical strategy selection for irreducible atlantoaxial dislocation. Chin J Orthop 35(5):474–480
Wang C, Yan M, Zhou HT et al (2006) Open reduction of irreducible atlantoaxial dislocation by transoral anterior atlantoaxial release and posterior internal fixation. Spine 31(11):E306–E313
Xu T, Maimait P, Maimait M et al (2017) One-stage posterior release, reduction and fixation for basilar invagination with irreducible atlantoaxial dislocation. Chin J Orthop 37(4):201–209
Henriques T, Cunningham BW, Olerud C et al (2000) Biomechanical comparison of five different atlantoaxial posterior fixation techniques. Spine 25(22):2877–2883
Lapsiwala SB, Anderson PA, Oza A et al (2006) Biomechanical comparison of four C1–C2 rigid fixative techniques: anterior transarticular, posterior transarticular, C1–C2 pedicle, and C1–C2 intralaminar screws. Neurosurgery 58(3):516–521
Stokes JK, Villavicencio AT, Liu PC et al (2002) Posterior atlantoaxial stabilization: new alternative to C1–2 transarticular screws. Neurosurg Focus 12(1):E6
Elliott RE, Tanweer O, Boah A et al (2014) Outcome comparison of atlantoaxial fusion with transarticular screws and screw-rod constructs: meta-analysis and review of literature. J Spinal Disord Tech 27(1):11–28
Bhowmick DA, Benzel EC (2014) Posterior atlantoaxial fixation with screw-rod constructs: safety, advantages, and shortcomings. World Neurosurg 81(2):288–289
Sim HB, Lee JW, Park JT et al (2011) Biomechanical evaluations of various C1–C2 posterior fixation techniques. Spine (Phila Pa 1976) 36(6):E401–E407
Xia H, Yin Q, Ai F et al (2014) Treatment of basilar invagination with atlantoaxial dislocation: atlantoaxial joint distraction and fixation with transoral atlantoaxial reduction plate (TARP) without odontoidectomy. Eur Spine J 23:1648–1655
Yin QS, Ai FZ, Zhang K et al (2005) Irreducible anterior atlantoaxial dislocation: one-stage treatment with a transoral atlantoaxial reduction plate fixation and fusion. Report of 5 cases and review of the literature. Spine 30(13):E375–E381
Yang J, Ma X, Xia H et al (2014) Transoral anterior revision surgeries for basilar invagination with irreducible atlantoaxial dislocation after posterior decompression: a retrospective study of 30 cases. Eur Spine J 23:1099–1108
Ren X, Gao F, Li S et al (2019) Treatment of irreducible atlantoaxial dislocation using one-stage retropharyngeal release and posterior reduction. J Orthop Surg (Hong Kong) 27:2309499019870465
Dong C, Yang F, Wei H et al (2021) Anterior release without odontoidectomy for irreducible atlantoaxial dislocation: Transoral or endoscopic transnasal? Eur Spine J 30:507–516
Wang J, Xu T, Pu L et al. (2020) Release, reduction, and fixation of one-stage posterior approach for basilar invagination with irreducible atlantoaxial dislocation. Br J Neurosurg 38(2):249–255
Funding
This work was supported by fund of the Guangzhou Municipal Science and Technology Project (No. 201803010046) and the National Natural Science Foundation of China (No. 82272582).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declared there was no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ma, X., Zou, X., Chen, J. et al. The development of posterior reduction forceps for atlantoaxial dislocation and its preliminary application in irreducible atlantoaxial dislocation. Eur Spine J (2024). https://doi.org/10.1007/s00586-024-08298-3
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00586-024-08298-3