Abstract
Purpose
High intensity zones (HIZ) in the lumbar intervertebral disk (IVD) can be associated with degenerative changes which may ultimately manifest as low back pain (LBP). However, the relationship between the prevalence of HIZ and lumbar degenerative parameters is still unclear. The purpose of this study was to determine the prevalence of HIZ in the lumbar spine, analyze the independent relationship between HIZ and lumbar degenerative parameters measured on MRI and X-ray and determine the association between HIZ and the presence of LBP.
Methods
A retrospective review of MRI data, X-ray data, and radiology reports for 136 consecutively recruited patients, above 18-years-age and with both lumbar MRI and X-ray scans was conducted. 57 patients with HIZ were identified. Patients without HIZ (n = 79) made up the control group.
Results
HIZ was prevalent in 41.9% of patients and in 11.0% of all lumbar IVDs. The odds of developing HIZ were 6.4 (Exp(B) 6.4, 95%CI [3.157–12.988]) and 3.0 (Exp(B) 3.0, 95%CI [1.603, 5.674]) times higher in IVDs with disk bulge/protrusion and nucleus degeneration, respectively. Odds of HIZ was also increased in disks with larger IVD angle (Exp(B) 1.1, 95%CI [1.034, 1.169]). The odds of patients presenting to imaging with LBP was 3.0 (OR 3.0, 95%CI [1.478–6.338]) times higher in the HIZ compared to the control group.
Conclusions
HIZ was prevalent in 41.9% of participants that were recruited in this study. Nucleus degeneration, disk bulge/protrusion and increased IVD angle were found to be independently associated with HIZ and since there is an increased likelihood of LBP, we posit that HIZ is likely a symptomatic and clinically meaningful diagnostic tool in the assessment of LBP.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
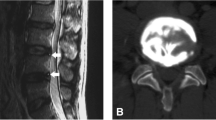
Many degenerative classifications of the lumbar spine have been devised to try and illustrate the degenerative process and provide insight on the symptomatic intervertebral disk (IVD). High intensity zones (HIZs), originally defined as a bright white signal in the posterior annulus fibrosus (AF) on T2 weighted (T2W) MRI are thought to be pathognomonic of a symptomatic IVD [1] (Fig. 1). However, literature regarding HIZ and its predictive value as the cause of discogenic LBP remains controversial.
Example High Intensity Zones on T1 and T2-weighted Magnetic Resonance Imaging. A sagittal slice from the magnetic resonance imaging (MRI) of three different patients with high intensity zones (HIZ) with different T1-weighted MRI classifications. (a) Represents an anterior HIZ on T2W MRI with corresponding isointense signal on T1W MRI, (b) Represents an anterior HIZ on T2W MRI with corresponding hyperintense signal on T1W MRI and (c) Represents a posterior HIZ on T2W MRI with corresponding hypointense signal on T1W MRI
Studies have found HIZ to be related to LBP [2,3,4]. Contrarily, other studies have observed HIZ in asymptomatic patients and found non-significant relationships between HIZ and LBP, leading researchers to question the significance of HIZ as a marker for LBP [5, 6]. To explain this Bogduk postulated that low intensity zones are asymptomatic fissures that need to be activated to form symptomatic HIZs. Subsequently, Liu et al. observed that symptomatic HIZs were significantly associated with a signal intensity of \(\ge\) 50% of the cerebrospinal fluid (CSF) [3]. Many authors have suggested that HIZ is a part of the disk degeneration process, finding significant associations between HIZ and degenerative changes, whilst others have not [1, 4,5,6,7].
To date, discography is still regarded as the gold standard for diagnosing LBP, however, it is highly invasive. Recent advances in literature regarding the pathogenesis of HIZ and using T1 weighted (T1W) MNRI scans have provided insight into the clinical significance of HIZ as a diagnostic indicator for LBP. Studies have observed HIZs exist circumferentially around the IVD, adding to the original definition that HIZs are posterior radial tears [1, 7]. HIZ has been proposed by authors to be fluid-filled zones in the AF resulting from inflammatory oedema [8]. Gadolinium DTPA-MR imaging has demonstrated enhanced signal intensity surrounding HIZs, positing HIZ’s association with extradural inflammation [9]. Histological studies have also backed up the presence of granulation tissue and resulting oedema [8]. Additionally, cadaveric studies have found that HIZs were generated by mucoid fluids containing fat [10]. Therefore, a single-subject multimodal approach was necessary to produce a more detailed definition of different HIZ phenotypes which can provide a higher clinical significance.
The studies mentioned previously have a variety of limitations, including inconsistency in the field strength of MR, no uniform consensus on the true definition of HIZ, and selection basis. As a result, the prevalence of HIZ and its relationship with LBP and lumbar degenerative parameters is still heavily debated. No studies to date have evaluated the relationship between HIZ and degenerative parameters observed on X-ray as potential risk factors. Hence, we performed a retrospective cohort study to assess the prevalence of HIZ in the lumbar spine, establish the independent relationships between IVDs with HIZs and lumbar X-ray and MRI degenerative parameters and identify the association between patients with HIZs and LBP.
Materials and methods
Study design and patient population
The study was IRB approved and conducted as a retrospective cohort study of adult patients (over 18 years of age) who had both lumbar MRI and X-ray scans conducted between January 2000 and May 2021 from our imaging centre. Written consent was obtained from all patients to be included in the study. The most recent MRI and X-ray scans were used if multiple scans of the same patient were available in the database. All MRI scans, X-ray scans, radiology reports, and demographic data were consecutively extracted. Patients were excluded if they had a history of lumbar spinal surgery prior to imaging or was diagnosed with a specific spinal pathology (i.e., vertebral fracture, malignancy, spinal infection, spondylarthritis, cauda equina etc.).
Data collection
The standing lateral X-ray images, axial and sagittal T1W and T2W MRI scans of the lumbar spine were assessed, and data points were collected before reading the radiology report. SS was trained by an experienced spine surgeon and back pain researcher with extensive experience in interpreting radiological images (XC). HIZ was defined as a lesion observed on T2W MRI where the signal intensity is at least 50% of the cerebrospinal fluid, contained within the AF and distinctly apart from the signal of the nucleus pulposus (NP) (Fig. 1) [3]. The location of the HIZ was classified as either anterior or posterior. X-ray degenerative parameters measured include disk heigh index, transforaminal height, IVD angle, sagittal alignment, sagittal translation, and the presence of bony spurs [5,6,7,8]. MRI degenerative parameters include nucleus degeneration, endplate changes, IVD protrusion/bulge, IVD extrusion, spinal stenosis, foraminal stenosis, and paraspinal muscle fatty infiltration. The specific measurement protocols of the lumbar degenerative parameters are outlined in Table 1. The radiology reports were prepared by board certified radiologists. The presence of LBP was defined as the inclusion of “LBP”, “Lumbar pain”, etc. in the radiological notes by the referring doctor as a clinical indication for MRI.
Data points for thirteen patients were also measured by a second rater (CS) to evaluate inter-rater reliability, and for a second time three weeks after initial extraction by the first author (SS) to evaluate intra-rater reliability. To enhance the quality and applicability of this study, each rater was blinded to their own measurements and findings of the other.
Statistical analysis
An independent t-test was used to analyze the difference in continuous radiological parameters between the two groups. Cohen’s d plot was used to calculate the effect size of the difference between two continuous groups [16]. Odds ratio (OR) with 95% confidence intervals (95%CI) was calculated to estimate risk. Pearson Chi-Square test was used to assess the independence of association and Phi and Cramer V was used to assess the strength of association between HIZ phenotypes and degenerative parameters and the presence of LBP. Logistic regression models were used to analyse the confounding status of lumbar degenerative parameters to determine the independent relationships between radiological parameters and HIZs. Inter-rater reliability was assessed using the intraclass coefficient estimates (ICC) based on single-rating, consistency, 2-way random effects model, and intra-rater reliability was assessed using ICC based on single-rating, absolute agreement, 2-way fixed effects model. ICC values of < 0.05, 0.5–0.75, 0.75–0.90, and > 0.90 indicated poor, moderate, good, and excellent reliability, respectively [17]. Statistical analyses were conducted using the commercially available software SPSS (version 20, IBM Corporation, New York, USA). The level of statistical significance was set at 5% (\(\alpha =0.05\)).
Results
Demographics
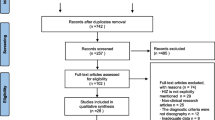
A flowchart depicting patient inclusion, exclusion, and separation into groups is shown in Fig. 2. Table 2 shows the demographic and clinical information of the included patients. Out of the 136 patients included in the study, 57 met the criteria for HIZ. The remaining 79 patients without HIZ were chosen as controls to compare with the cohort of HIZ patients. There were 40% more males than females who had HIZ (34 vs. 23, P < 0.005).
Flowchart Depicting Patient Inclusion, Exclusion and Separation of Patients and Intervertebral Disks. Flowchart representing the process of patient inclusion and exclusion of the study with specific data on the number of patients included/excluded at each step. It also shows how the patients included in the study were divided at a population-based level and a disk based level
Prevalence of HIZ
HIZs were noted in 57 (41.9%) patients. Out of the 680 lumbar IVD levels analyzed, 75 (11.0%) had HIZs. There was a higher number of posterior HIZ (n = 48) compared to anterior HIZ (n = 27). Posterior HIZs were more prevalent in lower lumbar levels compared to anterior HIZs in higher lumbar levels. The overall prevalence of anterior and posterior HIZ in each lumbar level is shown in Fig. 3.
Comparison of IVDs with and without HIZs
Disk levels with HIZs had more disk bulges/protrusion (84% vs. 37%, p < 0.0001), nucleus degeneration (76% vs. 38%, p < 0.001), and foraminal stenosis (40% vs. 25%, p < 0.01), and higher IVD angle (9.5 \(\pm\) 4.2 vs. 8.2 \(\pm\) 3.9, p < 0.005) when compared to disk levels without HIZs. The mean IVD angle for disks with HIZ was 0.35 standard deviations above disks without HIZ (Cohen’s d = 0.349, 95%CI [0.112, 0.621]). The Gardner-Altman estimation plots for IVD angle was shown in Fig. 4. The was no significant association and difference when comparing anterior and posterior HIZ (Table 3). HIZs and nucleus degeneration, disk bulge/protrusion, and foraminal stenosis were strongly (\({\chi }^{2}\)=39.088, phi and cramer V = 0.240, p < 0.001), very strongly (\({\chi }^{2}\)=60.365, phi and cramer V = 0.298, p < 0.001) and moderately (\({\chi }^{2}\)=7.534, phi and cramer V = 0.105, p < 0.01) associated, respectively.
Gardner-Altman Estimation Plot Comparing Intervertebral Disk Angle Between Disks with High Intensity Zones (test) and Disks without (control). Both IVD angle for disks with HIZ and disks without are plotted on the left axis. The mean difference is plotted on a floating axis on the right as a bootstrap sampling distribution and is depicted as a dot. The 95% confidence interval is indicated by the ends of the vertical error bar. Each data point is represented as a dot on the plot
Independent relationship between HIZ and radiological parameters
The binary logistic regression model was statistically significant, \({\chi }^{2}(4)\) = 82.390, p < 0.001. Disks with protrusion and nucleus degeneration were 6.4 (Exp(B) 6.404, 95%CI [3.157–12.988]) and 3.0 (Exp(B) 3.016, 95%CI [1.603, 5.674]) times more likely to have HIZ than healthy disks, respectively. Foraminal stenosis was non-significant. Increasing IVD angle was associated with an increased likelihood of HIZ (Exp(B) 1.100, 95%CI [1.034, 1.169]) (Table 4).
HIZ and low back pain
Patients with HIZs had a higher prevalence of LBP referral for MRI compared to the control (72% vs. 46%, p < 0.005). HIZ and LBP referral was very strongly positively associated (\({\chi }^{2}\)=9.367, phi and cramer V = 0.262, p < 0.005). The odds of having LBP were 3.1 times higher in HIZ patients when compared to the control group (OR 3.061, 95%CI [1.478–6.338]) (Table 5).
Intra-rater and inter-rater reliability
The intra-rater reliability for all measurements methods of the lumbar degenerative parameters included in this study was good-to-excellent from 0.764 (0.629–0.852) to 0.983 (0.972, 0.989) apart from sagittal translation which only had a moderate ICC of 0.579 (0.393, 0.720). The inter-rater reliability of the measurement methods was good-to-excellent from 0.776 (0.657, 0.857) to 0.982 (0.969, 0.989) apart from sagittal translation and sacral slope which both had moderate reliability with an ICC of 0.703 (0.556, 0.808) and 0.734 (0.331, 0.911), respectively (Table 6).
Discussion
To our knowledge, this is the first cohort study that reports the independent relationship between recumbent MRI-based HIZ, gravity-loaded standing x-rays, degenerative MRI parameters and clinical variables via a logistical regression. The prevalence of HIZ reported in studies has varied greatly. Our results showed that the prevalence of HIZs in this consecutively selected population was approximately 41.9%, with 11.0% of IVDs affected. Posterior HIZ was most common at the lower lumbar levels of L5/S1 (21/25) followed by L4/L5 (12/18), replicating many previous published results [2, 5, 6]. Dissimilar to other papers, we found 36% of the total HIZ to be anterior, with the most occurring at L3/L4 followed by L2/L3. This supports the postulation that upper lumbar (L1-L4) IVD degeneration has a developmental origin whilst lower lumbar (L4-S1) abnormalities are associated with aging and BMI [18]. However, this study cannot validate previous results as previous studies did not perform pan-disk analysis and did not have a uniform definition for HIZ.
This study was the first to introduce sagittal alignment measurements on X-ray. However, none were significantly associated with HIZ which demonstrates that HIZ is possibly a local disk based segmental issue with no associations to sagittal imbalance. The logistic regression model showed that the odds of developing HIZ was 6.4 and 3.0 times higher in disks with disk bulge/protrusion and disk degeneration, respectively. Increasing IVD angle was also found to increase the risk of developing HIZs. When confounding for factors, foraminal stenosis was found to be non-significant. These results support the view that degenerative findings can be a precursor to HIZ. The pathophysiological basis behind these associations can be attributed to the altered biomechanics of a degenerative disk. Many cadaveric studies have found reduced stiffness and increased range of motion in disks with HIZ. Instability in the disk results in increased fluid movement through the annular tear into the outer annulus causing disk degeneration and bulging/protrusion and consequently the formation of a HIZ [19]. Many articles have found a significant correlation between disk degeneration and foraminal width and foraminal area [20], which explains why the model has found that foraminal stenosis, independently, is not a risk factor for HIZ. Some caution is needed when interpreting these results as some technical assumptions may have been violated by the model. The measurements for each individual IVD were conducted independently, however, they were taken from the same patient (L1-S1) violating the independence of observation assumption [21]. This technical violation is very common in our field and many studies have found region specific differences within the lumbar spine to exist. As a result, the error due to correlated outcomes is minimized.
The clinical significance of HIZ is still heavily debated by researchers. The proportion of the population in industrial countries that have experienced LBP is at 84%. Approximately 85% percent of these cases are classified as non-specific LBP [22]. In our study, the percentage of patients with LBP in the HIZ group was higher at 72% compared to the control (46%) and the odds of having LBP were 3.1 times higher in the HIZ group compared to the control. This finding is due to the use of a qualitative definition for HIZ which allowed us to omit low intense zones [3]. It also underscores the fact LBP is only correlated to HIZs when large amounts of oedema and/or fatty infiltration occur because of inflammation or there is a large herniating process of the NP. This is supported by findings of mucoid fluids and inflammatory tissue in cadaveric and histology studies [8, 9, 23]. As a result, our results suggest that HIZ may be used independently in routine MRI and clinical assessments of patients with LBP, other degenerative parameters should be used in conjunction to formulate a diagnosis. Ultimately, HIZ may help in decreasing the number of non-specific LBP diagnoses.
Although there was higher prevalence of endplate changes in disks with HIZ compared to disks without (8% vs. 7.5%), this was not significant. Endplate changes represent severe toxic inflammatory responses in the vertebrae causing bone-oedema, re-vascularization, fatty infiltration, and subsequent repair which are all observed differently on MRI [24]. Therefore, future prospective pathohistological studies coupling T1W and T2W MRI are critical. It will allow us to further study the pathological connections between HIZ and lumbar degenerative parameters to see the progression of HIZ and determine if HIZ is a result of degeneration, if degeneration is a result of HIZ, or if HIZ and degeneration are both indications of nucleus pulposus material herniating into the annulus fibrosus meaning that there exists no functional difference between them.
The results of our studies were impacted by certain limitations. The first is that it is a retrospective cohort study that did not analyze patients’ clinical and radiological trends over time. Certain demographic information such as body mass index and socioeconomic status was not recorded. The population only included patients referred for MRI imaging, therefore the prevalence of HIZ in patients who do not present to a clinical or is not imaged is difficult to assess. The mean age was high in both the case and control groups, signifying the need for further studies that only look at certain age ranges. The nature (i.e., VAS) and duration of pain as well as disability scores were not recorded. Classification of patients into groups with and without pain based on the referral letters is imperfect and may be susceptible to classification error. This would bias the reported odds ratio towards 1 and mean the true underlying association between HIZ and pain may be somewhat stronger than observed here (Electronic Supplementary Material 1: ESM_1).
Conclusion
HIZ was found in 41.9% of patients. At all affected levels there was a significant association between HIZ and nucleus degeneration, disk bulge/protrusion, and foraminal stenosis on MRI and IVD angle on X-ray. The likelihood of having HIZ was 6.4 times and 3 times higher in IVDs with disk bulge/protrusion and nucleus degeneration, respectively. There was also an increased likelihood of HIZ in disks with increasing IVD angle. The odds of having LBP in patients with HIZ were 3.061 times higher than the control. According to the findings, HIZ is likely a clinically useful diagnostic parameter. However, creating a standardized definition for HIZ is essential for identifying problematic patients and minimizing harm from unnecessary management of non-specific LBP.
References
Aprill C, Bogduk N (1992) High-intensity zone: a diagnostic sign of painful lumbar disc on magnetic resonance imaging. Br J Radiol 65:361–369. https://doi.org/10.1007/s00586-012-2240-0
Wang ZX, Hu YG (2012) High-intensity zone (HIZ) of lumbar intervertebral disc on T2-weighted magnetic resonance images: spatial distribution, and correlation of distribution with low back pain (LBP). Eur Spine J 21:1311–1315. https://doi.org/10.1007/s00586-012-2240-0
Liu C, Cai HX, Zhang JF et al (2014) Quantitative estimation of the high-intensity zone in the lumbar spine: comparison between the symptomatic and asymptomatic population. Spine J 14:391–396. https://doi.org/10.1016/j.spinee.2013.06.078
Teraguchi M, Karppinen J, Luk K et al (2020) Lumbar high-intensity zones on MRI: imaging biomarkers for severe, prolonged low back pain and sciatica in a population-based cohort. Spine J 20:1025–1034. https://doi.org/10.1016/j.spinee.2020.02.015
Wang HL, Li ZH, Zhang CL, et al (2017) Correlation between high-intensity zone on MRI and discography in patients with low back pain. Medicine 96. https://doi.org/10.1097/MD.0000000000007222
Takeuchi M, Nagamachi A, Adachi K, et al (2018) Prevalence of high-intensity zones in the lumbar spine according to age and their correlation with other degenerative findings on magnetic resonance imaging. Spine Surg Relat Res 2:299–303. https://doi.org/10.22603/ssrr.2017-0071
Teraguchi M, Samartzis D, Hashizume H et al (2016) Classification of high intensity zones of the lumbar spine and their association with other spinal MRI phenotypes: the Wakayama Spine Study. PLoS ONE 11:e0160111. https://doi.org/10.1371/journal.pone.0160111
Peng B, Hou S, Wu W et al (2006) The pathogenesis and clinical significance of a high-intensity zone (HIZ) of lumbar intervertebral disc on MR imaging in the patient with discogenic low back pain. Eur Spine J 15:583–587. https://doi.org/10.1007/s00586-005-0892-8
Saifuddin A, Mitchell R, Taylor B (1999) Extradural inflammation associated with annular tears: demonstration with gadolinium-enhanced lumbar spine MRI. Eur Spine J 8:34–39. https://doi.org/10.1007/s005860050124
Ricketson R, Simmons JW, Hauser BO (1996) The prolapsed intervertebral disc: the high-intensity zone with discography correlation. Spine 21:2758–2762. https://doi.org/10.1097/00007632-199612010-00010
Guen YL, Joon WL, Hee SC et al (2011) A new grading system of lumbar central canal stenosis on MRI: an easy and reliable method. Skeletal Radiol 40:1033–1039. https://doi.org/10.1007/s00256-011-1102-x
Lee S, Lee JW, Yeom JS et al (2010) A practical MRI grading system for lumbar foraminal stenosis. AJR Am J Roentgenol 194:1095–1098. https://doi.org/10.2214/AJR.09.2772
Mandelli F, Nüesch C, Zhang Y et al (2021) Assessing fatty infiltration of paraspinal muscles in patients with lumbar spinal stenosis: Goutallier classification and quantitative MRI measurements. Front Neurol 12:1426. https://doi.org/10.3389/fneur.2021.656487
Chen X, Sima S, Sandhu HS et al (2022) Radiographic evaluation of lumbar intervertebral disc height index: an intra and inter-rater agreement and reliability study. J Clin Neurosci 103:153–162. https://doi.org/10.1016/j.jocn.2022.07.018
White A, Pnajabi M (1990) Clinical biomechanics of the spine. Lippincott
Ho J, Tumkaya T, Aryal S et al (2019) Moving beyond P values: data analysis with estimation graphics. Nat Methods 16:565–566. https://doi.org/10.1038/s41592-019-0470-3
Koo TK, Li MY (2016) A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 15:155–163. https://doi.org/10.1016/j.jcm.2016.02.012
Li Y, Samartzis D, Campbell D et al (2016) Two subtypes of intervertebral disc degeneration distinguished by large-scale population-based study. Spine J 16:1079–1089. https://doi.org/10.1016/j.spinee.2016.04.020
Schmidt TA, An HS, Lim T-H et al (1998) The stiffness of lumbar spinal motion segments with a high-intensity zone in the anulus fibrosus. Spine 23:2167–2173. https://doi.org/10.1097/00007632-199810150-00005
Splendiani A, Ferrari F, Barile A et al (2014) Occult neural foraminal stenosis caused by association between disc degeneration and facet joint osteoarthritis: demonstration with dedicated upright MRI system. Radiol med 119:164–174. https://doi.org/10.1007/s11547-013-0330-7
Stoltzfus JC (2011) Logistic regression: a brief primer. Acad Emerg Med 18:1099–1104. https://doi.org/10.1111/j.1553-2712.2011.01185.x
Maher C, Underwood M, Buchbinder R (2017) Non-specific low back pain. The Lancet 389:736–747. https://doi.org/10.1016/S0140-6736(16)30970-9
Lam K, Carlin D, Mulholland R (2000) Lumbar disc high-intensity zone: the value and significance of provocative discography in the determination of the discogenic pain source. Eur Spine J 9:36–41. https://doi.org/10.1007/s005860050006
Ohrt-Nissen S, Fritz B, Walbom J et al (2018) Bacterial biofilms: a possible mechanism for chronic infection in patients with lumbar disc herniation–a prospective proof-of-concept study using fluorescence in situ hybridization. APMIS 126:440–447. https://doi.org/10.1111/apm.12841
Acknowledgements
Chris Saulys for extracting the patient imaging parameters needed for inter-rater analysis.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. This work was supported by a University Postgraduate Award from The University of New South Wales to SS. Spine Labs is supported by unrestricted research grants to its institution by Baxter Inc and Nuvasive Inc.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
IRB approval was obtained from the Human Research Ethics Committee of the University of New South Wales (NRR-HC210515) for retrospective collection of anonymized patient’s lumbar MRI scans, X-ray scans, radiology reports, and demographic data from digital archives of St.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sima, S., Chen, X., Sheldrick, K. et al. Reconsidering high intensity zones: its role in intervertebral disk degeneration and low back pain. Eur Spine J 33, 1474–1483 (2024). https://doi.org/10.1007/s00586-024-08185-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-024-08185-x