Abstract
Background
Adolescent idiopathic scoliosis (AIS) is a spinal deformity that affects adolescents and poses a challenging public health problem. Compared to the general population, adolescents with AIS have a higher prevalence of hip dysplasia. However, the mechanisms underlying the impact of hip dysplasia on the coronal balance of the spine remain poorly understood. We hypothesized that the combination of AIS with hip dysplasia would exacerbate coronal imbalance.
Methods
We retrospectively analyzed the medical records and radiographs of adolescents diagnosed with AIS between 2015 and 2020. Participants were divided into two groups: those with hip dysplasia and those without. We recorded parameters related to the coronal deformity of the spine, sacral and pelvic obliquity, and center edge angle (CEA). We investigated differences in these parameters in those with and without hip dysplasia and analyzed their relationships in those with combined AIS and hip dysplasia.
Results
A total of 103 adolescents were included, 36 with hip dysplasia and 67 without. Those with hip dysplasia had significantly higher sacroiliac discrepancy (SID) compared to those without (t = − 2.438, P = 0.017). In adolescents with hip dysplasia, only iliac obliquity angle (IOA) was significantly correlated with SID (r = − 0.803, P < 0.001), with a linear relationship between them (r2 = 0.645, P < 0.001).
Conclusions
The incidence of hip dysplasia is higher in the AIS population. In adolescents with combined AIS and hip dysplasia, pelvic obliquity is greater, potentially contributing to the increased prevalence of low back pain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adolescent idiopathic scoliosis (AIS) is the most common form of scoliosis and affects 1–3% of the general population between the ages of 10 and skeletal maturity [3, 4]. Hip dysplasia, a disabling illness with an incidence of between 5 and 13% in the general population, causes an unstable ball-in-socket hip joint with insufficient coverage of the femoral head by the acetabulum [2, 5, 9]. Previous study has indicated that AIS adolescents have a higher risk of hip dysplasia than the general population [12, 14].
Both hip dysplasia and AIS can cause coronal imbalance. Zhang et al. [18] found that patients with unilateral developmental dysplasia of the hip (DDH) have increased coronal and sagittal spinopelvic parameters and decreased lumbar lordosis. These parameters have no correlation with the extent of dysplasia but are associated with low back pain in patients with unilateral DDH. Another study by Wen [16] revealed that most patients with adolescent idiopathic scoliosis (AIS) have trunk imbalance, which is more severe on the coronal plane than on the sagittal plane. However, it is unclear how coronal plane balance is affected in adolescent idiopathic scoliosis patients with concurrent hip dysplasia.
Therefore, the aim of this study was to investigate the impact of combined hip dysplasia and AIS on coronal balance in adolescents and hypothesized that adolescents with hip dysplasia would exacerbate the coronal imbalance. To our knowledge, there is currently no research investigating the effect of combined hip dysplasia and adolescent idiopathic scoliosis on coronal balance in adolescents.
Method
This was a retrospective cohort study from one medical center. Informed consent was waived for retrospective evaluation.
Patient selection
Following IRB approval, the medical information and radiographs of adolescents with adolescent idiopathic scoliosis (AIS) between 2015 and 2020 were retrospectively reviewed. Exclusion criteria involved adolescents with neurofibromatosis, a history of poliomyelitis and other neuromuscular diseases, and insufficiency of radiographic imaging (lack of long-length standing film in AP or Indistinctly displayed hip joint). In addition, the adolescents with lumbosacral transitional vertebrae were excluded. Study sample following inclusion and exclusion criteria can be observed in Fig. 1.
Radiograph parameters
Demographics including age, gender, and body mass index were gathered. The spinal and pelvic coronal parameters of the adolescents were evaluated. Two senior surgeons recorded the measurements to reduce the errors. The measurement parameters were as follows: (1) coronal Cobb angle, including proximal thoracic curve (PT-Cobb), main thoracic curve (MT-Cobb) and thoracolumbar or lumbar curve (TL/L-Cobb); (2) offset between central sacral vertical line (CSVL) and C7 vertebra plumb line (C7PL) (CSVL-C7PL); (3) sacral oblique angle (SOA); (4) iliac oblique angle (IOA); (5) center edge angle (CEA), which is measured as the angle between perpendicular to the transverse pelvic axis and centered on the femoral head; (6) lower-limb length discrepancy (LLLD), which is measured as the discrepancy in vertical distance between the upper edge of the lesser trochanter and teardrop line; (7) sacroiliac discrepancy (SID), which is defined as the difference between SOA and IOA. CEA less than 25° is diagnosed as hip dysplasia. Schematic measurements of these radiograph parameters are shown in Fig. 2.
The schematic measurements of these radiograph parameters. 2A. The schematic measurements of coronal spinal parameters. 2B. The schematic measurements of coronal sacroiliac and hip parameters. If the angle γ is less than 25°, acetabular dysplasia is diagnosed. PT: proximal thoracic curve; MT: main thoracic curve; TL: thoracolumbar curve; L: lumbar curve; C7PL: C7 vertebra plumb line; CSVL: central sacral vertical line; α: iliac oblique angle (IOA); β: sacral oblique angle (SOA); γ: center edge angle (CEA); a-b: lower-limb length discrepancy (LLLD); β-α: sacroiliac discrepancy (SID)
Pain assessment
The Visual Analogue Scale (VAS) was used to assess pain. The low back pain was examined after a 500-m walk. A score of 0 to 3 is regarded painless or mild, while a score of 3 or above is considered moderate or severe pain.
Data analysis
Inter-rater agreement was assessed on all pelvis and spine variables to ensure consistent measurements. The intraclass correlation coefficient (ICC) was used for all continuous and ordinal variables, while Cohen’s kappa was utilized for all nominal variables. The cutoffs for interpretation of the agreement coefficient were determined according to standard measures with poor agreement less than 0.40, fair agreement 0.40–0.60, good agreement 0.60–0.75, and excellent agreement 0.75–1.00. In the event of an inconsistency among observers, the most senior leader’s analysis was given priority.
Quantitative values are expressed as the mean ± standard deviation (SD) and 95% confidence intervals (CIs). Differences in age, BMI, and coronal spinopelvic variables between groups with and without hip dysplasia were evaluated using the non-paired t-test if the Shapiro–Wilk normal-distribution assessment test was good. Correlation analysis was performed on hip dysplasia group, and linear regression was conducted for correlative data. Chi-square test was used to compare the pain grading between the two groups.
Result
According to inclusion and exclusion criteria, a total of 103 adolescents were included in this study. The majority of included adolescents were female (83.5%, 86/103). Based on the diagnosis criteria of hip dysplasia, 36 adolescents were included in the hip dysplasia group, while the remaining 67 adolescents were assigned to the control group. The typical cases of the two groups are shown in Figs. 3 and 4.
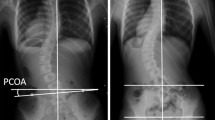
The typical case of AIS with AD. A 12-year-old girl diagnosed with AIS. Meanwhile, AD was determined by CEA less than 25°. The right CEA was 16.7°, and the contralateral CEA was 19.9°. γ1: right CE angle; γ2: left CE angle; AIS: adolescent idiopathic scoliosis; AD: acetabular dysplasia; CEA: center edge angle
The typical case of AIS without AD. A 15-year-old boy diagnosed with AIS. Meanwhile, AD was excluded by CEA more than 25°. The right CEA was 38.6°, and the contralateral CEA was 38.9°. γ1: right CE angle; γ2: left CE angle; AIS: Adolescent Idiopathic Scoliosis; AD: Acetabular Dysplasia; CEA: Center Edge Angle
The clinical characteristics of patients with AIS were evaluated. Mean PT-Cobb was measured at 22.41 ± 13.59. Mean MT-Cobb recorded a value of 51.22 ± 24.41. Mean TL/L-Cobb was measured as 28.47 ± 15.14. And mean CSVL-C7PL was found to be 17.20 ± 12.52. The aforementioned parameters, with the exception of PT-Cobb, did not show any statistically significant differences between the hip dysplasia group and the control group (P > 0.05). PT-Cobb, on the other hand, exhibited a statistically significant difference between the two groups (P = 0.037). Mean SOA was 5.58 ± 3.65 and 3.81 ± 3.25 in hip dysplasia and control groups, respectively. Mean SID were measured as 3.35 ± 3.51 and 1.96 ± 2.24 in hip dysplasia and control groups, respectively. SOA and SID showed statistically significant differences between the hip dysplasia group and control group (PSID = 0.017, PSOA = 0.013). VAS also displayed a statistically, but slightly significant difference between hip dysplasia group and control group (P = 0.027). In addition, there was also statistically significant difference in BMI between hip dysplasia and control groups (P = 0.045). The demographic characteristics, measurement parameters, and Lenke types of the included adolescents are shown in Table 1.
The ICCs for the intra-observer and inter-observer reliabilities of the measured parameters are shown in Table 2. All of the ICCs were > 0.9, indicating excellent consistency.
The correlation coefficients between SID and the other coronal spinopelvic variables in adolescents with hip dysplasia are shown in Table 3. Only IOA showed a significant correlation with SID (β = − 0.803, P < 0.001). It is noteworthy that in the pairwise correlation analysis of other parameters, we found a correlation between IOA and SOA (r = 0.642, P < 0.001).
Table 4 shows the regression analysis result between SID and IOA in adolescents with hip dysplasia. Regression coefficient was 0.645, while F-statistic and P-values were 61.815 and 0.000, respectively. Finally, the linear regression model was expressed as Y = 3.946–0.617X (t = 6.824, P < 0.001). The residuals plot about Y is shown in supplementary material 1.
As shown in Table 5, the adolescents with hip dysplasia had a statistically higher rate of moderate or severe low back pain than those without hip dysplasia (F = 5.671, P = 0.031).
Discussion
In our study, SID is considerably higher in individuals with adolescent idiopathic scoliosis who have hip dysplasia than in adolescents who do not have hip dysplasia. Specially, in AIS adolescents with hip dysplasia, we discovered a negative linearly correlation between SID and IOA. To the best of our knowledge, this is the first report about the effect of combined hip dysplasia and adolescent idiopathic scoliosis on coronal balance in adolescents.
It is not rare for AIS to be accompanied by hip dysplasia. According to Talmage et al. [14], the prevalence of hip dysplasia in EOS population was 11.1%, which was more than 3 times that of the general population. In our study, the incidence of hip dysplasia in AIS population was as high as 35%, which was greater than previously reported. The ethnic difference is one of the possible causes. Many studies found that the incidence of hip dysplasia in live births varied widely, with 75/1000 occurring in India, 6.6/1000 in Canada, and 1.3/1000 in Mexico [1, 6, 7].
Hip dysplasia may cause pelvic obliquity, thereby worsening the severity of spinal curvature. Sun et al. [13] discovered that adolescents with hip dysplasia have increased frequency of spinal anomalies visible on standard hip radiographs. Therefore, we speculate that hip dysplasia will aggravate the coronal imbalance of AIS. However, in our study, we found that hip dysplasia did not worsen the coronal imbalance of the spine, but significantly increased the sacroiliac discrepancy. More notably, in the adolescents with hip dysplasia, there was a clear correlation between SID and IOA, but not SOA. As a result, it can be proved that IOA is the decisive factor in patients with hip dysplasia, where IOA has a certain influence on SOA. Conversely, the influence of SOA on IOA is minimal, leading to the correlation between IOA and SOA, but only the difference between the two is strongly correlated with IOA, which suggests that hip dysplasia exacerbates the pelvic obliquity, but the sacroiliac joint corrects it. Similar to our study, Yu et al. [17] found that the sacroiliac joint compensates for the coronal imbalance caused by hip dysplasia in a study on the relationship between sacral and iliac obliquity in individuals with hip dysplasia.
As for the axes of movement passing obliquely across the pelvis, sacroiliac joint dysfunction is considered to cause low back pain. According to our findings, the adolescents with hip dysplasia experienced more low back pain after 500-m walk. Also, the adolescents with hip dysplasia had a higher rate of moderate or severe low back pain, which could have a greater impact on the quality of life, compared to those without hip dysplasia. Prather et al. [8] reported that physical examination findings indicating hip dysfunction are frequent in individuals presenting with low back pain. One possible explanation is that sacroiliac joint dysfunction was more frequent in adolescents with both AIS and hip dysplasia than in those with only AIS. Low back pain is not a unusual complaint among adolescents with AIS, and in the group of kids with scoliosis, the lifetime prevalence of back pain was close to 60%, nearly twice as high as in non-scoliosis group [11, 15]. Šarčević et al. [10] confirmed that there was a strong positive association between sacroiliac joint dysfunction and low back pain. In combination with our study, hip dysplasia may cause more prominent sacroiliac joint dysfunction due to the increasing SID, which lead to more frequent and serious low back pain in AIS adolescents.
There are several limitations in our study. Firstly, we did not study the impact of hip dysplasia on sagittal plane balance or spinal deformity in AIS, which will be addressed in our future research. Secondly, we cannot predict whether these adolescents with both hip dysplasia and AIS will continue to have this association between IO and SID as they mature or undergo spinal surgery. Thus, the results in our study may be appropriate for adolescents without spinal surgery. Last but not the least, we did not specifically select individuals with unilateral hip dysplasia, because even with bilateral hip dysplasia, the effect on lower-limb length and pelvic muscle is asymmetrical.
In summary, the incidence of hip dysplasia is high in AIS. Pelvic obliquity is greater in adolescents with combined AIS and hip dysplasia and was corrected by the sacroiliac joint, which may contribute to increased incidence of low back pain. Therefore, for adolescents with both hip dysplasia and AIS, more attention should be paid to pelvic obliquity to reduce the associated low back pain.
References
Chand S, Aroojis A, Pandey RA, Johari AN (2021) The incidence, diagnosis, and treatment practices of developmental dysplasia of hip (DDH) in India: a scoping systematic review. Indian J Orthop 55(6):1428–1439. https://doi.org/10.1007/s43465-021-00526-y
Ellsworth BK, Sink EL, Doyle SM (2021) Adolescent hip dysplasia: what are the symptoms and how to diagnose it. Curr Opin Pediatr 33(1):65–73. https://doi.org/10.1097/MOP.0000000000000969
Kuznia AL, Hernandez AK, Lee LU (2020) adolescent idiopathic scoliosis: common questions and answers. Am Fam Physician 101(1):19–23
Liu Y, Pan A, Hai Y, Li W, Yin L, Guo R (2019) Asymmetric biomechanical characteristics of the paravertebral muscle in adolescent idiopathic scoliosis. Clin Biomech (Bristol Avon) 65:81–86. https://doi.org/10.1016/j.clinbiomech.2019.03.013
Matsuda DK, Wolff AB, Nho SJ, Salvo JP Jr, Christoforetti JJ, Kivlan BR et al (2018) Hip dysplasia: prevalence, associated findings, and procedures from large multicenter arthroscopy study group. Arthroscopy 34(2):444–453. https://doi.org/10.1016/j.arthro.2017.08.285
Mendez-Dominguez N, Alvarez-Baeza A, Estrella-Castillo D, Lugo R, Villasuso-Alcocer V, Azcorra H (2022) Ethnic and sociodemographic correlates of developmental dysplasia of the hip in newborns from Yucatan, Mexico. Am J Hum Biol 34(6):e23724. https://doi.org/10.1002/ajhb.23724
Pollet V, Percy V, Prior HJ (2017) Relative risk and incidence for developmental dysplasia of the hip. J Pediatr 181:202–207. https://doi.org/10.1016/j.jpeds.2016.10.017
Prather H, Cheng A, Steger-May K, Maheshwari V, Van Dillen L (2017) Hip and lumbar spine physical examination findings in people presenting with low back pain, with or without lower extremity pain. J Orthop Sports Phys Ther 47(3):163–172. https://doi.org/10.2519/jospt.2017.6567
Pun S (2016) Hip dysplasia in the young adult caused by residual childhood and adolescent-onset dysplasia. Curr Rev Musculoskelet Med 9(4):427–434. https://doi.org/10.1007/s12178-016-9369-0
Sarcevic Z, Tepavcevic A (2019) Association between adolescent idiopathic scoliosis and sacroiliac joint dysfunction in young athletes: a case control study. Medicine (Baltimore) 98(15):e15161. https://doi.org/10.1097/MD.0000000000015161
Sato T, Hirano T, Ito T, Morita O, Kikuchi R, Endo N et al (2011) Back pain in adolescents with idiopathic scoliosis: epidemiological study for 43,630 pupils in Niigata City. Japan Eur Spine J 20(2):274–279. https://doi.org/10.1007/s00586-010-1657-6
Segreto FA, Vasquez-Montes D, Brown AE, Bortz C, Horn SR, Diebo BG et al (2018) Incidence, trends, and associated risks of developmental hip dysplasia in patients with early onset and adolescent idiopathic scoliosis. J Orthop 15(3):874–877. https://doi.org/10.1016/j.jor.2018.08.015
Sun J, Chhabra A, Thakur U, Vazquez L, Xi Y, Wells J (2021) The association of lumbosacral transitional vertebral anomalies with acetabular dysplasia in adult patients with hip-spine syndrome : a cross-sectional evaluation of a prospective hip registry cohort. Bone Jt J 103(B8):1351–1357. https://doi.org/10.1302/0301-620X.103B8.BJJ-2020-2481.R1
Talmage MS, Nielson AN, Heflin JA, D’Astous JL, Fedorak GT (2020) Prevalence of hip dysplasia and associated conditions in children treated for idiopathic early-onset scoliosis-don’t just look at the spine. J Pediatr Orthop 40(1):e49–e52. https://doi.org/10.1097/BPO.0000000000001390
Theroux J, Stomski N, Hodgetts CJ, Ballard A, Khadra C, Le May S et al (2017) Prevalence of low back pain in adolescents with idiopathic scoliosis: a systematic review. Chiropr Man Ther 25:10. https://doi.org/10.1186/s12998-017-0143-1
Wen JX, Yang HH, Han SM, Cao L, Wu HZ, Yang C et al (2022) Trunk balance, head posture and plantar pressure in adolescent idiopathic scoliosis. Front Pediatr 10:979816. https://doi.org/10.3389/fped.2022.979816
Yu Y, Song K, Wu B, Chi P, Liu J, Wang Z et al (2021) Coronal compensation mechanism of pelvic obliquity in patients with developmental dysplasia of the hip. Global Spine J 13:949–953. https://doi.org/10.1177/21925682211010760
Zhang G, Li M, Qian H, Wang X, Dang X, Liu R (2022) Coronal and sagittal spinopelvic alignment in the patients with unilateral developmental dysplasia of the hip: a prospective study. Eur J Med Res 27(1):160. https://doi.org/10.1186/s40001-022-00786-w
Acknowledgements
No funding was received for the conduct of this study. And all authors declare that they have no competing interest.
Author information
Authors and Affiliations
Contributions
XZ studied the design, collected the data, statistics and draft. AP collected the data and modified the manuscript. YH did study design, decision maker and manuscript modification.
Corresponding author
Ethics declarations
Conflict of interest
All authors have disclosed that they have no financial or personal relationships that could be construed as a potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhao, X., Pan, A. & Hai, Y. Greater pelvic obliquity in adolescent idiopathic scoliosis combined with hip dysplasia. Eur Spine J 33, 680–686 (2024). https://doi.org/10.1007/s00586-023-08055-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-08055-y