Abstract
Objective
It is unknown whether presence of pre-operative objective functional impairment (OFI) can predict post-operative outcomes in patients with lumbar disc herniation (LDH). We aimed to determine whether pre-operative OFI measured by the five-repetition sit-to-stand test (5R-STS) could predict outcomes at 12-months post-discectomy.
Methods
Adult patients with LDH scheduled for surgery were prospectively recruited from a Dutch short-stay spinal clinic. The 5R-STS time and patient reported outcome measures (PROMs) including Oswestry Disability Index, Roland-Morris Disability Questionnaire, Visual Analogue Scale (VAS) for back and leg pain, EQ-5D-3L health-related quality of life, EQ5D-VAS and ability to work were recorded pre-operatively and at 12-months. A 5R-STS time cut-off of ≥ 10.5 s was used to determine OFI. Mann–Whitney and Chi-square tests were employed to determine significant differences in post-operative outcomes between groups stratified by presence of pre-operative OFI.
Results
We recruited 134 patients in a prospective study. Twelve-month follow-up was completed by 103 (76.8%) patients. Mean age was 53.2 ± 14.35 years and 50 (48.5%) patients were female. Pre-operatively, 53 (51.5%) patients had OFI and 50 (48.5%) did not. Post-operatively, patients with OFI experienced a significantly greater mean change (p < 0.001) across all PROMs compared to patients without OFI, except leg pain (p = 0.176). There were no significant differences in absolute PROMs between groups at 12-months (all p > 0.05).
Conclusions
The presence of OFI based on 5R-STS time does not appear to decrease a patient’s likelihood of experiencing satisfactory post-operative outcomes. The 5R-STS cannot predict how a patient with LDH will respond to surgery at 12-month follow-up.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patient-reported outcome measures (PROMs) continue to be a gold-standard during assessment of patients with lumbar disc herniation (LDH) [1,2,3,4]. However, in recent years there has been a shift towards additional implementation of tests of objective functional impairment (OFI), such as Timed-Up-and-Go test or Motorized Treadmill Test (MTT) [5]. Due to their straight-forwardness, short completion time, objectivity, patient preference and their ability to account for symptoms such as foot drop (commonly missed by PROMs), they are an important addition to the clinical setting of lumbar spine-surgery, creating a new dimension of pre-operative assessment [5,6,7,8].
To overcome the restrictions of OFI tests involving the need for space and time as seen in six-minute walk test or specialized equipment during MTT, the five-repetition sit-to-stand test (5R-STS) has been introduced to the field of spinal surgery [9,10,11]. Its practicality is linked to relatively quick calculation of the time it takes for a patient to perform five consecutive sitting-to-standing movements [12].
Given how advantageous tests of OFI such as 5R-STS appear to be during assessment in patients with LDH, one can question whether they can also determine patients post-operative outcomes as seen with PROMs [13]. If baseline 5R-STS measurement can predict post-operative outcomes in patients with LDH, it can potentially aid in treatment decision-making and management of patients’ expectations.
Therefore, we carried out a prospective study to determine whether the presence of pre-operative OFI measured by 5R-STS influences post-operative outcomes of patients with LDH at 12-month follow-up.
Materials and methods
Study design and oversight
In this prospective cohort study carried out between November 2020 and May 2022, patients were seen at a Dutch specialized short-stay spine surgery clinic pre-operatively and at 12-month post-operatively. The study (ClinicalTrials.gov Identifier: NCT04660656) was approved by the local institutional review board (Medical Research Ethics Committees United, Registration Number: W17.107 and W17.134) and was conducted according to the Declaration of Helsinki and its later amendments. Informed consent was obtained from all participants.
Study population
All enrolled patients underwent tubular microdiscectomy as described previously [14] and were assessed during outpatient consultations. Inclusion criteria were presence of LDH requiring surgical treatment. Patients who were bedridden, pregnant, had hip or knee prosthetics or required walking aides were excluded.
Testing protocol
The test was performed according to the protocol described by Jones et al. [12] If the patient was unable to perform the test in 30 s, or not at all, this was noted down and the test score was recorded as 30 s. The previously described cut-off of ≥ 10.5 s was used to describe patients as objectively functionally impaired according to their pre operative 5R-STS time [9] Based on the baseline severity stratification (BSS) of 5R-STS previously published by Staartjes et al. patients were additionally categorized by their levels of OFI (none, ≤ 10.4 s; mild, 10.5–15.2 s; moderate, 15.3–22.0 s; and severe, > 22.0 s) [9].
Outcome measures
After performing the 5R-STS at pre-operative assessment, patients were asked to complete questionnaires containing baseline sociodemographic data (age, gender, body mass index (BMI), height, weight, smoking status, education level, level of spinal pathology, site of surgery, analgesia use, history of pain, work situation, ability to work), as well as PROMs: VAS for back and leg pain severity, validated Dutch versions of ODI, Roland–Morris Disability Questionnaire (RMDQ), and EQ-5D-3L questionnaire—containing the EQ visual analogue scale (EQ-VAS)—to capture pain, subjective functional impairment, and health-related quality of life. At 12-month post-operative follow-up patients were asked to perform 5R-STS and complete the aforementioned PROMs again including “ability to work” section. Every assessment was performed in the outpatient clinic by the same examiner. We did not refer any patients to a physiotherapy or rehabilitation programme postoperatively.
Statistical analysis
Continuous variables are reported as mean ± standard deviation, and categorical variables as numbers and percentages. Mann–Whitney tests were used to assess the intergroup differences in continuous data. The Chi-square test with Yates correction was chosen for categorical data at baseline. To compare the change in categorical outcomes from baseline to 12-months among patients with and without OFI, ordinal logistic regression adjusted for the baseline measurement was used with continuity correction where applicable. As a sensitivity analysis, we also compared outcomes of patients with different levels of OFI according to BSS using Kruskal–Wallis test and Chi-square test. Complete-case analysis was performed, and patients with missing outcome data were excluded. All analyses were carried out using R version 1.4.1003 (The R Foundation for Statistical Computing, Vienna Austria) [15]. A 2-tailed p ≤ 0.05 was considered significant. The statistical code is provided (Supplementary Content 2).
Results
Overview
The study recruited 134 patients. Thirty-one patients were excluded from the final analysis (Fig. 1). Thirty (22.3%) patients were lost to follow-up and one (0.7%) patient could not perform the test 12-months post-operatively due to advanced pregnancy. Overall, 103 patients were analyzed. Baseline patient demographics are presented in Table 1. The mean age of participants was 53.2 ± 14.35 years.
Pre-operative
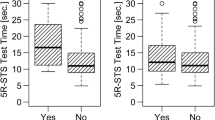
Based on the pre-operative 5R-STS time, 53 (51.5%) patients had OFI. Patients with OFI had significantly higher 5R-STS time compared to patients without OFI (18.6 ± 6.9 s vs. 8.17 ± 1.4 s, p < 0.001). In the OFI group, 27 (51.0%) patients reported presence of anxiety & depression symptoms measured by EQ5D-3L, which was significantly more than in the no-OFI group, where there were 13 (26.0%) of such patients (p = 0.024).
Post-operative
At 12-month follow-up, patients with pre-operative OFI still performed the 5R-STS time slower compared to patients with no pre-operative OFI (10.9 ± 3.6 s vs. 7.8 ± 1.8 s, p < 0.001) (Table 2). Among absolute scores at 12-months, only the 5R-STS time was significantly different between groups (OFI 10.9 ± 3.6 s vs. no-OFI 7.8 ± 1.8 s, p < 0.001). Post-operatively, 102 patients (99.0%) denied presence of anxiety and depression and there were no significant differences in mood symptoms between groups (p = 1.00) (Fig. 2). Patients with pre-operative OFI experienced a significantly greater change in PROMs at 12-months compared to patients without pre-operative OFI, except VAS Leg (− 6.6 ± 2.5 vs. − 6.0 ± 2.4, p = 0.176).
Sensitivity analysis according to OFI BSS
Results are reported in Supplementary Content 1. There were no statistically significant differences between absolute PROMs scores of different OFI groups at 12-months. Stratification of patients based on their level of pre-operative OFI identified that there were statistically significant changes in PROMs between no, mild, moderate, and severe OFI groups at 12-months, except VAS Leg (no OFI 6.0 ± 2.39, mild OFI 6.5 ± 2.4, moderate OFI 6.4 ± 2.9, severe OFI 7.1 ± 2.1, p = 0.494).
Subgroup analysis
Subgroup analyses were performed to identify predictive value of 5R-STS in patients with LDH according to predominant site of pain at presentation (predominant or equal leg or back pain), history of previous spine surgery and patients with chronic pain (> 3 months) (Supplementary Table 3, 4, 5, 6, 7 and 8).
Discussion
In our prospective cohort study of patients with LDH, individuals with pre-operative OFI as per their 5R-STS time experienced significantly greater improvement in 5R-STS performance, ODI, RMDQ, VAS Back, and EQ5D-VAS at 12-month post-surgery compared to individuals with no pre-operative OFI. However, the overall post-operative absolute PROMs score did not differ significantly across groups, demonstrating that 5R-STS at baseline cannot predict 12-month outcomes.
Although it was hypothesized that patients with pre-operative OFI would have significantly different post-operative outcomes as measured by PROMs compared to their not objectively functionally impaired counterparts, findings in our study contradict that. It is known that surgery can successfully reverse the disability associated with LDH, and it appears that patients with motor deficits may achieve as good post-operative outcomes as if they were not present, even when stratified by different level of OFI as seen in our sensitivity analysis [16]. This information is reassuring for both the surgical team and the patient during consultation [17]. As seen in our study, patients who report worse functionality and pain scores pre-operatively, are sometimes theorized to “have more room for improvement” and hence are more likely to experience an overall higher satisfaction with post-operative outcomes [18, 19]. This can aid in management of patients’ expectations–crucial in the spinal surgery setting as positive expectations appear to be linked to better post-operative PROMs [20, 21].
Interestingly, at 12-month follow-up, patients with pre-operative OFI still performed the 5R-STS slower than patients with no pre-operative OFI, yet in both groups the absolute PROMs at 12-months were not significantly different. Ongoing presence of degree of OFI does not appear to necessarily constitute poor post-operative outcomes. It can be concluded that in the absence of pain, the ongoing OFI is no longer burdensome, and patients can cope with it sufficiently to achieve a satisfactory quality of life.
Nearly all PROMs except VAS Leg differed among patients with OFI vs. no OFI, a pattern seen also in our sensitivity analysis. This agrees with a previous study validating the proposed OFI baseline severity stratification of 5R-STS in patients with lumbar degenerative disease, where again, severity of VAS Leg was not associated with advancement of OFI [10]. This further implies that there may exist a subgroup of patients with LDH with a motor component independent of leg pain that is not captured by commonly used PROMs but is potentially identifiable by the 5R-STS [22].
Although the 5R-STS in itself does not appear to predict post-microdiscectomy outcomes, it complements the pre-operative consultation through an objective assessment of functionality and provides a reference point for analyzing post-surgical recovery and outcomes in both clinical and research setting. The 5R-STS was also shown to be reliable when performed at home by patients [11]. This has created an opportunity for patients to not only monitor their self-improvement but better surgeons’ assessment during telephone consultations that have increased in popularity especially since the SARS-CoV-2 pandemic [23].
The 5R-STS as shown above adds a new objective dimension in the assessment of patients with LDH, but on its own, it cannot predict patients’ post-microdiscectomy outcomes. Findings in our study can, however, reassure the patient that despite presence of OFI, they can still achieve satisfactory results after surgery, and they are not disadvantaged. The 5R-STS appears to have the potential to detect a motor component of LDH independent of leg pain and is a validated tool for assessment and monitoring of patients with LDH in both clinical and research setting.
Limitations
As all our patients were diagnosed with LDH, findings in our study are disease-specific and should not be applied to all diagnoses of lumbar degenerative disease.
In this prospective cohort study, 103 (76.9%) patients out of 134 recruited were followed up at 12-months. This may have introduced attrition bias due to unassessed outcomes in a subgroup of patients which may have impacted the results.
As our data was collected at one specialized Dutch short-stay spinal clinic, findings have limited generalizability in other countries. Populations from different areas may require adjusted outcome measures as seen with EQ-5D or 6MWT [24, 25]. Future studies are encouraged to differentiate between nationalities and ethnicities.
Finally, presence of chronic conditions in patients was not clearly reported. This may have led to overestimation of the impact of LDH on the 5R-STS performance and underestimation of the perceived improvement from the surgery due to ongoing burden of other illnesses. However, our inclusion criteria did not allow to analyze patients whose mobility was markedly affected by chronic comorbidities.
Conclusions
Although at 12-months there were no significant differences in absolute post-operative scores between patients with pre-operative OFI and no OFI, patients with pre-operative OFI experienced a greater improvement in PROM scores. It can be concluded that presence of OFI based on 5R-STS time does not decrease a patient’s likelihood of experiencing satisfactory post-operative outcomes. The 5R-STS cannot predict how a patient with LDH will respond to surgery at 12-month follow-up. The 5R-STS continues to remain an effective tool to assess disease severity of patients with LDH with excellent concurrent validity with PROMs. It can be used in both research setting as an outcome measure to determine treatment effectiveness as well as in clinical setting to complement pre-operative assessment and monitor post-operative recovery.
References
Fairbank JC, Couper J, Davies JB, O’Brien JP (1980) The Oswestry low back pain disability questionnaire. Physiotherapy 66:271–273
Rabin R, de Charro F (2001) EQ-5D: a measure of health status from the EuroQol Group. Ann Med 33:337–343
Roland M, Morris R (1983) A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back pain. Spine 8:141–144
Finkelstein JA, Schwartz CE (2019) Patient-reported outcomes in spine surgery: past, current, and future directions: JNSPG 75th anniversary invited review article. J Neurosurg Spine 31:155–164. https://doi.org/10.3171/2019.1.SPINE18770
Stienen MN, Ho AL, Staartjes VE et al (2019) Objective measures of functional impairment for degenerative diseases of the lumbar spine: a systematic review of the literature. Spine J 19:1276–1293. https://doi.org/10.1016/j.spinee.2019.02.014
Gvozdyev BV, Carreon LY, Graves CM et al (2017) Patient-reported outcome scores underestimate the impact of major complications in patients undergoing spine surgery for degenerative conditions. J Neurosurg Spine 27:397–402. https://doi.org/10.3171/2017.3.SPINE161400
Gautschi OP, Smoll NR, Corniola MV et al (2016) Validity and reliability of a measurement of objective functional impairment in lumbar degenerative disc disease: the timed up and go (TUG) test. Neurosurgery 79:270–278. https://doi.org/10.1227/NEU.0000000000001195
Joswig H, Stienen MN, Smoll NR et al (2017) Patients’ preference of the timed up and go test or patient-reported outcome measures before and after surgery for lumbar degenerative disk disease. World Neurosurg 99:26–30. https://doi.org/10.1016/j.wneu.2016.11.039
Staartjes VE, Schröder ML (2018) The five-repetition sit-to-stand test: evaluation of a simple and objective tool for the assessment of degenerative pathologies of the lumbar spine. J Neurosurg Spine 29:380–387. https://doi.org/10.3171/2018.2.SPINE171416
Klukowska AM, Schröder ML, Stienen MN, Staartjes VE (2020) Objective functional impairment in lumbar degenerative disease: concurrent validity of the baseline severity stratification for the five-repetition sit-to-stand test. J Neurosurg Spine 33(1):1–8. https://doi.org/10.3171/2019.12.SPINE191124
Staartjes VE, Beusekamp F, Schröder ML (2019) Can objective functional impairment in lumbar degenerative disease be reliably assessed at home using the five-repetition sit-to-stand test? A prospective study. Eur Spine J 28:665–673. https://doi.org/10.1007/s00586-019-05897-3
Jones SE, Kon SSC, Canavan JL et al (2013) The five-repetition sit-to-stand test as a functional outcome measure in COPD. Thorax 68:1015–1020. https://doi.org/10.1136/thoraxjnl-2013-203576
Nerland US, Jakola AS, Giannadakis C et al (2015) The risk of getting worse: predictors of deterioration after decompressive surgery for lumbar spinal stenosis: a multicenter observational study. World Neurosurg 84:1095–1102. https://doi.org/10.1016/j.wneu.2015.05.055
Staartjes VE, de Wispelaere MP, Miedema J, Schröder ML (2017) Recurrent lumbar disc herniation after tubular microdiscectomy: analysis of learning curve progression. World Neurosurg 107:28–34. https://doi.org/10.1016/j.wneu.2017.07.121
R Core Team (2023) R: a language and environment for statistical computing
Ravindra VM, Senglaub SS, Rattani A et al (2018) Degenerative lumbar spine disease: estimating global incidence and worldwide volume. Glob Spine J 8:784–794. https://doi.org/10.1177/2192568218770769
Hébert JJ, Abraham E, Wedderkopp N et al (2020) Preoperative factors predict postoperative trajectories of pain and disability following surgery for degenerative lumbar spinal stenosis. Spine 45:E1421–E1430. https://doi.org/10.1097/BRS.0000000000003587
Rampersaud YR, Canizares M, Perruccio AV et al (2022) Fulfillment of patient expectations after spine surgery is critical to patient satisfaction: a cohort study of spine surgery patients. Neurosurgery 91:173–181. https://doi.org/10.1227/neu.0000000000001981
Mannion AF, Junge A, Elfering A et al (2009) Great expectations: Really the novel predictor of outcome after spinal surgery? Spine 34:1590. https://doi.org/10.1097/BRS.0b013e31819fcd52
Waljee J, McGlinn EP, Sears ED, Chung KC (2014) Patient expectations and patient-reported outcomes in surgery: a systematic review. Surgery 155:799–808. https://doi.org/10.1016/j.surg.2013.12.015
Canizares M, Gleenie RA, Perruccio AV et al (2020) Patients’ expectations of spine surgery for degenerative conditions: results from the Canadian spine outcomes and research network (CSORN). The Spine J 20:399–408. https://doi.org/10.1016/j.spinee.2019.10.001
Lipetz JS (2002) Pathophysiology of inflammatory, degenerative, and compressive radiculopathies. Phys Med Rehabilit Clin N Am 13:439–449
Taha A, Saad B, Enodien B et al (2021) The development of telemedicine and eHealth in surgery during the SARS-CoV-2 pandemic. Int J Environ Res Public Health 18:11969. https://doi.org/10.3390/ijerph182211969
Casanova C, Celli BR, Barria P et al (2011) The 6-min walk distance in healthy subjects: reference standards from seven countries. Eur Respir J 37:150–156. https://doi.org/10.1183/09031936.00194909
Lamers LM, McDonnell J, Stalmeier PFM et al (2006) The Dutch tariff: results and arguments for an effective design for national EQ-5D valuation studies. Health Econ 15:1121–1132. https://doi.org/10.1002/hec.1124
Acknowledgements
The authors are grateful to all patients participating in this study and generously sharing their time.
Funding
Open access funding provided by University of Zurich. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that the article and its content were composed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.

Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Klukowska, A.M., Staartjes, V.E., Dol, M. et al. Predictive value of the five-repetition sit-to-stand test for outcomes after surgery for lumbar disc herniation: prospective study. Eur Spine J 33, 956–963 (2024). https://doi.org/10.1007/s00586-023-08046-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-08046-z