Abstract
Purpose
In spine care, frailty is associated with poor outcomes. The aim of this study was to describe changes in frailty in spine care during the coronavirus disease 2019 (COVID-19) pandemic and their relation to surgical management and outcomes.
Methods
Patients hospitalized for spine pathologies between January 1, 2019, and May 17, 2022, within a nationwide network of 76 hospitals in Germany were retrospectively included. Patient frailty, types of surgery, and in-hospital mortality rates were compared between pandemic and pre-pandemic periods.
Results
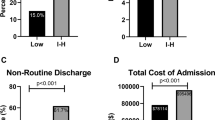
Of the 223,418 included patients with spine pathologies, 151,766 were admitted during the pandemic and 71,652 during corresponding pre-pandemic periods in 2019. During the pandemic, the proportion of high-frailty patients increased from a range of 5.1–6.1% to 6.5–8.8% (p < 0.01), while the proportion of low frailty patients decreased from a range of 70.5–71.4% to 65.5–70.1% (p < 0.01). In most phases of the pandemic, the Elixhauser comorbidity index (ECI) showed larger increases among high compared to low frailty patients (by 0.2–1.8 vs. 0.2–0.8 [p < 0.01]). Changes in rates of spine surgery were associated with frailty, most clearly in rates of spine fusion, showing consistent increases among low frailty patients (by 2.2–2.5%) versus decreases (by 0.3–0.8%) among high-frailty patients (p < 0.02). Changes in rates of in-hospital mortality were not associated with frailty.
Conclusions
During the COVID-19 pandemic, the proportion of high-frailty patients increased among those hospitalized for spine pathologies in Germany. Low frailty was associated with a rise in rates of spine surgery and high frailty with comparably larger increases in rates of comorbidities.


Similar content being viewed by others
Data availability
All data were stored and analyzed in pseudonymized form.
Code availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Cong T, Hall AJ, Jia Z, Christiano A, Elsevier HCK, Cheung ZB, Wellman D, Forsh D, Lane JM (2022) Conceptualizing biological aging and frailty in orthopaedics: a framework for clinical practice. J Bone Joint Surg Am 104:1212–1222. https://doi.org/10.2106/JBJS.21.01053
Lemos JL, Welch JM, Xiao M, Shapiro LM, Adeli E, Kamal RN (2021) Is frailty associated with adverse outcomes after orthopaedic surgery?: a systematic review and assessment of definitions. JBJS Rev. https://doi.org/10.2106/JBJS.RVW.21.00065
Fried LP, Tangen CM, Walston J, A B Newman, C Hirsch, J Gottdiener, T Seeman, R Tracy, W J Kop, G Burke, M A McBurnie, Cardiovascular Health Study Collaborative Research Group (2001) Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 56:M146-156. https://doi.org/10.1093/gerona/56.3.m146
Collard RM, Boter H, Schoevers RA, Oude Voshaar RC (2012) Prevalence of frailty in community-dwelling older persons: a systematic review. J Am Geriatr Soc 60:1487–1492. https://doi.org/10.1111/j.1532-5415.2012.04054.x
Syddall H, Roberts HC, Evandrou M, Cooper C, Bergman H, Aihie Sayer A (2010) Prevalence and correlates of frailty among community-dwelling older men and women: findings from the Hertfordshire Cohort Study. Age Ageing 39:197–203. https://doi.org/10.1093/ageing/afp204
Chan V, Wilson JRF, Ravinsky R, Badhiwala JH, Jiang F, Anderson M, Yee A, Wilson JR, Fehlings MG (2021) Frailty adversely affects outcomes of patients undergoing spine surgery: a systematic review. Spine J 21:988–1000. https://doi.org/10.1016/j.spinee.2021.01.028
Veronesi F, Borsari V, Martini L, Visani A, Gasbarrini A, Brodano GB, Fini M (2021) The impact of frailty on spine surgery: systematic review on 10 years clinical studies. Aging Dis 12:625–645
Laverdière C, Georgiopoulos M, Ames CP, Corban J, Ahangar P, Awadhi K, Weber MH (2022) Adult spinal deformity surgery and frailty: a systematic review. Global Spine J 12:689–699
Passias PG, Brown AE, Bortz C, Pierce K, Alas H, Ahmad W, Passfall L, Kummer N, Krol O, Lafage R, Lafage V, Burton D, Hart R, Anand N, Mundis G, Neuman B, Line B, Shaffrey C, Klineberg E, Smith J, Ames C, Schwab FJ, Bess S; International Spine Study Group (2021) A risk-benefit analysis of increasing surgical invasiveness relative to frailty status in adult spinal deformity surgery. Spine (Phila Pa 1976) 46:1087–1096. https://doi.org/10.1097/BRS.0000000000003977
Gum JL, Yeramaneni S, Wang K, Hostin RA Jr, Kebaish KM, Neuman BJ, Jain A, Kelly MP, Burton DC, Ames CP, Shaffrey CI, Klineberg EO, Kim HJ, Protopsaltis TS, Passias PG, Mundis GM Jr, Eastlack RK, Schwab FJ, Hart RA, Gupta MC, Daniels AH, Smith JS, Lafage V, Line B, Bess S; International Spine Study Group. (2021) Comparison of patient factors (frailty) vs. surgical factors (invasiveness) for optimization of 2-year cost-utility: we should focus on the patient factors. Spine J 21 Suppl:S105. https://doi.org/10.1016/j.spinee.2021.05.413
United Nations, Department of Economic and Social Affairs, Population Division. World population prospects 2019. https://population.un.org/wpp/publications/files/wpp2019_highlights.pdf. Accessed 8 Sept 2022
Kalseth J, Halvorsen T (2020) Health and care service utilisation and cost over the life-span: a descriptive analysis of population data. BMC Health Serv Res 20:435. https://doi.org/10.1186/s12913-020-05295-2
Garner IW, Varey S, Navarro-Pardo E, Marr C, Holland CA (2022) An observational cohort study of longitudinal impacts on frailty and well-being of COVID-19 lockdowns in older adults in England and Spain. Health Soc Care Commun 30:e2905–e2916. https://doi.org/10.1111/hsc.13735
Yamada M, Kimura Y, Ishiyama D, Otobe Y, Suzuki M, Koyama S, Kikuchi T, Kusumi H, Arai H (2021) The influence of the COVID-19 pandemic on physical activity and new incidence of frailty among initially non-frail older adults in Japan: a follow-up online survey. J Nutr Health Aging 25:751–756. https://doi.org/10.1007/s12603-021-1634-2
Gilbert T, Neuburger J, Kraindler J, Keeble E, Smith P, Ariti C, Arora S, Street A, Parker S, Roberts HC, Bardsley M, Conroy S (2018) Development and validation of a Hospital Frailty Risk Score focusing on older people in acute care settings using electronic hospital records: an observational study. Lancet 391:1775–1782. https://doi.org/10.1016/S0140-6736(18)30668-8
Hannah TC, Neifert SN, Caridi JM, Martini ML, Lamb C, Rothrock RJ, Yuk FJ, Gilligan J, Genadry L, Gal JS (2020) Utility of the hospital frailty risk score for predicting adverse outcomes in degenerative spine surgery cohorts. Neurosurgery 87:1223–1230. https://doi.org/10.1093/neuros/nyaa248
Pulido LC, Meyer M, Reinhard J, Kappenschneider T, Grifka J, Weber M (2022) Hospital frailty risk score predicts adverse events in spine surgery. Eur Spine J 31:1621–1629. https://doi.org/10.1007/s00586-022-07211-0
Elsamadicy AA, Koo AB, Sarkozy M, David WB, Reeves BC, Patel S, Hansen J, Sandhu MRS, Hengartner AC, Hersh A, Kolb L, Lo SL, Shin JH, Mendel E, Sciubba DM (2022) Leveraging HFRS to assess how frailty affects healthcare resource utilization after Elective ACDF for CSM. Spine J S1529–9430(22):00845–00852. https://doi.org/10.1016/j.spinee.2022.08.004
Kilkenny MF, Phan HT, Lindley RI, Kim J, Lopez D, Dalli LL, Grimley R, Sundararajan V, Thrift AG, Andrew NE, Donnan GA, Cadilhac DA; Stroke123 Investigators and the AuSCR Consortium (2021) Utility of the hospital frailty risk score derived from administrative data and the association with stroke outcomes. Stroke 52:2874–2881. https://doi.org/10.1161/STROKEAHA.120.033648
Subramaniam A, Ueno R, Tiruvoipati R, Srikanth V, Bailey M, Pilcher D (2022) Comparison of the predictive ability of clinical frailty scale and hospital frailty risk score to determine long-term survival in critically ill patients: a multicentre retrospective cohort study. Crit Care 26:121. https://doi.org/10.1186/s13054-022-03987-1
Nachtigall I, Lenga P, Jóźwiak K, Thürmann P, Meier-Hellmann A, Kuhlen R, Brederlau J, Bauer T, Tebbenjohanns J, Schwegmann K, Hauptmann M, Dengler J (2020) Clinical course and factors associated with outcomes among 1904 patients hospitalized with COVID-19 in Germany: an observational study. Clin Microbiol Infect 26:1663–1669. https://doi.org/10.1016/j.cmi.2020.08.011
Dengler J, Prass K, Palm F, Hohenstein S, Pellisier V, Stoffel M, Hong B, Meier-Hellmann A, Kuhlen R, Bollmann A, Rosahl S (2022) Changes in nationwide in-hospital stroke care during the first four waves of COVID-19 in Germany. Eur Stroke J 7:166–174. https://doi.org/10.1177/23969873221089152
Abduljawwad N, Pamnani S, Stoffel M, Kraft CN, Hegewald AA, Dörre R, Heese O, Gerlach R, Rosahl S, Maier B, Burger R, Wutzler S, Carl B, Ryang YM, Hau KT, Stein G, Gulow J, Kuhlen R, Hohenstein S, Bollmann A, Dengler J (2023) Effects of the COVID-19 pandemic on spinal fusion procedures for spinal infections in a nationwide hospital network in Germany. J Neurol Surg A Cent Eur Neurosurg 84:58–64. https://doi.org/10.1055/s-0042-1749353
Moore BJ, White S, Washington R, Coenen N, Elixhauser A (2017) Identifying increased risk of readmission and in-hospital mortality using hospital administrative data: the AHRQ Elixhauser comorbitiy index. Med Care 55:698–705. https://doi.org/10.1097/MLR.0000000000000735
Kane AE, Howlett SE (2021) Sex differences in frailty: Comparisons between humans and preclinical models. Mech Ageing Dev 198:111546. https://doi.org/10.1016/j.mad.2021.111546
Lekan DA, McCoy TP, Jenkins M, Mohanty S, Manda P, Yasin R (2021) Comparison of a frailty risk score and comorbidity indices for hospital readmission using electronic health record data. Res Gerontol Nurs 14:91–103. https://doi.org/10.3928/19404921-20210115-03
Baayen RH, Davidson DJ, Bates DM (2008) Mixed-effects modeling with crossed random effects for subjects and items. J Mem Lang 59:390–412. https://doi.org/10.1016/j.jml.2007.12.005
Kliegl R, Masson MEJ, Richter EM (2010) A linear mixed model analysis of masked repetition priming. Vis Cogn 18:655–681. https://doi.org/10.1080/13506280902986058
Bates D, Mächler M, Bolker B, Walker S (2015) Fitting linear mixed-effects models using lme4. J Stat Softw 67:1–48. https://doi.org/10.18637/jss.v067.i01
R Core Team (2020) A language and environment for statistical computing. R Foundation for statistical computing. Vienna, Austria
Haffer H, Schömig F, Rickert M, Randau T, Raschke M, Wirtz D, Pumberger M, Perka C (2020) Impact of the COVID-19 pandemic on orthopaedic and trauma surgery in university hospitals in germany: results of a nationwide survey. J Bone Joint Surg Am 102:e78. https://doi.org/10.2106/JBJS.20.00756
Soh TLT, Ho SWL, Yap WMQ, Oh JY (2020) Spine Surgery and COVID-19: Challenges and Strategies from the Front Lines. J Bone Joint Surg Am 102:e56. https://doi.org/10.2106/JBJS.20.00503
Power FR, Juhdi A, Macken M, Synnott KA, Butler JS (2022) The Impact of COVID-19 and lockdown on spinal services at a national level: lessons learned and areas of service improvement for future health care delivery. Clin Spine Surg 35:7–11. https://doi.org/10.1097/BSD.0000000000001261
Arnold PM, Owens L, Heary RF, Webb AG, Whiting MD, Vaccaro AR, Iyer RK, Harrop JS (2021) Lumbar spine surgery and what we lost in the era of the coronavirus pandemic: a survey of the lumbar spine research society. Clin Spine Surg 34:E575-579. https://doi.org/10.1097/BSD.0000000000001235
Abramovic A, Lener S, Grassner L, Thaler M, Pinggera D, Freyschlag CF, Thomé C, Hartmann S (2021) The impact of the COVID-19 pandemic on spine surgery in central Europe: a questionnaire-based study. World Neurosurg 155:e576-587. https://doi.org/10.1016/j.wneu.2021.08.106
Sablerolles RSG, Lafeber M, van Kempen JAL, van de Loo BPA, Boersma E, Rietdijk WJR et al (2021) Association between clinical frailty scale score and hospital mortality in adult patients with COVID-19 (COMET): an international, multicentre, retrospective, observational cohort study. Lancet Healthy Longev 2:e163–e170. https://doi.org/10.1016/S2666-7568(21)00006-4
Zhang XM, Jiao J, Cao J, Huo XP, Zhu C, Wu XJ, Xie XH /2021) Frailty as a predictor of mortality among patients with COVID-19: a systematic review and meta-analysis. BMC Geriatr 21:186. https://doi.org/10.1186/s12877-021-02138-5
Sealy MJ, van der Lucht F, van Munster BC, Krijnen WP, Hobbelen H, Barf HA, Finnema EJ, Jager-Wittenaar H (2022) Frailty among Older People during the First Wave of the COVID-19 Pandemic in The Netherlands. Int J Environ Res Public Health 19:3669. https://doi.org/10.3390/ijerph19063669
Robert Koch Institute; Digitales Impfquotenmonitoring zur COVID-19-Impfung. https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Daten/Impfquoten-Tab.htm. Accessed 14 Nov 2021
Ljungqvist O, Scott M, Fearon KC (2017) Enhanced recovery after surgery: a review. JAMA Surg 152:292–298. https://doi.org/10.1001/jamasurg.2016.4952
Porche K, Yan S, Mohamed B, Garvan C, Samra R, Melnick K, Vaziri S, Seubert C, Decker M, Polifka A, Hoh DJ (2022) Enhanced recovery after surgery (ERAS) improves return of physiological function in frail patients undergoing one- to two-level TLIFs: an observational retrospective cohort study. Spine J 22:1513–1522. https://doi.org/10.1016/j.spinee.2022.04.007
Grieco M, Galiffa G, Marcellinaro R, Santoro E, Persiani R, Mancini S, Di Paola M, Santoro R, Stipa F, Crucitti A, Carlini M, “Lazio Network” study group, (2022) Impact of the COVID-19 Pandemic on Enhanced Recovery After Surgery (ERAS) Application and Outcomes: Analysis in the “Lazio Network” Database. World J Surg 46:2288–2296. https://doi.org/10.1007/s00268-022-06694-8
Tan L, Peng D, Cheng Y. Enhanced Recovery After Surgery Is Still Powerful for Colorectal Cancer Patients in COVID-19 Era. J Laparoendosc Adv Surg Tech A 33:257–262. https://doi.org/10.1089/lap.2022.0393
Prodromidou A, Koulakmanidis AM, Haidopoulos D, Nelson G, Rodolakis A, Thomakos N /2022) Where Enhanced Recovery after Surgery (ERAS) Protocols Meet the Three Major Current Pandemics: COVID-19, Obesity and Malignancy. Cancers (Basel) 14:1660 https://doi.org/10.3390/cancers14071660
Partridge JSL, Harari D, Martin FC, Peacock JL, Bell R, Mohammed A, Dhesi JK (2017) Randomized clinical trial of comprehensive geriatric assessment and optimization in vascular surgery. Br J Surg 104:679–687. https://doi.org/10.1002/bjs.10459
Hall DE, Arya S, Schmid KK, Carlson MA, Lavedan P, Bailey TL, Purviance G, Bockman T, Lynch TG, Johanning JM (2017) Association of a frailty screening initiative with postoperative survival at 30, 180, and 365 days. JAMA Surg 152:233–240. https://doi.org/10.1001/jamasurg.2016.4219
Funding
This study was funded by the Helios Center for Research and Innovation via a grant (HCRI ID 2021–0431) to JD.
Author information
Authors and Affiliations
Contributions
JD and MS conceived the study, wrote the first draft of the manuscript, and were involved in data interpretation. JD, HG, CNK, AAH, RD, OH, RG, SR, BM, RB, SW, BC, YR, KTH, GS, JG, AA, NA, GRG, and MS were involved in the collection of data. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interests
JD received funding through the Helios Center for Research and Innovation via a grant (HCRI ID 2020–0458). RK holds shares in Fresenius AG. YR is a member of the DWG Advisory Board for the journal “Die Wirbelsäule, DWG Commissions (Science, Education, Quality Safety, Congress Program), and Eurospine EduCom.” All other authors declare no conflict of interest.
Ethics approval
The study was approved by the ethics committee of the University of Leipzig on February 07, 2022 (490/20-ek).
Informed consent
Informed consent was waived due to the retrospective design of this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dengler, J., Gheewala, H., Kraft, C.N. et al. Changes in frailty among patients hospitalized for spine pathologies during the COVID-19 pandemic in Germany—a nationwide observational study. Eur Spine J 33, 19–30 (2024). https://doi.org/10.1007/s00586-023-08014-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-08014-7