Abstract
Objective
Dorsal instrumentation using pedicle screws is a standard treatment for multiple spinal pathologies, such as trauma, infection, or degenerative indications. Intraoperative three-dimensional (3D) imaging and navigated pedicle screw placement are used at multiple centers. For the present study, we evaluated a new navigation system enabling augmented reality (AR)-supported pedicle screw placement while integrating navigation cameras into the reference array and drill guide. The present study aimed to evaluate its clinical application regarding safety, efficacy, and accuracy.
Methods
A total of 20 patients were operated on between 06/2021 and 01/2022 using the new technique for intraoperative navigation. Intraoperative data with a focus on accuracy and patient safety, including patient outcome, were analyzed. The accuracy of pedicle screw placement was evaluated by intraoperative CT imaging.
Results
A median of 8 (4–18) pedicle screws were placed in each case. Percutaneous instrumentation was performed in 14 patients (70%). The duration of pedicle screw placement (duration scan–scan) was 56 ± 26 (30–107) min. Intraoperative screw revision was necessary for 3 of 180 pedicle screws (1.7%). Intraoperatively, no major complications occurred—one case of delay due to software issues and one case of difficult screw placement were reported.
Conclusion
The current study's results could confirm the use of the present AR-supported system for navigated pedicle screw placement for dorsal instrumentation in clinical routine. It provides a reliable and safe tool for 3D imaging-based pedicle screw placement, only requires a minimal intraoperative setup, and provides new opportunities by integrating AR.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In spine surgery, dorsal instrumentation using pedicle screws is a standard treatment for multiple spinal pathologies, such as trauma, infection, or degenerative indications, especially of the thoracolumbar spine [1,2,3,4,5]. Numerous studies, including systematic reviews and meta-analyses, have shown that intraoperative computed tomography (CT)—navigated screw placement is superior to screw placement using free-hand technique or 2-D fluoroscopy regarding screw positioning and patient safety [6,7,8,9,10].
Multiple imaging solutions, especially for mobile cone beam CT-based approaches but also for portable CT scanners, exist mainly differing regarding imaging quality, the field of view (FOV), acquisition and running costs, and not at least, their compatibility with navigation platforms [11]. Recently, a comprehensive review of assistive active and passive technologies summarizing current tools for spine surgery recommended the acquisition of devices with maximum compatibility and universal registration mechanisms [12]. As development has proceeded for intraoperative imaging, the same has occurred for intraoperative navigation, including augmented reality for spinal instrumentation [13,14,15,16,17,18,19,20].
For the present study, we evaluated a new navigation system enabling augmented reality (AR)-supported pedicle screw placement while integrating navigation cameras into the surgical instruments. Similarly to other systems, this system for spinal navigation is based on intraoperative 3D imaging. However, the setup is reduced by integrating navigation targets into the reference array and infrared camera into surgical instruments, establishing a flexible platform, including preoperative planning.
This study aimed to analyze the clinical application of this navigation system regarding safety, efficacy, and accuracy.
Methods
Ethics
The local ethics board approved the study (registration number: 2022-306-S-NP). The study was performed in accordance with the Declaration of Helsinki and in accordance to the STROBE statement.
Patients
Patients scheduled for dorsal instrumentation between June 2021 and January 2022 were considered eligible for this pilot study. Inclusion criteria were patients undergoing navigated pedicle screw placement of the thoracic and lumbar spine at our institution using the new navigation system (NextAR TS [Tracking System], Medacta, Castel San Pietro, Switzerland) enabling AR-supported pedicle screw placement.
Intraoperative procedures
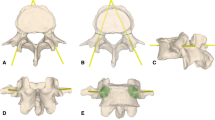
An open midline approach or percutaneous pedicle screw implantation was performed depending on the additional need for decompression, construct length, and instrumentation levels. For spinal navigation, a reference array equipped with navigation targets incorporating multiple light emitting diodes (LEDs) in a certain spatial configuration was attached to a spinous process close to the levels planned for instrumentation, and an infrared camera was firmly attached to surgical instruments such as the drill guide (Fig. 1). Next, a navigation scan was performed using either a 3D C-arm scanner (Vision, Ziehm Imaging, Nuremberg, Germany) or an operation room-based CT scanner (ORCT) (Brilliance CT Big Bore, Philips, Amsterdam, Netherlands). During image acquisition, the surgery staff was outside the operation room to reduce radiation exposure. After uploading the navigation data set to the navigation software, the image quality, as well as the accuracy of the registration in correlation with anatomical structures, were reviewed. Under the use of the AR-supported navigation system, skin incisions for percutaneous instrumentation, screw entry points, and screw trajectories were planned using a navigated drill guide (Figs. 1, 2). The planned trajectory was drilled using a battery-powered drill, and a Kirschner wire was inserted via the drill guide to mark the screw trajectory. In the next step, cannulated pedicle screws (Medacta Universal Screw Technology [MUST], Medacta, Castel San Pietro, Switzerland) were implanted by passing them over the Kirschner wires. After implantation of all pedicle screws, a final control scan was acquired. Pedicle screw placement was then reviewed on 3D imaging. In case of screw revision, another final scan was performed. Afterward, rods were fitted regarding curvature and length and installed by fixating the pedicle screw nuts. Additional decompression was performed, depending on the indication of surgery.
Intraoperative Setup. Figure 1 represents the setup of the system during navigated pedicle screw placement. The navigation system consists of targets (1), which are battery-powered devices incorporating multiple LEDs in a known spatial configuration allowing for three-dimensional navigation and attached to the reference array (2) and infrared cameras (3) firmly attached to surgical instruments, such as the navigated drill guide (4) shown in this figure
Intraoperative visualization for navigated pedicle screw placement. Figure 2 illustrates the visualization of intraoperative neuronavigation as displayed through the surgeons (A) AR-goggle (B) and on the main screen (C) as used for K-wire placement. The navigated drill guide is represented in green color, and the planned trajectory is shown in pink. The fact that the surgeons’ view has not been averted from the situs has been rated advantageously
Data acquisition
Surgical data, including perioperative data, accuracy of screw placement on 3D intraoperative imaging, and screw revision rates were acquired for all patients undergoing AR-supported pedicle screw placement during the analyzed period. Furthermore, we analyzed data on intra- and postoperative complication rates and additional surgeries.
Radiation dose analysis
Intraoperatively, 3D radiographs were acquired before and after pedicle screw placement. The accuracy was rated on intraoperative imaging according to the Gertzbein and Robbins classification system (GRS) (Grade A = 0 mm breach distance, B = < 2 mm, C = < 4 mm, D = < 6 mm, E > 6 mm) [21]. In addition, screw placement was evaluated intraoperatively into sufficient (= intraoperative evaluation as solid + no neurological compression suspected—usually GRS grade A + B + C) and insufficient (= requiring screw revision) [11].
Data analysis
Statistical analyses were performed using Prism (version 8.4.1; GraphPad Software, La Jolla, CA, USA). Descriptive statistics, including mean, median, minimum, maximum, and standard deviation, were calculated for patient- and surgery-related characteristics including radiation dose analysis.
Results
Patient characteristics
Twenty consecutive patients (10 women, 10 men) aged 69.4 ± 12.0 (32.1–88.0) years were included in this study and analyzed (Table 1). A median of 4 (1–11) segments were instrumented. Indications for surgical treatment were trauma, including ankylosing spondylitis and osteoporotic fractures in 12 cases (60%), degenerative spinal disease in 6 cases (30%), and infection and pathological fractures in one case each (5.0%) (Table 1).
Surgical data
Preoperative scans had to be repeated in three (15.0%) cases due to insufficient imaging quality and inaccuracies. One case (5.0%) of delay during surgery related to intraoperative software issues was reported. Overall, a median (range) of 8 (4–18) pedicle screws were implanted in each patient, summed up to a total of 180 (Table 2). The duration of surgery was 186 ± 68 (106–324) minutes. The time span between skin incision and first intraoperative imaging was 19 ± 11 (9–40) min, with durations of 16 ± 9 (9–40) min for intraoperative CT imaging and 28 ± 11 (13–37) min for 3D C-arm imaging (p = 0.0169). The estimated duration of pedicle screw placement as measured by the difference between the time of the first scan and the time of the final scan (including undraping of the situs and uploading data to the navigation system) was 57 ± 24 (30–107) min, resulting in an estimated duration per screw of 6.5 ± 1.9 (4.0–11.5) min (Table 2). Intraoperatively, three screws (1.7%) had to be revised. In 14 (70.0%) surgeries, pedicle screw placement was performed percutaneously (Table 2). Cement augmentation of screws was performed in ten cases (50.0%) (Table 2). Revision surgery was necessary in one (5.0%) case due to a dislocation of two pedicle screw nuts. Lateral instrumentation was additionally performed in ten (50.0%) cases, with nine cases of vertebral body replacement and one case of implantation of intervertebral cages.
Clinical outcome
Navigated pedicle screw placement was successfully performed in all cases. No patient developed new neurological deficits postoperatively. Regarding pedicle screw placement, postoperative surgery-related complications were reported in three cases (15.0%) (Suppl. Table 1). Apart from the loosening of pedicle screw nuts in one patient, one patient developed a wound seroma postoperatively, and one patient showed cement embolism after cementation of pedicle screws (Suppl. Table 1). Non-surgical postoperative complications are further listed in Suppl. Table 1.
Radiological outcome
The initial pedicle screw placement, as analyzed in accordance with the GRS was Grade A for 116 PS (64.4%), B for 47 PS (26.1%), C for 14 PS (7.8%), D for two PS (1.1%), and E for one PS (0.6%) (Fig. 3).
Radiographic evaluation of pedicle screw placement. This figure lines up the rating of all 180 pedicle screw placements on intraoperative imaging according to the Gertzbein–Robbins classification scale (Grade A = 0 mm breach distance, B = < 2 mm, C = < 4 mm, D = < 6 mm, E > 6 mm) before screw revision
Furthermore, rates of pedicle screw placements rated GRS C–E were analyzed regarding the distance from the index vertebral body the spinal navigation was registered to. A trend towards more GRS C-E for vertebral bodies distant more than three levels from the index level was found (Fig. 4).
System accuracy. In Fig. 4, the accuracy of pedicle screw placement according to the Gertzbein and Robbins classification system (GRS) is illustrated in relation to the position of the reference array. The distance was measured as the number of vertebral levels between the instrumented and index levels
ORCT was used for imaging in 14 cases (70%) and a 3D C-arm in 6 cases (30%), depending on its availability at the time of surgery.
Mean ± SD (Min–Max) radiation dose for ORCT was 1418 ± 464 (838–2164) mGy and 150 ± 61 (92–271) mGy per pedicle screw. For 3D C-arm imaging, the dose was 2195 ± 881 (1099–3617) mGy and 370 ± 165 (193–595) mGy per pedicle screw (Table 2).
Discussion
Assessment of safety, efficacy, and accuracy
For the present study, we evaluated a new navigation system enabling augmented AR-supported pedicle screw placement while integrating navigation cameras into the reference array and drill guide. The clinical application of the image-guided navigation system was feasible in multiple indications, such as trauma, degeneration, infection, and tumor. Pedicle screw placement was performed in open and in percutaneous technique, and navigation was precise in both techniques. Additional cement augmentation of the cannulated pedicle screws was performed in 50% of cases.
In all cases, navigated pedicle screw placement could be performed successfully, while intraoperative imaging had to be repeated in 15% of the cases due to insufficient imaging data, and in one case, a delay related to software issues (5.0%) was reported. With a focus on accuracy and patient safety, 90.5% of pedicle screws were rated GRS Grade A or B (Fig. 3), with a rate of screw revisions of 1.7% in this study. No new neurological deficits postoperatively. In a large study performed by Ille et al. [11] analyzing the accuracy of navigated pedicle screw placement in 6733 pedicle screws of the whole spine, an overall rate of screw revision of 3.4% was observed. Another study conducted by Ryang et al. [9] in 2011 and 2012 on navigated pedicle screw placement reported a screw revision rate of 4.7% for lumbar pedicle screw placement. These results match with studies performed by Waschke et al. reporting accuracy rates of 96.4% in CT-navigated pedicle screw placement, and Tkatschenko et al. showing accuracy rates of 96.6% for navigated percutaneous pedicle screw implantation [7, 22].
In this study, the duration between skin incision and first intraoperative imaging was 19 ± 11 (9–40) min, and the estimated duration per screw was 6.5 ± 1.9 (4.0–11.5) minutes. A comparable study by Ding et al. on navigated pedicle screw placement measured a time of skin incision to reference frame attachment of 28.3 ± 20.4 min and a time of 7.8 ± 2.7 min for a single pedicle screw placement [23]. The average time required from skin incision to reference frame attachment was 28.3 ± 20.4 min, and the average time required for insertion of a single pedicle screw was 7.8 ± 2.7 min [23]. Durations of pedicle screw placement on the thoracolumbar spine as low as 3.9 ± 2.5 (1–22) min were reported by Ryang et al. [9]. However, this report measured the time from placement of the navigated drill guide on the supposed/ planned pedicle entry point to final pedicle screw insertion [9].
Regarding radiation dose, comparable settings for ORCT or 3D C-Arm imaging were applied compared to spinal navigation systems routinely applied at our institution. This results in a similar radiation dose, in total as well as per pedicle screw.
Canulated pedicle screws of titanium, as well as titanium rods, were used in this study. No intraoperative case of hardware failure was reported. One implant failure (loosened pedicle screw nuts) occurred in a long-segment construct.
Intraoperative set-up
Conventional CT-based spinal navigation systems applied in clinical routine mostly require a setup consisting of a central computing unit, display units and an external adjustable infrared camera [9, 11]. In many cases, the system is permanently installed in the operation room. Furthermore, a device for intraoperative 3D imaging, including software integration to the navigation system, is required. To provide intraoperative navigation, a reference array has to be attached to the patient, and all surgical instruments have to be equipped with reflective marker spheres.
In contrast, the system applied in this study offers excellent versatility. As the reference array is equipped with targets incorporating LEDs and any navigated instrument is equipped with a camera, there is no need for an external infrared camera constantly being placed in the field of vision of reflective markers (Fig. 1). This enables improved visibility of the reference array without the necessity to adapt camera positioning due to line-of-sight issues [24]. Furthermore, only one main computing unit compact in size and equipped with a single screen is required (Fig. 5). Overall, the setup is reduced to a minimum by integrating the cameras into the surgical instruments and establishing a flexible platform, including preoperative planning. No specific modifications of the operating room or the 3D-imaging device, such as installing a reference frame, are required. This results in great flexibility and enables a versatile application of the system in multiple operation rooms as well as for several indications reaching beyond the instrumentation of the spine. However, the targets incorporating LEDs and cameras are single-use materials and are required for every surgery.
Complete setup. Figure 5 represents the complete setup of the system required for spinal navigation. The mobile main computing unit (left) is equipped with a single screen. Furthermore, the sterile system (right) consists of two targets attached to the reference array and a camera attached to the surgical instruments, such as the navigated drill guide shown in this figure
Intraoperative addition of augmented reality
The system offers the option to apply AR intraoperatively. Intraoperatively, the 3D imaging is integrated into the navigation software enabling real-time planning of the pedicle screw positioning on an external screen or integrated into an augmented reality view. The view can be chosen by the surgeon individually and changed intraoperatively. AR goggles (NextAR Smart Glasses, Medacta, Castel San Pietro, Switzerland) present the 3D-imaging and neuronavigation data combined with the view of the operation situs (Fig. 2). Subjectively perceived, the fact that the surgeons' view has not been averted from the situs has been rated advantageously. In general, AR is constantly gaining increasing importance in surgery. Augmented reality in pedicle screw placement has become technically feasible over the last few years [13,14,15,16,17,18,19,20]. Recent studies in models and first clinical applications have shown promising results, especially regarding improved visualization of the situs, reduced time of surgery, and precise screw positioning [16, 25, 26].
Limitations
As this study aimed to evaluate the feasibility of this novel navigation system enabling AR, this study was limited to 20 patients at one single high-volume spine center. As a result, no specific analysis regarding instrumentation using only AR was performed.
Conclusion
Navigated pedicle screw placement using a system with integrated cameras for spinal navigation is feasible and appears safe in clinical use. The compact setup enables a versatile use of the system. In addition, the integration of AR and flexible screen application offer new opportunities when compared to an OR room-based navigation system. However, more extensive studies must be conducted in the future to assess the benefits of AR in detail.
Abbreviations
- 3D:
-
Three dimensional
- AR:
-
Augmented reality
- ASA:
-
American Society of Anaesthesiologists
- CT:
-
Computed tomography
- GRS:
-
Gertzbein and Robbins classification system
- LEDs:
-
Light emitting diodes
- ORCT:
-
Operation room-based sliding gantry computed tomography
- PS:
-
Pedicle screw
References
Ringel F, Stoffel M, Stuer C, Meyer B (2006) Minimally invasive transmuscular pedicle screw fixation of the thoracic and lumbar spine. Neurosurgery 59(4 Suppl 2):ONS361-6. https://doi.org/10.1227/01.NEU.0000223505.07815.74
Vazan M, Ryang YM, Barz M, Torok E, Gempt J, Meyer B (2019) Ankylosing spinal disease-diagnosis and treatment of spine fractures. World Neurosurg 123:e162–e170. https://doi.org/10.1016/j.wneu.2018.11.108
Hubertus V, Gempt J, Marino M et al (2021) Surgical management of spinal metastases involving the cervicothoracic junction: results of a multicenter, European observational study. Neurosurg Focus 50(5):E7. https://doi.org/10.3171/2021.2.FOCUS201067
Janssen IK, Jorger AK, Barz M, Sarkar C, Wostrack M, Meyer B (2021) Minimally invasive posterior pedicle screw fixation versus open instrumentation in patients with thoracolumbar spondylodiscitis. Acta Neurochir (Wien) 163(6):1553–1560. https://doi.org/10.1007/s00701-021-04744-z
Schwendner M, Motov S, Ryang YM, Meyer B, Krieg SM (2022) Dorsal instrumentation with and without vertebral body replacement in patients with thoracolumbar osteoporotic fractures shows comparable outcome measures. Eur Spine J 31(5):1138–1146. https://doi.org/10.1007/s00586-021-07044-3
Shin BJ, James AR, Njoku IU, Hartl R (2012) Pedicle screw navigation: a systematic review and meta-analysis of perforation risk for computer-navigated versus freehand insertion. J Neurosurg Spine 17(2):113–122. https://doi.org/10.3171/2012.5.SPINE11399
Waschke A, Walter J, Duenisch P, Reichart R, Kalff R, Ewald C (2013) CT-navigation versus fluoroscopy-guided placement of pedicle screws at the thoracolumbar spine: single center experience of 4,500 screws. Eur Spine J 22(3):654–660. https://doi.org/10.1007/s00586-012-2509-3
Shin MH, Hur JW, Ryu KS, Park CK (2015) Prospective comparison study between the fluoroscopy-guided and navigation coupled with O-arm-guided pedicle screw placement in the thoracic and lumbosacral spines. J Spinal Disord Tech 28(6):E347–E351. https://doi.org/10.1097/BSD.0b013e31829047a7
Ryang YM, Villard J, Obermuller T et al (2015) Learning curve of 3D fluoroscopy image-guided pedicle screw placement in the thoracolumbar spine. Spine J 15(3):467–476. https://doi.org/10.1016/j.spinee.2014.10.003
Meng XT, Guan XF, Zhang HL, He SS (2016) Computer navigation versus fluoroscopy-guided navigation for thoracic pedicle screw placement: a meta-analysis. Neurosurg Rev 39(3):385–391. https://doi.org/10.1007/s10143-015-0679-2
Ille S, Baumgart L, Obermueller T, Meyer B, Krieg SM (2021) Clinical efficiency of operating room-based sliding gantry CT as compared to mobile cone-beam CT-based navigated pedicle screw placement in 853 patients and 6733 screws. Eur Spine J 30(12):3720–3730. https://doi.org/10.1007/s00586-021-06981-3
Malham GM, Wells-Quinn T (2019) What should my hospital buy next? Guidelines for the acquisition and application of imaging, navigation, and robotics for spine surgery. J Spine Surg 5(1):155–165. https://doi.org/10.21037/jss.2019.02.04
Burström G, Persson O, Edström E, Elmi-Terander A (2021) Augmented reality navigation in spine surgery: a systematic review. Acta Neurochir (Wien) 163(3):843–852. https://doi.org/10.1007/s00701-021-04708-3
Carl B, Bopp M, Saß B, Pojskic M, Voellger B, Nimsky C (2020) Spine surgery supported by augmented reality. Global Spine J 10(2 Suppl):41s–55s. https://doi.org/10.1177/2192568219868217
Carl B, Bopp M, Saß B, Voellger B, Nimsky C (2019) Implementation of augmented reality support in spine surgery. Eur Spine J 28(7):1697–1711. https://doi.org/10.1007/s00586-019-05969-4
Elmi-Terander A, Burstrom G, Nachabe R et al (2019) Pedicle screw placement using augmented reality surgical navigation with intraoperative 3D imaging: a first in-human prospective cohort study. Spine (Phila Pa 1976) 44(7):517–525. https://doi.org/10.1097/BRS.0000000000002876
Ghaednia H, Fourman MS, Lans A et al (2021) Augmented and virtual reality in spine surgery, current applications and future potentials. Spine J 21(10):1617–1625. https://doi.org/10.1016/j.spinee.2021.03.018
Gibby J, Cvetko S, Javan R, Parr R, Gibby W (2020) Use of augmented reality for image-guided spine procedures. Eur Spine J 29(8):1823–1832. https://doi.org/10.1007/s00586-020-06495-4
Hersh A, Mahapatra S, Weber-Levine C et al (2021) Augmented reality in spine surgery: a narrative review. HSS J 17(3):351–358. https://doi.org/10.1177/15563316211028595
Schupper AJ, Steinberger J, Gologorsky Y (2021) Augmented reality in spine surgery. World Neurosurg 151:290. https://doi.org/10.1016/j.wneu.2021.05.041
Gertzbein SD, Robbins SE (1990) Accuracy of pedicular screw placement in vivo. Spine (Phila Pa 1976) 15(1):11–4. https://doi.org/10.1097/00007632-199001000-00004
Tkatschenko D, Kendlbacher P, Czabanka M, Bohner G, Vajkoczy P, Hecht N (2020) Navigated percutaneous versus open pedicle screw implantation using intraoperative CT and robotic cone-beam CT imaging. Eur Spine J 29(4):803–812. https://doi.org/10.1007/s00586-019-06242-4
Ding BTK, Kaliya-Perumal AK, Oh JY, Yu CS (2020) Prospective evaluation of the time required for insertion of 380 lumbar and sacral pedicle screws using navigation with an intraoperative 3-dimensional imaging system. Int J Spine Surg 14(3):368–374. https://doi.org/10.14444/7048
Rahmathulla G, Nottmeier EW, Pirris SM, Deen HG, Pichelmann MA (2014) Intraoperative image-guided spinal navigation: technical pitfalls and their avoidance. Neurosurg Focus 36(3):E3. https://doi.org/10.3171/2014.1.FOCUS13516
Yanni DS, Ozgur BM, Louis RG et al (2021) Real-time navigation guidance with intraoperative CT imaging for pedicle screw placement using an augmented reality head-mounted display: a proof-of-concept study. Neurosurg Focus 51(2):E11. https://doi.org/10.3171/2021.5.FOCUS21209
Yahanda AT, Moore E, Ray WZ, Pennicooke B, Jennings JW, Molina CA (2021) First in-human report of the clinical accuracy of thoracolumbar percutaneous pedicle screw placement using augmented reality guidance. Neurosurg Focus 51(2):E10. https://doi.org/10.3171/2021.5.FOCUS21217
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. This trial was funded entirely by institutional grants from the Department of Neurosurgery, Technical University of Munich, Germany, School of Medicine, Klinikum rechts der Isar. Dr. Meyer received honoraria, consulting fees, and research grants from Medtronic, Icotec AG, and Relievant Medsystems Inc.; honoraria and research grants from Ulrich Medical; honoraria and consulting fees from Spineart Deutschland GmbH and DePuy Synthes; and royalties from Spineart Deutschland GmbH; and is a consultant for Medacta International. Dr. Wostrack is a consultant for Medacta International. Dr. Ille is consultant for Brainlab AG and for Icotec AG and received honoraria from Nexstim Plc and Carl Zeiss Meditec.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Schwendner, M., Ille, S., Wostrack, M. et al. Evaluating a cutting-edge augmented reality-supported navigation system for spinal instrumentation. Eur Spine J 33, 282–288 (2024). https://doi.org/10.1007/s00586-023-08011-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-08011-w