Abstract
Purpose
The present study aimed to identify the clinical predictive factors for worsened spinal deformity (SD) following surgical resection via posterior approach for primary intramedullary tumors.
Methods
A systematic search was performed using PubMed, Web of Science, and Scopus databases to extract potential references. Observational studies reporting predictive factors for worsened SD following surgical resection via posterior approach for primary intramedullary tumors were included. The odds ratio (OR) was calculated for dichotomous parameters.
Results
Four retrospective cohort studies were included in the meta-analysis. They were comprised of two groups of patients; those who developed SD (n = 87) and those who did not (n = 227). For patients with IMSCTs, age under 25 years as well as age under 13 years were the demographic variables associated with postoperative SD (odds ratio [OR] 3.92; p = 0.0002 and OR 4.22; p = 0.003). In both the fusion and the non-fusion subgroups, preoperative spinal deformity strongly predicted postoperative SD (OR 11.94; p < 0.001), with the risk highly elevated among the non-fusion patients (OR 24.64; p < 0.0002). Thoracolumbar junction involvement was also found to be a predictor of postoperative SD for patients with IMSCT (OR 2.89; p = 0.02).
Conclusion
This study highlights the importance of considering age, preoperative spinal deformity, and thoracolumbar junction involvement as predictors of postoperative spinal deformity following surgical resection for IMSCT. These findings may provide guidance for the management of these patients, including the development of preoperative planning strategies and the selection of the most appropriate surgical approach for high-risk patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intramedullary spinal cord tumors (IMSCTs) are rare forms of central nervous system (CNS) neoplasms with a prevalence as low as 2–10% of all CNS neoplasms and an incidence of less than 1/100,000 people per year [1,2,3,4]. It most commonly presents with symptoms such as pain, sensory/motor deficits, and sphincter dysfunction [3]. Eventually, the majority of them require surgical resection. The access to the spinal canal is usually obtained by laminectomy, laminoplasty, or laminotomy, referred to as “posterior approach” methods.
Employing laminectomy as a surgical approach, accessibility to the spinal canal is accomplished by detaching the paraspinal muscles. This is followed by the removal of the spinous processes and associated ligaments, including the posterior interspinous ligament, which is a key component of the tension band mechanism [2]. Consequently, this detachment and removal leads to a reduction in the force exerted by the extensor muscles. As demonstrated by Pal et al. [5], the posterior columns are responsible for transmitting as much as 64% of the axial load.
Due to the decrease in extensor force following the procedure, there is a shift in load toward the anterior aspect of the spine. This shift, in a significant number of patients, culminates in postoperative spinal deformities (SD), predominantly kyphosis [6]. The growing spine is considerably more susceptible to deformity; thus, children and young adults exhibit a higher risk of developing SD post-laminectomy [7]. Reported incidence rates show substantial variability. Some studies have documented incidence rates as high as 64% among the younger population [8]. It is essential to interpret these figures with caution, especially when considering differences in surgical procedures and relatively low number of analyzed cases.
Laminoplasty, in which the posterior elements of the spinal column are replaced following en bloc removal of the laminae, has been introduced to avoid the complications seen in laminectomy. However, its effectiveness in preventing postoperative kyphosis is yet to be demonstrated [4, 9,10,11]. The purpose of this study is to determine the clinical predictive factors for worsened spinal alignment following surgical resection of IMSCTs via posterior approach, in order to indicate whether delayed spinal fusion may be required to prevent postoperative spinal deformity.
Methods
Search strategy
The screening procedure adhered to the guidelines outlined in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). A comprehensive literature search was conducted utilizing PubMed, Web of Science, and Scopus databases from the earliest available records until October 22, 2022, including studies published in all languages. The search was conducted using the following keywords: ((laminoplasty) OR (laminotomy) OR (laminectomy)) AND ((tumor*) OR (resection)) AND ((spinal_deformity) OR (kypho*)). The search was performed independently by one author (M.S.). The study’s protocol was registered through PROSPERO (registration no. CRD42023377675; https://www.crd.york.ac.uk/prospero/).
Selection criteria
The initial phase of screening involved a comprehensive evaluation of the titles and abstracts of the articles, in order to ascertain that they met three predefined criteria. These were: (1) written in the English language, (2) involving patients undergoing surgery via posterior approach for the treatment of IMSCTs, and (3) reporting risk factors for postoperative SD. The articles that passed the initial screening were then subjected to a secondary screening phase. This phase assessed whether the articles provided sufficient extractable data, and if they met the minimum sample size requirement (i.e., at least 10 patients). Any articles that failed to meet either of these criteria were excluded from further analysis. Screening was performed independently by two authors: M.S. and J.K. Disagreement at any step was resolved by the author, G.M.
Quality and publication bias evaluation
The quality of each study selected for analysis was evaluated using the modified Newcastle–Ottawa Scale (NOS). A study could earn a maximum of 2 points in the comparability category and a maximum of 1 point in the other categories, for a total of 9 points. A score of 7 or higher indicated high quality, a score between 6 and 4 indicated moderate quality, and a score of 3 or lower indicated low quality. The quality assessment was performed independently by one author (O.L.), and any disagreements were resolved through discussion with author G.M. Publication bias among the included studies was assessed through visual inspection of funnel plot asymmetry.
Statistical analysis
For the statistical analysis, dichotomized variables such as age and sex were pooled into an overall odds ratio (OR) and 95% confidence intervals (CI) to identify risk factors for postoperative SD. Additionally, patients were divided into subgroups depending on whether their diagnosis required fusion to assess any differences between the two groups. Random-effect models were used, and the heterogeneity of the overall OR was calculated using the I^2 statistic. Publication bias was again assessed through visual inspection of the funnel plot asymmetry. A p-value < 0.05 was considered statistically significant. All analyses were performed using Review Manager version 5.4.1 (Cochrane IMS).
Results
Search results
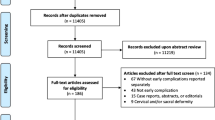
The comprehensive literature search resulted in the identification of 2730 unique records. The titles and abstracts of these records were critically evaluated for relevance, and 2697 records were subsequently excluded. The remaining thirty-three records underwent further analysis to evaluate the presence of extractable data. Twenty-nine records were determined to have insufficient data and were excluded from further consideration (Fig. 1). Hence, the final number of records included in this meta-analysis was four: they are listed in Table 1. They consisted of retrospective cohort studies, all rated as high quality according to the NOS (Supplementary Table 1).
PRISMA flowchart of the scientific literature search and study selection. Data added to the PRISMA template (from Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021; 372:n71) under the terms of the Creative Commons Attribution License. Figure is available in color online only
Publication bias
The funnel plot revealed an asymmetrical distribution of the included studies in the graph between the mean deviation (MD) and standard error, indicating the presence of publication bias (Supplementary Fig. 1).
Predictors of spinal deformity
A total of 20 extractable perioperative variables reported in the literature were assessed (Figs. 2, 3, 4, and 5, Supplementary Figs. 2–17). The identified statistically significant predictors for postoperative SD consisted of two demographic factors, one preoperative factor, and one intraoperative factor. For patients with IMSCT, age under 25 years was a demographic variable associated with postoperative SD (OR 3.83, 95%CI 1.59–9.22; p = 0.003) (Fig. 2). Additionally, age under 13 years was also displayed as a predictor for the development of spinal deformity post-tumor resection (OR 4.22, 95%CI 1.61–11.06; p = 0.003) (Fig. 3).
When pooling the fusion and non-fusion subgroups, the presence of preoperative SD was shown to be a strong predictor for postoperative SD (OR 11.94, 95%CI 2.66–53.64; p < 0.001) (Fig. 4). Furthermore, when assessing only non-fusion patients, preoperative spinal deformity was a statistically significant predictor for worsened SD (OR 24.64, 95%CI 4.59–132.3; p < 0.0002) (Fig. 4).
Thoracolumbar junction involvement and non-thoracolumbar junction involvement were assessed as predictors for postoperative SD. When assessing all patients, the thoracolumbar junction involvement group had a statistically significant increased prediction for SD (OR 2.89, 95%CI 1.20–6.99; p < 0.02) when compared to the latter (Fig. 5).
Variables that are lacking association with spinal deformity
All perioperative variables reported among the included studies were assessed for association with postoperative SD. Among the 20 variables, the following 16 were not statistically significant: sex, MMS at follow-up, preoperative MMS, astrocytoma, ependymoma, cervical involvement, thoracic involvement, lumbar involvement, cervicothoracic involvement, tumor confined in cervical region, tumor confined in thoracic region, tumor confined in lumbar region, single-level approach, two-level approach, 2 + level approach, laminoplasty, or laminotomy (Supplementary Figs. 2–17).
Discussion
This systematic review revealed that spinal alignment and age emerged as pivotal predictors in the progression of spinal deformity. The implications are profound. Additionally, regardless of whether patients underwent fusion or not, pre-existing SD was a dominant predictor of worsened postoperative outcomes, with an even higher odds ratio observed exclusively in non-fusion patients. Given that many neurosurgeons working on intradural intramedullary and extramedullary tumors are more entrenched in brain surgery than spine surgery, there is a pressing need for heightened awareness, as emphasized by this study, about spinal deformity and its predictive factors among this group of practitioners.
Of the four retrospective studies included, a total of 314 patients were included in this analysis. To the best of our knowledge, this is the first systematic review and meta-analysis to identify predictors for SD following IMSCT resection.
Age
Our study consists of patients of all ages, but is mainly focused on two age groups: patients under 25 years old and those under 13 years old. We found that both groups demonstrated a statistically significant prediction for spinal deformity (p = 0.003). It suggests that younger individuals, whose skeletal systems are still developing, may have an increased risk of developing spinal deformity post-resection [7]. The higher incidence of spinal deformity in younger populations after IMSCT resection may be attributed to a combination of factors, including age-related differences in spine elasticity, stress concentration in key areas, and progressive elastoplastic strain. In adults, deformation mainly impacts viscous–elastic structures, leading to motion segment instability and vertebral remodeling [12, 13]. Further research should, therefore, focus on finding the optimal cutoff age that accurately predicts postoperative SD, as this has yet to be identified [14, 15].
Preoperative spinal deformity
The previous studies have shown that preoperative spinal deformity tends to worsen postoperative spinal deformity (p = 0.07) [8, 15,16,17]. When pooling data together in this systematic review, we find compelling evidence that preoperative spinal deformity does predict postoperative spinal deformity (p = 0.001). Therefore, it seems to be an important factor to take into account when choosing treatment for patients with IMSCTs. Advances in preoperative planning and the use of advanced MRI might reduce the risk of postoperative spinal deformity when the patient is displaying preoperative deformity [18].
Preoperative spinal deformity has been frequently described throughout the literature in individuals receiving IMSCT resection. In their analysis of 55 pediatric IMSCT patients, Ahmed et al. found that an underlying abnormality was present in 20% of cases [19]. A preoperative abnormality was present in 56 out of 161 pediatric IMSCT patients, and 46% of those deformities progressed, 43% remained stable, and 11% resolved postoperatively [8]. It has been cogitated that involvement of the anterior horn of the spinal cord during IMSCT may cause muscular weakening. This is caused by diminished innervation of nearby muscles, which could result in an increased spinal deformity [15, 20].
Thoracolumbar junction involvement
When examining the relationship between thoracolumbar junction involvement and spinal deformity, a statistical significant finding emerges. The odds of predicting spinal deformity in this group of patients are present (p = 0.02). We can speculate that this finding appears due to the involvement and the ramification of the thoracic column and its osseoligamentous structures. When the posterior osseoligamentous structures are left intact, local denervation of the back muscles does not ultimately lead to deformity of the spine. This explanation was discovered and explored using an immature animal model [21].
The unparalleled incidence of spinal deformity explored in this study is not unique for IMSCT and has been observed in patients undergoing surgery in the thoracolumbar areas for trauma-related injuries. These patients have shown an increased incidence of postoperative spinal deformity [22]. It has been postulated that due to the high-stress nature of this region, which experiences rotational forces from the thoracic spine and significant mobilization stimulus from the lumbar region, spinal deformity tends to manifest in this area [23].
Limitations
This meta-analysis presents several limitations. Only one of the four studies presented preoperative Cobb angle measurements, and only two of the four provided the definition of the degree in which the Cobb angle needed to change before being considered significant. Instead, the definition was categorized as either “worse” or “not worse” and “requiring fusion” or “asymptomatic.” Due to this, despite being scored as high in quality, the studies included in this meta-analysis have lower reliability. Of the 20 variables assessed for association with spinal deformity (SD), only four were found to be significant. However, it is important to note that the lack of significant association for some variables may be due to limited evidence. Variables such as tumor type and locations in the spine should not be disregarded, as they require further assessment in the future studies (p values close to significant and/or lacking studies assessing the variable). Furthermore, different studies reported on a limited number of the same variables, which could result in different outcomes observed by different groups of surgeons. Given that IMSCT is a rare type of pathology, our study only contains a total of 314 patients, which might make it challenging to draw large conclusions about the population as a whole. Since a multivariate analysis was not possible to perform, this study does not provide independent predictors for SD after surgical resection. To account for heterogeneity, a random-effect model was used for meta-analysis. However, this method may not account for all heterogeneity. Owing to the highly specialized nature of the subject matter, it is acknowledged that certain cited references may appear antiquated. Despite diligent efforts to identify more contemporary research, such endeavors have been unsuccessful in yielding up-to-date sources.
Conclusion
In conclusion, this systematic review and meta-analysis aimed to evaluate the available literature on preoperative, postoperative, and intraoperative variables that may be associated with SD following surgical resection of IMSCTs. Our analysis revealed that following key variables: lower patient age, pre-existing spinal deformity, and thoracolumbar involvement were statistically significant predictors of postoperative SD.
Further research is necessary to develop a clinically applicable preoperative risk scoring system which takes into account the identified cutoff points of the significant predictors. While the findings from this study should be interpreted with caution, the variables identified may be of great value to those seeking to develop a preoperative scoring system for risk analysis to predict SD in the clinical setting [24].
References
Schellinger KA, Propp JM, Villano JL, McCarthy BJ (2008) Descriptive epidemiology of primary spinal cord tumors. J Neurooncol 87:173–179. https://doi.org/10.1007/S11060-007-9507-Z
Jecko V, Roblot P, Mongardi L et al (2022) Intramedullary spinal cord lesions: a single-center experience. Neurospine 19:108–117. https://doi.org/10.14245/NS.2143190.595
Knafo S, Aghakhani N, David P, Parker F (2021) Management of intramedullary spinal cord tumors: a single-center experience of 247 patients. Rev Neurol 177:508–514. https://doi.org/10.1016/J.NEUROL.2020.07.014
Tobin MK, Geraghty JR, Engelhard HH et al (2015) Intramedullary spinal cord tumors: a review of current and future treatment strategies. Neurosurg Focus 39:E14. https://doi.org/10.3171/2015.5.FOCUS15158
Pal GP, Sherk HH (1988) The vertical stability of the cervical spine. Spine (Phila Pa 1976) 13:447–449. https://doi.org/10.1097/00007632-198805000-00001
Arima H, Hasegawa T, Yamato Y et al (2021) Incidence and predictors of postoperative kyphotic deformity after thoracic spinal cord tumor resection. Spine Surg Relat Res 6:17–25. https://doi.org/10.22603/SSRR.2021-0092
Dimeglio A, Canavese F (2012) The growing spine: how spinal deformities influence normal spine and thoracic cage growth. Eur Spine J 21:64–70. https://doi.org/10.1007/S00586-011-1983-3
Yao KC, McGirt MJ, Chaichana KL et al (2007) Risk factors for progressive spinal deformity following resection of intramedullary spinal cord tumors in children: an analysis of 161 consecutive cases. J Neurosurg 107:463–468. https://doi.org/10.3171/PED-07/12/463
Goh KYC, Velasquez L, Epstein FJ (1997) Pediatric intramedullary spinal cord tumors: is surgery alone enough? Pediatr Neurosurg 27:34–39. https://doi.org/10.1159/000121222
Raimondi AJ, Gutierrez FA, Di Rocco C (1976) Laminotomy and total reconstruction of the posterior spinal arch for spinal canal surgery in childhood. J Neurosurg 45:555–560. https://doi.org/10.3171/JNS.1976.45.5.0555
Kehrli P, Bergamaschi R, Maitrot D (1996) Open-door laminoplasty in pediatric spinal neurosurgery. Childs Nerv Syst 12:551–552. https://doi.org/10.1007/BF00261609
Fassett DR, Clark R, Brockmeyer DL, Schmidt MH (2006) Cervical spine deformity associated with resection of spinal cord tumors. Neurosurg Focus 20:1–7. https://doi.org/10.3171/foc.2006.20.2.3
Lupparelli S, Pola E, Pitta L et al (2002) Biomechanical factors affecting progression of structural scoliotic curves of the spine. Stud Health Technol Inform 91:81–85. https://doi.org/10.3233/978-1-60750-935-6-81
De Jonge T, Slullitel H, Dubousset J et al (2005) Late-onset spinal deformities in children treated by laminectomy and radiation therapy for malignant tumours. Eur Spine J 14:765–771. https://doi.org/10.1007/S00586-004-0778-1
Yeh JS, Sgouros S, Walsh AR, Hockley AD (2001) Spinal sagittal malalignment following surgery for primary intramedullary tumours in children. Pediatr Neurosurg 35:318–324. https://doi.org/10.1159/000050444
Shi W, Wang S, Zhang H et al (2019) Risk factor analysis of progressive spinal deformity after resection of intramedullary spinal cord tumors in patients who underwent laminoplasty: a report of 105 consecutive cases. J Neurosurg Spine 30:655–663. https://doi.org/10.3171/2018.10.SPINE18110
Montano N, Trevisi G, Cioni B et al (2014) The role of laminoplasty in preventing spinal deformity in adult patients submitted to resection of an intradural spinal tumor. Case series and literature review. Clin Neurol Neurosurg 125:69–74. https://doi.org/10.1016/J.CLINEURO.2014.07.024
Juthani RG, Bilsky MH, Vogelbaum MA (2015) Current management and treatment modalities for intramedullary spinal cord tumors. Curr Treat Options Oncol 16:1–17. https://doi.org/10.1007/S11864-015-0358-0
Ahmed R, Menezes AH, Awe OO et al (2014) Long-term incidence and risk factors for development of spinal deformity following resection of pediatric intramedullary spinal cord tumors. J Neurosurg Pediatr 13:613–621. https://doi.org/10.3171/2014.1.PEDS13317
Sciubba DM, Chaichana KL, Woodworth GF et al (2008) Factors associated with cervical instability requiring fusion after cervical laminectomy for intradural tumor resection. J Neurosurg Spine 8:413–419. https://doi.org/10.3171/SPI/2008/8/5/413
Hemmy DC, Walsh PR, Larson SJ (1978) Effect of application of current on the paravertebral muscles of a primate model for kyphosis-PubMed. https://pubmed.ncbi.nlm.nih.gov/401243/. Accessed 25 Feb 2023
Price C, Makintubee S, Hemdon W, Istre GR (1994) Epidemiology of traumatic spinal cord injury and acute hospitalization and rehabilitation charges for spinal cord injuries in Oklahoma, 1988–1990. Am J Epidemiol 139:37–47. https://doi.org/10.1093/OXFORDJOURNALS.AJE.A116933
Takemura Y, Yamamoto H, Tani T (1999) Biomechanical study of the development of scoliosis, using a thoracolumbar spine model. J Orthop Sci 4:439–445. https://doi.org/10.1007/S007760050127
Pettersson SD, Skrzypkowska P, Ali S et al (2022) Predictors for cervical kyphotic deformity following laminoplasty: a systematic review and meta-analysis. J Neurosurg Spine 38:4–13. https://doi.org/10.3171/2022.4.SPINE22182
Funding
None reported.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None reported.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Szyduczyński, M., Korneliussen, J., Landé, O. et al. Predictors for spinal deformity following resection of intramedullary tumor via posterior approach: a systematic review and meta-analysis. Eur Spine J 32, 4355–4361 (2023). https://doi.org/10.1007/s00586-023-07957-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07957-1