Abstract
Objective
The C3 & C7 dome-hybrid open-door laminoplasty was proven to be an effective treatment for multi-levels cervical spondylotic myelopathy (CSM). However, its superiority over traditional unilateral open-door laminoplasty (UOLP) remains questionable, and no studies have compared the efficacy of this technique with traditional UOLP. This study aimed to compare the effectiveness of C3 & C7 dome-hybrid open-door laminoplasty with traditional UOLP in treating multi-levels CSM.
Methods
A retrospective study of multi-levels CSM with laminoplasty was performed, including 35 cases of traditional UOLP and 27 cases of C3 & C7 dome-hybrid open-door laminoplasty. Radiographic evaluation parameters and clinical outcomes were recorded to evaluate the surgical effectiveness.
Results
There was no significant difference in demographic baseline parameters. At the final follow-up, the C2–C7 Cobb angle of the modified group was significantly greater than that of the traditional group (p = 0.026). Meanwhile, the C2–C7 SVA of the modified group was significantly smaller than that of the traditional group (p = 0.009). Clinical outcomes such as VAS, NDI, and SF-12 scores, improved significantly in the modified group compared to the traditional group, while the JOA scores had no significant difference in both groups. There was no significant difference in the overall rate of complications between the two groups.
Conclusion
Both techniques have satisfactory outcomes in treating multi-levels CSM. Comparing with traditional UOLP, C3 & C7 dome-hybrid open-door laminoplasty has a greater superiority in reducing postoperative neck pain and maintaining the cervical sagittal alignment. It is proven to be a feasible management for patients with multi-levels CSM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cervical spondylotic myelopathy (CSM) is a common degenerative spinal disease caused by stenosis of the spinal canal and compression of spinal cord, often resulting in spinal cord dysfunction and associated clinical symptoms and signs [1, 2]. Currently, there is no effective way to treat or prevent the progression of CSM. For patients with evidence of spinal cord compression and signs of myelopathy or root compression, surgery is a common effective treatment option [2,3,4]. Previous literatures have described many surgical techniques to manage the CSM. Generally, anterior surgical approach, such as anterior cervical discectomy and fusion and anterior cervical corpectomy and fusion, is suitable for the management of 1- to 2-level CSM [5,6,7]. While for 3- or multi-levels CSM, posterior surgical approach, such as unilateral open-door laminoplasty (UOLP), may be the optimal choice [6, 8].
Traditional cervical UOLP was first developed in the 1970s [9]. This technique aims to widen the spinal canal and decompress the spinal cord by reconstructing the lamina and has become a mature and prevalent surgical technique in treating multi-levels CSM. However, traditional UOLP is often associated with a number of complications, including loss of lordosis, cervical sagittal imbalance and axial neck pain, which seriously affect the postoperative recovery and quality of life of patients [10,11,12,13,14].
Cervical sagittal imbalance has been reported to be closely related to detachment of the semispinalis cervicis muscle during UOLP [14]. Previous studies have shown that disruption of muscle attachments of C2 and C7 spinous processes is related with worse cervical sagittal alignment and serious neck pain [15,16,17,18]. To avoid injury of muscle attachments after traditional UOLP, Liu et al. reported a novel muscle sparing technique using C3 dome-osteotomy, C4–C6 UOLP and C7 dome-osteotomy, which has been shown to be an effective treatment choice for multi-level cervical myelopathy patients with fewer complications [19]. However, its superiority over traditional UOLP remains questionable, and no studies we know of have compared the efficacy of this technique with traditional UOLP. In the present study, we aimed to evaluate the clinical and radiological outcomes between C3 & C7 dome-hybrid open-door laminoplasty technique and traditional UOLP in treating multi-levels cervical myelopathy.
Patients and methods
Study design
This study was approved by our Institutional Review Board. We retrospective analyzed consecutive patients with multi-levels CSM underwent surgical treatment from September 2016 to December 2019. The inclusion criteria were as follows: (1) symptomatic CSM with C3-C7 multi-levels cord compression, (2) K-line (+) in the cervical spine, and (3) minimal preoperative neck pain. The exclusion criteria included: (1) kyphotic cervical deformities, (2) previous cervical surgeries, (3) patients combined with cervical fracture, tumor, infection and so on, and (4) the follow-up time was less than 24 months.
Surgical procedures
All surgeries were conducted by two senior doctors of same medical team. Under general anesthesia, the prone position was taken to make the neck slightly flexion, and a posterior median incision of the neck was performed. The skin, subcutaneous tissue and nuchal ligament were dissected layer by layer until the cervical spinous process was exposed, and the most severe compression site was selected as the open side. In the modified group, after the dissection of paravertebral muscles along the laminae, the interspinous ligament complex was cut between C3–C4 and C6–C7, respectively, and the tips of the C4–C6 spinous processes were removed, while the ending points of the cervical semi-spinous muscles at the tips of the C2 and C7 spinous processes were preserved. The caudal lamina of C3 and the upper part of C7 lamina were ground thin with a high-speed drill, and the residual lamina and thickened ligamentum flavum were carefully removed with a laminar rongeur. This process creates a dome-like osteotomy. A “V” shape gutters were created at C4–C6 using a high-speed drill on both sides, and a unilateral open-door laminoplasty at C4–C6 was performed. Afterward, the appropriate size of miniplates were selected to fix the expanded spinal canal. Finally, the drainage tube was placed and the incision was closed layer by layer. In the traditional group, the C3–C7 laminoplasty was performed as previously described [9], and the incision was closed in the same way as in the modified group.
Postoperative protocol
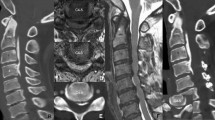
After surgery, ambulant was suggested for patients on the first postoperative day, and the drain was removed within 24 h after surgery. The neck muscle exercises were started at 2 days after surgery. Every patient needed to wear a soft cervical collar for two weeks after surgery, and then were allowed to gradually resume normal activities. The patients were followed up routinely at 3, 6, and 12 months within the first postoperative year and then followed up once a year (Fig. 1). Clinical and radiological evaluation were performed routinely during follow-up.
A 54-year-old male with multi-levels cervical spondylotic myelopathy. Preoperative X-ray lateral view and MRI (T2) sagittal view showed multi-levels spinal cord compression (a, b). The patient underwent C3 & C7 dome-hybrid open-door laminoplasty and immediately postoperative X-ray lateral view showed the titanium miniplates in good position (c). The X-ray lateral view and MRI (T2) sagittal view at 6 months (d, e) and final follow-up (f, g) showed satisfactory results without cervical instability and kyphosis occurred
Outcomes measures
The primary outcome measures were radiological outcomes. To achieve this, preoperative and the final follow-up lateral cervical X-ray films were used to measure sagittal parameters, including cervical lordosis and C2–C7 sagittal vertical axis (C2–C7 SVA). Cervical lordosis was measured using the C2–C7 Cobb angle, which was the angle between the upper endplate of C2 vertebral body and the lower endplate of C7 vertebral body; C2–C7 SVA was defined as the vertical distance between the vertical line of the C2 center and the C7 postero-superior corner.
The second outcome measures were clinical outcomes and complications. Clinical outcomes included Japanese Orthopaedic Association (JOA) score, neck disability index (NDI), the visual analog scale (VAS) pain score and the SF-12 concise health survey. These values were recorded before surgery and at the final follow-up. The neurologic function evaluation of each patient was evaluated using JOA score [20]. We used the VAS score to evaluate the neck pain level [21], and the NDI score to assess the neck functional status [22]. The SF-12 were used to evaluate the general health status and the quality of life comprehensively [23]. Complications included cerebrospinal fluid leakage, neck axial pain, C5 nerve root palsy, and cervical kyphosis were recorded.
To avoid bias, the clinical and radiological evaluation was performed by two spine surgeons not involved in the surgical treatment of these patients.
Statistical analysis
All analyses were carried out using SPSS 25.0 software (Chicago, Illinois, USA). Continuous variables were presented as mean ± SD or as the median and range. Independent t-test was applicated for comparison between two groups for continuous variable complying with a normal distribution. Mann–Whitney U-test was applicated to compare non-normally distributed continuous variables, and Fisher’s exact test was used to assess categorical variables. A p value < 0.05 was considered as statistically significant.
Results
Participants’ baseline data
A total 62 patients were enrolled in this study. Among them, 27 patients received C3 & C7 dome-hybrid open-door laminoplasty (modified group), 35 patients received C3–C7 UOLP (traditional group). We found no significant difference in demographic baseline parameters such as age, gender and body mass index between the two groups. No significant differences in ASA status, operation time, intraoperative blood loss and follow-up time were observed between the two groups (Table 1).
Radiological outcomes
There were no significant differences in preoperative sagittal parameters between the two groups (Table 2). At the final follow-up, the Cobb angle of the two groups decreased in varying degrees. In modified group, the mean C2–C7 Cobb angle decreased from 18.7° ± 8.1° before surgery to 16.6° ± 7.5° at the final follow-up. Similarly, the mean C2–C7 Cobb angle decreased from 16.3° ± 7.7° before surgery to 11.8° ± 8.7° at the final follow-up in traditional group. At the final follow-up, the C2–C7 Cobb angle of the modified group was significantly greater than that of the traditional group (p = 0.026). The mean C2-C7 SVA of modified group was increased from 18.4 ± 9.2 mm before surgery to 20.3 ± 7.8 mm at the final follow-up. Meanwhile, the mean C2–C7 SVA increased from 18.2 ± 8.8 mm to 26.0 ± 8.5 mm in traditional group. There was significant difference in C2–C7 SVA at the final follow-up between the two groups (p = 0.009).
Clinical outcomes
There were no significant differences in the preoperative VAS, JOA and NDI scores (p = 0.651, p = 0.283, and p = 0.613, respectively; Table 3). In modified group, the median VAS score was 4 (3–5) before surgery, and decrease to 1 (0–4) at the final follow-up. The median VAS score of traditional group decreased from 4 (3–6) before surgery to 2 (1–4) at the final follow-up. The median VAS score of the modified group at the final follow-up was significantly lower than that of the traditional group (p < 0.001). For modified group, the median JOA scores improved from 10 (7–13) before surgery to 15 (12–17) at the final follow-up. In the traditional group, the median JOA scores improved from 10 (7–13) before surgery to 15 (14–16) at the final follow-up. No statistical differences in the JOA scores were observed between the two groups. The NDI scores indicated significant improvement after surgery in both groups. In the modified group, the median NDI scores improved from 26 (12–34) before surgery to 6 (2–10) at the final follow-up. Similarly, the median NDI scores improved from 24 (12–35) before surgery to 8 (3–20) at the final follow-up in the traditional group. At the final follow-up, the difference in NDI scores between two groups was statistically significant (p = 0.020). The median SF-12 physical component summary (PCS) improved from 30 (10–50) preoperatively to 75 (65–95) at the final follow-up in the modified group, and from 30 (10–60) preoperatively to 70 (50–90) at the final follow-up in the traditional group. A significantly higher SF-12 PCS was observed in the modified group than that in the traditional group at the final follow-up (p = 0.004). Similarly, the median SF-12 mental component summary (MCS) improved from 50 (25–83) preoperatively to 71 (63–75) at the final follow-up in the modified group, and from 54 (25–83) preoperatively to 67 (50–75) at the final follow-up in the traditional group. A significantly higher SF-12 MCS was observed in the modified group than that in the traditional group at the final follow-up (p = 0.033).
Complications
There was no significant difference in the overall rate of complications between the modified group (2.7%, 1 of 27) and the traditional group (14.3%, 5 of 35) groups (p = 0.220) (Table 4). One patient (2.9%) experienced cerebrospinal fluid leakage during the operation in the traditional group, whereas no cerebrospinal fluid leakage occurred in modified group. During the period of follow-up, the incidence of neck axial pain was slightly higher in the traditional group (8.8%, 3 patients) than that in the modified group (3.7%, 1 patients) group (p = 0.626). Cervical kyphosis was found in one patient (2.9%) at the final follow-up in the traditional group. In contrast, no cervical kyphosis occurred in modified group. No C5 nerve root palsy was observed in either group.
Discussion
The traditional UOLP technique was first described by Hirabayashi and has become a mature surgical technique for treating multi-levels CSM [9]. However, traditional UOLP destroys cervical posterior extensor muscles inescapably, which may lead to the development of postoperative complications, such as cervical kyphosis, loss of lordosis, and severe neck pain [12]. Recent studies indicated that the preservation of muscle attachments in laminoplasty can reduce the incidence of postoperative complications, which has been a crucial consensus for the management of multi-levels CSM [18, 19].
The posterior cervical muscles, especially C2 semispinalis cervicis muscle, play an important role in maintaining the cervical alignment and biomechanical stability [24,25,26]. Riew et al. [26] suggested that the detachment of semispinalis cervicis inserted at C2 spinous processes may cause postoperative cervical kyphosis and persistent neck pain after the traditional UOLP procedure. Moreover, the muscle-ligament complex at C7 insertion was also important to maintain a lordotic cervical spine and reduce neck pain after laminoplasty [16, 27, 28]. Cho et al. [29] hypothesized that detachment of the ligamentum nuchae at C7 insertion was significant related to postoperative progression of kyphosis and axial neck pain, whereas Hosono et al. [30] emphasized that preservation of the trapezius at C7 and C7 spinous process could reduce the postoperative neck pain compared to C3–C7 UOLP.
In light of the relationship between the posterior muscles and cervical alignment, some scholars developed modified muscle preservation laminoplasty to maintain sagittal balance and relieve neck pain postoperatively. Nori et al. [31] performed a modified muscle-preserving approach for patients with multi-levels CSM, and the results showed that this procedure can maintain satisfactory cervical sagittal alignment after surgery. Chen et al. [18] reported a modified C3 laminectomy combined with laminoplasty while preserving the posterior muscle-ligament complex, and this modified technique achieved satisfactory cervical sagittal alignment compared to traditional C3–C7 UOLP. Although these modified procedures have achieved good results, the optimum surgical method has not yet reached a consensus.
In a recent study, Liu et al. [19] introduced a modified hybrid laminoplasty technique, comprised C3 caudally dome-osteotomy, C4–6 UOLP, and C7 cephalad dome-osteotomy. As mentioned above, after traditional UOLP, patients are prone to the worse cervical alignment and cervical pain, which may be associated with the destruction of cervical posterior extensor muscles. Traditional UOLP damages C2 and C7 attachment muscle, which greatly reduces the mechanical role of the posterior extensor muscles in maintaining cervical sagittal alignment [12]. To compensate for the loss of lordosis, the residual extensor muscles need greater contraction force. Constant contraction of muscles may be related to neck pain and stiffness after laminoplasty [32]. To address this problem, modified hybrid laminoplasty technique innovatively adopted C3 & C7 dome-osteotomy instead of the C3 & C7 laminoplasty [19]. This procedure can preserve greater muscle attachments, which is beneficial to better cervical alignment and less postoperative neck pain. Moreover, the residual lamina of C3 and C7 prevent C5 nerve root palsy caused by excessive spinal cord migration. Although this new hybrid laminoplasty technique can maintain cervical sagittal alignment as well as obtain satisfactory clinical outcomes, which was considered as a safe, feasible, and reproducible option for multi-levels CSM, whether this modified dome-hybrid open-door laminoplasty is better than traditional ULOP is unclear. Therefore, we compared the efficacy of C3 & C7 dome-hybrid open-door laminoplasty with traditional UOLP. In the present study, the C2–C7 Cobb angle and C2–C7 SVA were measured to evaluate the cervical sagittal alignment. We found that the C2–C7 Cobb angle of modified group was significantly larger than traditional group, while the C2–7 SVA of modified group was significantly smaller than traditional group. Our results indicated that cervical sagittal balance could be maintained better with C3 & C7 dome-hybrid open-door laminoplasty.
The purpose of surgical treatment is to relieve symptoms and improve the quality of life of patients. In current study, there were no significant differences in the JOA scores preoperatively and after surgery between the two groups. This result suggested that the procedure of C3 & C7 dome-hybrid open-door laminoplasty could achieve the same decompression effect as traditional UOLP. In addition, we found that the postoperative neck VAS pain scores in modified group were significantly superior to traditional group. This result is consistent with previous report that the muscle-preserving laminoplasty leaded to reduction of postoperative neck pain [33]. For traditional laminoplasty, it is inevitable to detach partial semispinalis at C2, especially when the most cephalad laminoplasty level was C3 [15]. With this modified surgical method, we not only achieve satisfactory decompression, but also minimize the damage to the semispinalis at C2, thereby reducing the degree of neck pain after surgery. The NDI and SF-12 scores in modified group were also significantly superior to traditional group. Our study suggested that for patients with compression levels between C3/C4 and C6/C7 spinal level, C3 & C7 dome-hybrid open-door laminoplasty may achieve satisfactory clinical results.
In the present study, C3 & C7 dome-hybrid open-door laminoplasty shared a comparable rate of overall complications with traditional UOLP. However, the incidence of postoperative neck axial pain and cervical kyphosis was relatively lower in modified group than that in traditional group. This is likely due to the preservation of the posterior muscle-ligament complex when C3 & C7 dome-hybrid open-door laminoplasty performed. C5 nerve root palsy is also a nonnegligible surgical complication after traditional laminoplasty. Previous literatures reported that preoperative foraminal stenosis and postoperative spinal cord migration were chief risk factors for C5 nerve root palsy [34, 35]. The residual lamina of C3 and C7 in C3 & C7 dome-hybrid open-door laminoplasty could limit excessive dorsal migration of the spinal cord after modified laminoplasty, which is conducive to the prevention of postoperative C5 nerve root palsy [19]. However, limited by the small size, no C5 nerve root palsy was observed in this study. A long-term follow-up study with lager samples is need in the future to confirm this hypothesis.
This study also has some limitations. The main limitation is that this study is a single center retrospective study and may has a selection bias. Nevertheless, we believe that selection bias was not a significant limitation since all patients met the same inclusion and exclusion criteria, and there were no significant differences in preoperative participants’ baseline data between two groups. During the control period, all surgeries were conducted by same medical team, and all patients received same postoperative protocol. Likewise, during the follow-up, all patients were evaluated using the same outcomes measurement methods. Second, the sample size is small and the follow-up period is insufficient; therefore, not all complications may have been observed in this study. To further compare the effectiveness of C3 & C7 dome-hybrid open-door laminoplasty with traditional UOLP, a randomized controlled trial with larger sample sizes and longer follow-up period should be performed in the future.
Conclusion
Both the C3 & C7 dome-hybrid open-door laminoplasty and traditional UOLP have satisfactory outcomes in treating multi-levels CSM. Comparing with traditional UOLP, C3 & C7 dome-hybrid open-door laminoplasty has a greater superiority in reducing postoperative neck pain and maintaining the cervical sagittal alignment. Furthermore, the modified technique achieved the same neurological results as traditional technique. It is proven to be a feasible management for patients with multi-levels CSM.
References
Iyer A, Azad TD, Tharin S (2016) Cervical spondylotic myelopathy. Clin Spine Surg 29(10):408–414
Singh A, Tetreault L, Casey A, Laing R, Statham P, Fehlings MG (2015) A summary of assessment tools for patients suffering from cervical spondylotic myelopathy: a systematic review on validity, reliability and responsiveness. Eur Spine J 24(Suppl 2):209–228
Fehlings MG, Tetreault LA, Riew KD et al (2017) A clinical practice guideline for the management of patients with degenerative cervical myelopathy: recommendations for patients with mild, moderate, and severe disease and nonmyelopathic patients with evidence of cord compression. Glob Spine J 7(3 Suppl):70S-83S
Fehlings MG, Arvin B (2009) Surgical management of cervical degenerative disease: the evidence related to indications, impact, and outcome. J Neurosurg Spine 11(2):97–100
Edwards CC 2nd, Riew KD, Anderson PA, Hilibrand AS, Vaccaro AF (2023) Cervical myelopathy. Current diagnostic and treatment strategies. Spine J 3(1):68–81
Bakhsheshian J, Mehta VA, Liu JC (2017) Current diagnosis and management of cervical spondylotic myelopathy. Glob Spine J 7(6):572–586
Hu Y, Lv G, Ren S, Johansen D (2016) Mid- to long-term outcomes of cervical disc arthroplasty versus anterior cervical discectomy and fusion for treatment of symptomatic cervical disc disease: a systematic review and meta-analysis of eight prospective randomized controlled trials. PLoS ONE 11(2):e0149312
McCormick JR, Sama AJ, Schiller NC, Butler AJ, Donnally CJ 3rd (2020) Cervical spondylotic myelopathy: a guide to diagnosis and management. J Am Board Fam Med 33(2):303–313
Hirabayashi K, Watanabe K, Wakano K, Suzuki N, Satomi K, Ishii Y (1983) Expansive open-door laminoplasty for cervical spinal stenotic myelopathy. Spine (Phila Pa 1976) 8(7):693–699
Kimura A, Shiraishi Y, Inoue H, Endo T, Takeshita K (2018) Predictors of persistent axial neck pain after cervical laminoplasty. Spine (Phila Pa 1976) 43(1):10–15
Suk KS, Kim KT, Lee JH, Lee SH, Lim YJ, Kim JS (2007) Sagittal alignment of the cervical spine after the laminoplasty. Spine (Phila Pa 1976) 32(23):E656–E660
Weinberg DS, Rhee JM (2020) Cervical laminoplasty: indication, technique, complications. J Spine Surg 6(1):290–301
Cho SK, Kim JS, Overley SC, Merrill RK (2018) Cervical laminoplasty: indications, surgical considerations, and clinical outcomes. J Am Acad Orthop Surg 26(7):e142–e152
Lin S, Zhou F, Sun Y, Chen Z, Zhang F, Pan S (2015) The severity of operative invasion to the posterior muscular-ligament complex influences cervical sagittal balance after open-door laminoplasty. Eur Spine J 24(1):127–135
Michael KW, Neustein TM, Rhee JM (2016) Where should a laminoplasty start? The effect of the proximal level on post-laminoplasty loss of lordosis. Spine J 16(6):737–741
Secer HI, Harman F, Aytar MH, Kahraman S (2018) Open-door laminoplasty with preservation of muscle attachments of C2 and C7 for cervical spondylotic myelopathy: retrospective study. Turk Neurosurg 28(2):257–262
Kotani Y, Abumi K, Ito M et al (2012) Impact of deep extensor muscle-preserving approach on clinical outcome of laminoplasty for cervical spondylotic myelopathy: comparative cohort study. Eur Spine J 21(8):1536–1544
Chen C, Li J, Liao Z, Gao Y, Shao Z, Yang C (2020) C3 laminectomy combined with modified unilateral laminoplasty and in situ reconstruction of the midline structures maintained cervical sagittal balance: a retrospective matched-pair case-control study. Spine J 20(9):1403–1412
Liu G, Fung G, Tan J, Ng JH, Tan JH (2020) A feasibility study of a new muscle sparing “C3 Dome-Hybrid Open-Door Laminoplasty”: a surgical technique, clinical outcome, and learning curve description. Spine (Phila Pa 1976) 45(19):E1256–E1263
Fujibayashi S, Neo M, Yoshida M, Miyata M, Takemoto M, Nakamura T (2010) Neck muscle strength before and after cervical laminoplasty: relation to axial symptoms. J Spinal Disord Tech 23(3):197–202
Cheung J, Cheung P, Law K et al (2019) Postoperative rigid cervical collar leads to less axial neck pain in the early stage after open-door laminoplasty—a single-blinded randomized controlled trial. Neurosurgery 85(3):325–334
Pietrobon R, Coeytaux RR, Carey TS, Richardson WJ, DeVellis RF (2002) Standard scales for measurement of functional outcome for cervical pain or dysfunction: a systematic review. Spine (Phila Pa 1976) 27(5):515–522
Gandek B, Ware JE, Aaronson NK et al (1998) Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project. International quality of life assessment. J Clin Epidemiol 51(11):1171–1178
Shimizu K, Mitsuhara T, Takeda M, Kurisu K, Yamaguchi S (2021) Effects of preservation of the semispinalis cervicis inserted into C2 on craniocervical alignment after laminoplasty. World Neurosurg 146:e1367–e1376
Sasai K, Saito T, Akagi S, Kato I, Ogawa R (2000) Cervical curvature after laminoplasty for spondylotic myelopathy–involvement of yellow ligament, semispinalis cervicis muscle, and nuchal ligament. J Spinal Disord 13(1):26–30
Riew KD, Raich AL, Dettori JR, Heller JG (2013) Neck pain following cervical laminoplasty: does preservation of the C2 muscle attachments and/or C7 matter. Evid Based Spine Care J 4(1):42–53
Johnson GM, Zhang M, Jones DG (2000) The fine connective tissue architecture of the human ligamentum nuchae. Spine (Phila Pa 1976) 25(1):5–9
Takeshita K, Peterson ET, Bylski-Austrow D, Crawford AH, Nakamura K (2004) The nuchal ligament restrains cervical spine flexion. Spine (Phila Pa 1976) 29(18):E388–E393
Cho CB, Chough CK, Oh JY, Park HK, Lee KJ, Rha HK (2010) Axial neck pain after cervical laminoplasty. J Korean Neurosurg Soc 47(2):107–111
Hosono N, Sakaura H, Mukai Y, Fujii R, Yoshikawa H (2006) C3–6 laminoplasty takes over C3–7 laminoplasty with significantly lower incidence of axial neck pain. Eur Spine J 15(9):1375–1379
Nori S, Shiraishi T, Aoyama R et al (2018) Muscle-preserving selective laminectomy maintained the compensatory mechanism of cervical lordosis after surgery. Spine (Phila Pa 1976) 43(8):542–549
Lin W, Song J, Zhang Y, Yao S et al (2023) Comparison of clinical outcomes of modified laminoplasty with preservation of muscle group inserted into C2 and C7 spinous processes versus conventional C3–C7 laminoplasty: a prospective, randomized, controlled, noninferiority trial. Int J Surg 109(4):905–912
Kato M, Nakamura H, Konishi S et al (2008) Effect of preserving paraspinal muscles on postoperative axial pain in the selective cervical laminoplasty. Spine (Phila Pa 1976) 33(14):E455–E459
Tsuji T, Matsumoto M, Nakamura M et al (2017) Factors associated with postoperative C5 palsy after expansive open-door laminoplasty: retrospective cohort study using multivariable analysis. Eur Spine J 26(9):2410–2416
Wu FL, Sun Y, Pan SF, Zhang L, Liu ZJ (2014) Risk factors associated with upper extremity palsy after expansive open-door laminoplasty for cervical myelopathy. Spine J 14(6):909–915
Acknowledgements
We wish to thank all of those who generously agreed to be interviewed for this research.
Funding
This research was funded by the National Natural Science Foundation of China, Grant number 81271347.
Author information
Authors and Affiliations
Contributions
Tao Xu and Shanxi Wang have contributed equally to this work. Huang Fang conceived and designed this study, Tao Xu and Shanxi Wang wrote the manuscript; Tao Xu and Shanxi Wang collected the data; Hongqi Zhao and Xuan Fang performed the clinical and radiologic assessment. Hua Wu and Feng Li performed the data analysis; Huang Fang reviewed and revised this manuscript. All authors reviewed the final manuscript. All authors agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Xu, T., Wang, S., Fang, H. et al. Comparative effectiveness and functional outcome of C3 & C7 dome-hybrid open-door laminoplasty with traditional unilateral open-door laminoplasty for cervical spondylotic myelopathy. Eur Spine J 33, 224–231 (2024). https://doi.org/10.1007/s00586-023-07953-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07953-5