Abstract
Purpose
Hounsfield unit (HU) measurements and vertebral bone quality (VBQ) scores are opportunistic screening methods for evaluating bone quality. Since studies comparing the efficacies of the two methods are rare, this retrospective study aimed to examine the efficacy of VBQ scores compared with that of HU measurements for diagnosing osteoporosis in lumbar spine surgery patients.
Methods
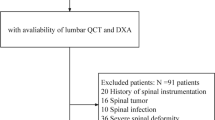
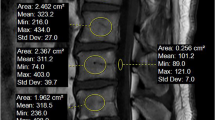
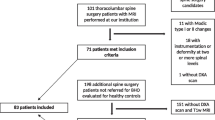
We selected patients who had undergone spinal surgery between January 2020 and May 2022 from our database. The VBQ scores based on magnetic resonance imaging (MRI) and HU measurements based on computed tomography (CT) were calculated. Correlation analysis of the dual-energy X-ray absorptiometry (DEXA) T score and study parameters was performed. The Delong test and decision curve analysis (DCA) were used to compare the efficacies of the two methods.
Results
We included 118 consecutive patients who underwent selective spinal surgery. The VBQ score and HU measurement were significantly correlated with the DEXA T score. Based on the Delong test, HU measurement predicted osteoporosis more effectively than the VBQ score did. The DCA revealed that the VBQ score performed better than the HU measurement did.
Conclusions
The calculation of VBQ scores is a novel opportunistic screening method for diagnosing osteoporosis; however, CT-based HU measurements outperform MRI-based VBQ scores. HU measurements can be used as a screening method when pre-operative CT scans are available.





Similar content being viewed by others
Availability of data and materials
Data available on request from the authors.
Code availability
Not applicable.
References
Hu YH, Yeh YC, Niu CC et al (2022) Novel MRI-based vertebral bone quality score as a predictor of cage subsidence following transforaminal lumbar interbody fusion. J Neurosurg Spine 37(5):654–662. https://doi.org/10.3171/2022.3.SPINE211489
Haffer H, Muellner M, Chiapparelli E et al (2022) Bone quality in patients with osteoporosis undergoing lumbar fusion surgery: analysis of the MRI-based vertebral bone quality score and the bone microstructure derived from microcomputed tomography. Spine J 22(10):1642–1650. https://doi.org/10.1016/j.spinee.2022.05.008
Zou D, Li W, Deng C, Du G, Xu N (2019) The use of CT Hounsfield unit values to identify the undiagnosed spinal osteoporosis in patients with lumbar degenerative diseases. Eur Spine J 28(8):1758–1766. https://doi.org/10.1007/s00586-018-5776-9
Schreiber JJ, Anderson PA, Rosas HG, Buchholz AL, Au AG (2011) Hounsfield units for assessing bone mineral density and strength: a tool for osteoporosis management. J Bone Jt Surg Am 93(11):1057–1063. https://doi.org/10.2106/JBJS.J.00160
Meredith DS, Schreiber JJ, Taher F, Cammisa FP, Girardi FP (2013) Lower preoperative Hounsfield unit measurements are associated with adjacent segment fracture after spinal fusion. Spine 38(5):415–418. https://doi.org/10.1097/BRS.0b013e31826ff084
Krishnaraj A, Barrett S, Bregman-Amitai O et al (2019) Simulating dual-energy X-ray absorptiometry in CT using deep-learning segmentation cascade. J Am Coll Radiol 16(10):1473–1479. https://doi.org/10.1016/j.jacr.2019.02.033
Choi MK, Kim SM, Lim JK (2016) Diagnostic efficacy of Hounsfield units in spine CT for the assessment of real bone mineral density of degenerative spine: correlation study between T-scores determined by DEXA scan and Hounsfield units from CT. Acta Neurochir 158(7):1421–1427. https://doi.org/10.1007/s00701-016-2821-5
Löffler MT, Jacob A, Scharr A et al (2021) Automatic opportunistic osteoporosis screening in routine CT: improved prediction of patients with prevalent vertebral fractures compared to DXA. Eur Radiol 31(8):6069–6077. https://doi.org/10.1007/s00330-020-07655-2
Zou D, Sun Z, Zhou S, Zhong W, Li W (2020) Hounsfield units value is a better predictor of pedicle screw loosening than the T-score of DXA in patients with lumbar degenerative diseases. Eur Spine J 29(5):1105–1111. https://doi.org/10.1007/s00586-020-06386-8
Zaidi Q, Danisa OA, Cheng W (2019) Measurement techniques and utility of Hounsfield unit values for assessment of bone quality prior to spinal instrumentation: a review of current literature. Spine 44(4):E239–E244. https://doi.org/10.1097/BRS.0000000000002813
Ehresman J, Schilling A, Pennington Z et al (2019) A novel MRI-based score assessing trabecular bone quality to predict vertebral compression fractures in patients with spinal metastasis. J Neurosurg Spine 32(4):499–506. https://doi.org/10.3171/2019.9.SPINE19954
Ehresman J, Pennington Z, Schilling A et al (2020) Novel MRI-based score for assessment of bone density in operative spine patients. Spine J 20(4):556–562. https://doi.org/10.1016/j.spinee.2019.10.018
Burns JE, Yao J, Summers RM (2017) Vertebral body compression fractures and bone density: automated detection and classification on CT images. Radiology 284(3):788–797. https://doi.org/10.1148/radiol.2017162100
Soliman MAR, Aguirre AO, Kuo CC et al (2022) Vertebral bone quality score independently predicts cage subsidence following transforaminal lumbar interbody fusion. Spine J 22(12):2017–2023. https://doi.org/10.1016/j.spinee.2022.08.002
St Jeor JD, Jackson TJ, Xiong AE et al (2020) Osteoporosis in spine surgery patients: what is the best way to diagnose osteoporosis in this population? Neurosurg Focus 49(2):E4. https://doi.org/10.3171/2020.5.FOCUS20277
Berger-Groch J, Thiesen DM, Ntalos D, Hennes F, Hartel MJ (2020) Assessment of bone quality at the lumbar and sacral spine using CT scans: a retrospective feasibility study in 50 comparing CT and DXA data. Eur Spine J 29(5):1098–1104. https://doi.org/10.1007/s00586-020-06292-z
Lubelski D, Choma TJ, Steinmetz MP, Harrop JS, Mroz TE (2015) Perioperative medical management of spine surgery patients with osteoporosis. Neurosurgery 77(Suppl 4):S92–S97. https://doi.org/10.1227/NEU.0000000000000939
Zou D, Muheremu A, Sun Z et al (2020) Computed tomography Hounsfield unit-based prediction of pedicle screw loosening after surgery for degenerative lumbar spine disease. J Neurosurg Spine 32(5):716–721. https://doi.org/10.3171/2019.11.SPINE19868
Dipaola CP, Bible JE, Biswas D et al (2009) Survey of spine surgeons on attitudes regarding osteoporosis and osteomalacia screening and treatment for fractures, fusion surgery, and pseudoarthrosis. Spine J 9(7):537–544. https://doi.org/10.1016/j.spinee.2009.02.005
Alswat K, Adler SM (2012) Gender differences in osteoporosis screening: retrospective analysis. Arch Osteoporos 7:311–313. https://doi.org/10.1007/s11657-012-0113-0
Schilling AT, Ehresman J, Pennington Z et al (2021) Interrater and intrarater reliability of the vertebral bone quality score. World Neurosurg 154:e277–e282. https://doi.org/10.1016/j.wneu.2021.07.020
Bloem JL, Reijnierse M, Huizinga TWJ, van der Helm-van AHM (2018) MR signal intensity: staying on the bright side in MR image interpretation. RMD Open 4(1):e000728. https://doi.org/10.1136/rmdopen-2018-000728
Ding Y, Chen JY, Yang JC et al (2023) Disc degeneration contributes to the denser bone in the sub-endplate but not in the vertebral body in patients with lumbar spinal stenosis or disc herniation. Spine J 23(1):64–71. https://doi.org/10.1016/j.spinee.2022.09.010
Funding
This work was supported by Joint Funds for the innovation of science and Technology, Fujian province (Grant number: 2020Y9055).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by TTX, XYH and YJ. The first draft of the manuscript was written by YJ, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
Institutional Review Board approval was obtained (approval no. 2021KJCX038).
Consent to participate
Written informed consent was not required for this study because this is a retrospective study.
Consent for publication
The authors affirm that human research participants provided informed consent for publication of the images in Figure 1A and B.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xu, TT., Huang, XY. & Jiang, YW. Efficacy of two opportunistic methods for screening osteoporosis in lumbar spine surgery patients. Eur Spine J 32, 3912–3918 (2023). https://doi.org/10.1007/s00586-023-07938-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07938-4