Abstract
Purpose
Radiological degenerative phenotypes provide insight into a patient’s overall extent of disease and can be predictive for future pathological developments as well as surgical outcomes and complications. The objective of this study was to develop a reliable method for automatically classifying sagittal MRI image stacks of cervical spinal segments with respect to these degenerative phenotypes.
Methods
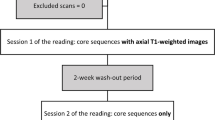
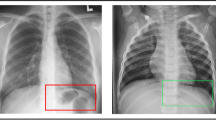
We manually evaluated sagittal image data of the cervical spine of 873 patients (5182 motion segments) with respect to 5 radiological phenotypes. We then used this data set as ground truth for training a range of multi-class multi-label deep learning-based models to classify each motion segment automatically, on which we then performed hyper-parameter optimization.
Results
The ground truth evaluations turned out to be relatively balanced for the labels disc displacement posterior, osteophyte anterior superior, osteophyte posterior superior, and osteophyte posterior inferior. Although we could not identify a single model that worked equally well across all the labels, the 3D-convolutional approach turned out to be preferable for classifying all labels.
Conclusions
Class imbalance in the training data and label noise made it difficult to achieve high predictive power for underrepresented classes. This shortcoming will be mitigated in the future versions by extending the training data set accordingly. Nevertheless, the classification performance rivals and in some cases surpasses that of human raters, while speeding up the evaluation process to only require a few seconds.





Similar content being viewed by others
Data, materials, and/or code availability
The material associated with the study is available upon reasonable request. The computer code and the images are confidential.
Abbreviations
- T2w:
-
T2-Weighted
- ROI:
-
Region of interest
- AI:
-
Artificial intelligence
- ACDF:
-
Anterior cervical discectomy fusion
- TSE:
-
Turbo spin-echo
- ROC:
-
Receiver-operator characteristic
- Post.:
-
Posterior
- Ant.:
-
Anterior
- Sup.:
-
Superior
- Inf.:
-
Inferior
- Abnorm.:
-
Abnormality
- DC:
-
Dilated convolutions
- Res:
-
Residual connections
- ClsW:
-
Class-weighted loss
References
Vos T, Allen C, Arora M et al (2016) Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 388(10053):1545–1602. https://doi.org/10.1016/S0140-6736(16)31678-6
Samartzis D, Borthakur A, Belfer I et al (2015) Novel diagnostic and prognostic methods for disc degeneration and low back pain. Spine J Off J North Am Spine Soc 15(9):1919–1932. https://doi.org/10.1016/j.spinee.2014.09.010
Luk KDK, Samartzis D (2015) Intervertebral disc “dysgeneration.” Spine J 15(9):1915–1918. https://doi.org/10.1016/j.spinee.2014.07.020
Määttä JH, Karppinen JI, Luk KDK, Cheung KMC, Samartzis D (2015) Phenotype profiling of Modic changes of the lumbar spine and its association with other MRI phenotypes: a large-scale population-based study. Spine J 15(9):1933–1942. https://doi.org/10.1016/j.spinee.2015.06.056
Samartzis D, Mok FPS, Karppinen J, Fong DYT, Luk KDK, Cheung KMC (2016) Classification of Schmorl’s nodes of the lumbar spine and association with disc degeneration: a large-scale population-based MRI study. Osteoarthr Cartil 24(10):1753–1760. https://doi.org/10.1016/j.joca.2016.04.020
Harada GK, Alter K, Nguyen AQ et al (2020) Cervical spine endplate abnormalities & association with pain, disability and adjacent segment degeneration after anterior cervical discectomy and fusion. Spine 45(15):E917–E926. https://doi.org/10.1097/BRS.0000000000003460
Harada GK, Tao Y, Louie PK et al (2020) Cervical spine MRI phenotypes and prediction of pain, disability and adjacent segment degeneration/disease after ACDF. J Orthop Res 39(3):657–670. https://doi.org/10.1002/jor.24658
Krizhevsky A, Sutskever I, Hinton GE (2016) ImageNet classification with deep convolutional neural networks. In: Pereira F, Burges CJC, Bottou L, Weinberger KQ (eds) Advances in neural information processing systems 25. Curran Associates, Inc.; 2012:1097–1105. http://papers.nips.cc/paper/4824-imagenet-classification-with-deep-convolutional-neural-networks.pdf. Accessed 17 Apr 2023
Schmidhuber J (2015) Deep learning in neural networks: an overview. Neural Netw 61:85–117. https://doi.org/10.1016/j.neunet.2014.09.003
Wang L, Li G, Shi F et al (2018) Volume-based analysis of 6-month-old infant brain MRI for autism biomarker identification and early diagnosis. In: Frangi AF, Schnabel JA, Davatzikos C, Alberola-López C, Fichtinger G (eds) Medical image computing and computer assisted intervention—MICCAI 2018. Lecture notes in computer science. Springer, pp 411–419
Ciompi F, de Hoop B, van Riel SJ et al (2015) Automatic classification of pulmonary peri-fissural nodules in computed tomography using an ensemble of 2D views and a convolutional neural network out-of-the-box. Med Image Anal 26(1):195–202. https://doi.org/10.1016/j.media.2015.08.001
Meng Y, Yi P, Guo X et al (2018) Detection for pulmonary nodules using RGB channel superposition method in deep learning framework. In: 2018 third international conference on security of smart cities, industrial control system and communications (SSIC) 1–8. https://doi.org/10.1109/SSIC.2018.8556807
Tang H, Kim DR, Xie X (2018) Automated pulmonary nodule detection using 3D deep convolutional neural networks. In: 2018 IEEE 15th international symposium on biomedical imaging (ISBI 2018) 523–526. https://doi.org/10.1109/ISBI.2018.8363630
Ebrahimighahnavieh MA, Luo S, Chiong R (2020) Deep learning to detect Alzheimer’s disease from neuroimaging: a systematic literature review. Comput Methods Programs Biomed 187:105242. https://doi.org/10.1016/j.cmpb.2019.105242
Tomita N, Cheung YY, Hassanpour S (2018) Deep neural networks for automatic detection of osteoporotic vertebral fractures on CT scans. Comput Biol Med 98:8–15. https://doi.org/10.1016/j.compbiomed.2018.05.011
Jamaludin A, Kadir T, Zisserman A (2017) SpineNet: automated classification and evidence visualization in spinal MRIs. Med Image Anal 41:63–73. https://doi.org/10.1016/j.media.2017.07.002
Niemeyer F, Galbusera F, Tao Y, Kienle A, Beer M, Wilke HJ (2021) A deep learning model for the accurate and reliable classification of disc degeneration based on MRI data. Invest Radiol 56(2):78–85. https://doi.org/10.1097/RLI.0000000000000709
Galbusera F, Niemeyer F, Wilke H-J et al (2019) Fully automated radiological analysis of spinal disorders and deformities: a deep learning approach. Eur Spine J 28(5):951–960. https://doi.org/10.1007/s00586-019-05944-z
Hosny A, Aerts HJ, Mak RH (2019) Handcrafted versus deep learning radiomics for prediction of cancer therapy response. Lancet Digit Health 1(3):e106–e107. https://doi.org/10.1016/S2589-7500(19)30062-7
Baker LC, Atlas SW, Afendulis CC (2008) Expanded use of imaging technology and the challenge of measuring value. Health Aff Proj Hope 27(6):1467–1478. https://doi.org/10.1377/hlthaff.27.6.1467
Wiens J, Shenoy ES (2018) Machine learning for healthcare: on the verge of a major shift in healthcare epidemiology. Clin Infect Dis 66(1):149–153. https://doi.org/10.1093/cid/cix731
Tao Y, Galbusera F, Niemeyer F, Samartzis D, Vogele D, Wilke H-J (2021) Radiographic cervical spine degenerative findings: a study on a large population from age 18 to 97 years. Eur Spine J 30(2):431–443. https://doi.org/10.1007/s00586-020-06615-0
Chartrand G, Cheng PM, Vorontsov E et al (2017) Deep learning: a primer for radiologists. Radiogr Rev Publ Radiol Soc N Am Inc 37(7):2113–2131. https://doi.org/10.1148/rg.2017170077
He K, Zhang X, Ren S, Sun J (2020) Deep residual learning for image recognition. In: Proceedings of the IEEE conference on computer vision and pattern recognition. 2016:770–778. https://openaccess.thecvf.com/content_cvpr_2016/html/He_Deep_Residual_Learning_CVPR_2016_paper.html. Accessed 17 Apr 2023
Szegedy C, Liu W, Jia Y et al (2015) Going deeper with convolutions. In: Proceedings of the IEEE conference on computer vision and pattern recognition. 1–9. https://www.cv-foundation.org/openaccess/content_cvpr_2015/html/Szegedy_Going_Deeper_With_2015_CVPR_paper.html. Accessed 17 Apr 2023
Chollet F (2017) Xception: deep learning with depthwise separable convolutions. In: Proceedings of the IEEE conference on computer vision and pattern recognition. 1251–1258. https://openaccess.thecvf.com/content_cvpr_2017/html/Chollet_Xception_Deep_Learning_CVPR_2017_paper.html. Accessed 17 Apr 2023
Kelleher JD, Namee BM, D’Arcy A (2020) Fundamentals of machine learning for predictive data analytics, second edition: algorithms, worked examples, and case studies. MIT Press
Maji S, Rahtu E, Kannala J, Blaschko M, Vedaldi A. Fine-grained visual classification of Aircraft. ArXiv13065151 Cs. Published online June 21, 2013. http://arxiv.org/abs/1306.5151. Accessed 17 Apr 2023
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
The study has been approved by the approved by Rush’s IRB as 18033101-IRB01, “Machine learning of cervical spine MRI phenotypes.”
Consent for publication
Since this was not a prospective study, but a retrospective study of preexisting records, patient informed consent was not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Niemeyer, F., Galbusera, F., Tao, Y. et al. Deep phenotyping the cervical spine: automatic characterization of cervical degenerative phenotypes based on T2-weighted MRI. Eur Spine J 32, 3846–3856 (2023). https://doi.org/10.1007/s00586-023-07909-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07909-9