Abstract
Background
Back pain occurs commonly in adults and is multifactorial in nature. This study aimed to assess the prevalence and intensity of back pain during young adulthood in subjects with adolescent idiopathic scoliosis (AIS), as well as factors that may be associated with its prognosis.
Methods
Subjects with AIS aged 20–39 treated conservatively were included in this study. Patient-reported outcome measures in adulthood involved episodes of back pain, and scales of self-image, depression, anxiety, and stress. Additionally, pain, self-image, and mental health scores were retrieved at the first clinic consultation. Occurrence of back pain was defined as a numeric pain rating scale ≥ 6.
Results
101 participants were enrolled. The prevalence of back pain in the lifetime, past 12 months, past 6 months, past 1 month, past 7 days, and past 24 h were 37%, 35%, 31%, 27%, 23%, and 20%, respectively. Male, self-image, and depression were significant associated factors for the development of back pain at all time points. Furthermore, the analyses of the initial presentation of participants have shown that participants with back pain in adulthood were characterised by poor self-image and mental health during their adolescence.
Conclusion
The present study addressed the natural history of back pain in young adults with conservatively treated AIS. Psychological makeup has been shown to constitute the development of back pain and is strongly hinted as an early sign of having back pain in adulthood among subjects with AIS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adolescent idiopathic scoliosis (AIS) is the most common spine deformity worldwide [1], and scoliotic individuals may complain of back discomfort [2]. Although back pain causes rapidly increased disability-adjusted life years in the global population when compared to other diseases and injuries [3], some researchers have found that the occurrence of back pain was significantly higher in subjects with scoliosis as compared to healthy adolescents [4, 5]. In the literature, the prevalence of back pain among scoliotic participants varied between papers, yet the reason for this variation is unknown [6,7,8,9].It has also been shown that back pain in AIS is a risk factor for developing back pain in adulthood [5]. But generally, the research into the prevalence distribution and severity of back pain among young adults is lacking [10,11,12].
Nevertheless, the pathomechanism of back pain in AIS is not known [13]. Based on the multifactorial aetiology of back pain [7], it was suggested that spinal morphology is not the only explanation [9]. Several associated factors for back pain in AIS were separately investigated, including age [6, 8], body mass index [5], Cobb angle [6, 8], curve pattern [9], appearance [7], and mental health [7,8,9]. However, the interplay among these factors is yet to be known. It remains uncertain whether physical and/or psychological factors contribute to the development of back pain.
To assess the burden of scoliosis-related back pain, the patient group without receiving definitive correction for the condition of AIS should be targeted. Accordingly, the information about this young adult group may help clinicians to mitigate their pain and prevent severe back problems. Given the above, the present study aimed to evaluate the prevalence and intensity of back pain among young adults with conservatively treated AIS. This study also aimed to determine the effects of psychological makeup on the perception of pain among participants.
Methods
The manuscript was prepared in accordance with the strengthening the reporting of observational studies in epidemiology (STROBE) recommendation [14].
Study design
This prospective cross-sectional study complied with the World Medical Association Declaration of Helsinki [15]. The study protocol obtained approval from the institutional review board of the University of Hong Kong and Hospital Authority Hong Kong West Cluster (reference number: UW 22-257). Informed consent was provided to the participants prior to any study procedures initiate.
Setting
The study site was a territory-wide referral centre in Hong Kong. It is one of the only two designated hospitals specialised in managing spinal deformity, which covers at least half of the local population. Subjects with AIS were screened consecutively from the patient lists of an orthopaedic scoliosis outpatient clinic between 04th January 2021 and 22nd December 2021. All eligible study subjects were included without restrictions on curve severity and curve pattern. Potential candidates were contacted by phone and enquired about their willingness to participate in this study. On top of the baseline assessment, an electronic database stored records of the Scoliosis Research Society patient outcome questionnaire during regular clinic visits was used. Data collected during the initial presentation were retrieved.
Participants
Study subjects aged 20–39 years with a primary diagnosis of AIS were eligible for inclusion, of which this specific age range of young adults was less affected by spinal degeneration [16]. Additionally, only those who attended the clinical appointment at the scoliosis clinic with the available radiological findings were included. The exclusion criteria were listed as follows, (1) spinal trauma, injury, fracture, or tumour, (2) history of spinal surgery, and (3) mental retardation. Electronic medical records were reviewed to confirm the eligibility.
Measurements
The primary outcomes were collected through a self-administered online survey (Qualtrics XM, United States). Particularly, the numeric rating scale (NRS) was adopted to quantify the intensity of back pain [17]. Average pain intensity in the lifetime, past 12 months, past 6 months, past 1 month, past 7 days, and past 24 h, was graded using a 0 (no pain) to 10 (extreme pain requiring emergency care) scale [18]. Other psychological factors were examined via the self-image subscale of the Scoliosis Research Society questionnaire [19], the patient health questionnaire [20], the generalised anxiety disorder scale [21], and the stress subscale of the depression anxiety stress scale [22]. The self-image subscale mapped one’s perceived appearance of the back, with a score of 5 being the best and 1 being the worst. The patient health questionnaire, the generalised anxiety disorder scale, and the stress scale estimated the depressive symptoms (0–27 points), anxiety symptoms (0–21 points), and stress levels (0–34 points) of participants, respectively. Smoking habit was affirmed by asking whether the participants have ever smoked, while alcohol consumption was asked by intake of alcoholic beverages or not over the past year. Furthermore, the radiographic assessment was used on the posteroanterior standing view of the whole spine (EOS imaging, France). Since all patients attending the scoliosis clinic would have the imaging taken routinely, no additional X-ray images were required for this study. The picture archiving and communication system (PACS) was utilised for measuring the Cobb angle of the major curve and classifying the curve pattern. Demographic data were extracted from the database of medical records. Alternatively, the pain, self-image, and mental health scores of the Scoliosis Research Society questionnaire collected during the first clinic consultation were also used.
Variables
Apart from the pain intensity, the occurrence of back pain was dichotomised into the study (NRS ≥ 6 points) and control groups (NRS < 6 points) [23]. The pain, self-image and mental health scores were the mean value of the questions answered, whereas the depression, anxiety, and stress scores were the accumulative points of the corresponding answers. Records of smoking and drinking were recognised as smokers and alcohol drinkers. Regarding the condition of AIS, the Cobb angle of the major curve was evaluated and subdivided into three levels of severity [24], namely mild curve as curve magnitude from 10° to 24°, moderate curve as between 25° and 44°, and severe curve as ≥ 45°. In addition, the categorisation of curve patterns (see Appendix) was adapted from the Lenke classification because the lack of bending films in non-surgical patients [25]. All spinal curves ≥ 10° were accounted. The six types of curvature involved, (a) main thoracic curve with a single curvature in the lower thoracic region, (b) double thoracic curves with two curvatures in both upper and lower thoracic regions, (c) double major curves I with two curvatures and the major curve at the thorax, (d) triple major curves with three curvatures over the spine, (e) thoracolumbar or lumbar curve with one curvature in the thoracolumbar or lumbar region, and (f) double major curves II with two curvatures and the major curve at the lower back. Conservative treatment was received for AIS, including observation, physiotherapy, and bracing.
Statistical analysis
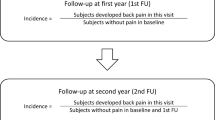
All data were analysed by the statistical package for the social sciences software version 28.0 (SPSS Inc., United States). The level of significance was set at 0.05. In light of the primary objective, the independent samples t-test was performed between participants with and without back pain. Subgroup analyses were performed by the Chi-squared test and Kruskal–Wallis test to evaluate participants with different curve severities, curve patterns, and treatments. In order to address the secondary objective, backward stepwise logistic and linear regression were applied to establish the associated factors for back pain. Further, the Mann–Whitney U test was performed between pain and control groups to compare the pain, self-image, and mental health scores measured in adolescence.
Results
Initially, 583 potential study subjects were retrieved and assessed for eligibility. Of them, 457 were excluded since they could not be reached (n = 243), declined to participate (n = 131), did not meet the inclusion criteria (n = 36), or had undergone spinal surgery (n = 47). After removing 25 entries due to incompletion of the survey, a total of 101 participants were enrolled in the present study (Fig. 1).
The demographics of participants were shown with mean and standard deviation or proportion in percentage (Table 1), comprising age of 24.5 ± 4.8 years, females rate at 77.2%, 1.6 ± 0.1 m in height, 53.5 ± 9.9 kg in weight, and body mass index of 19.9 ± 3.1. Among them, 4.0% and 58.4% were smokers and alcohol drinkers. In relation to their condition of AIS, the average Cobb angle of the major curve was 41.9° ± 13.8°. Most of them had a moderate (48.0%) or severe curve (41.0%), whereas the distribution of curve patterns mainly encompassed double major I (25.0%), triple major (26.0%), and double major II (31.0%). About half of them received bracing (49.5%).
In general, the prevalence of back pain in the lifetime, past 12 months, past 6 months, past 1 month, past 7 days, and past 24 h were 36.6%, 34.7%, 30.7%, 26.7%, 22.8%, and 19.8%, respectively. With reference to the intensity of back pain, the study group had significantly greater NRS than the control group in all periods (Table 2). The average pain intensity within the study group was denoted as 7.1 ± 1.1 points in the lifetime, 7.2 ± 1.2 points in the past 12 months, 7.2 ± 1.1 points in the past 6 months, 7.2 ± 1.2 points in the past 1 month, 7.1 ± 1.2 points in the past 7 days, and 7.3 ± 1.2 points in the past 24 h. Subgroup analyses have illustrated that curve severity, curve pattern, and treatment received were not associated with the prevalence and intensity of back pain (Tables 3 and 4).
As for the inputs of regression models, the following parameters were entered at the beginning stage, namely age, gender, body mass index, smoking, alcohol drinking, major Cobb angle, self-image, depression, anxiety, and stress scores.
Logistic regression was performed to ascertain the effects of associated factors on the likelihood that adult participants have back pain (Table 5). Age was associated with the occurrence of back pain in the lifetime (p = 0.001), past 12 months (p = 0.012), and past 24 h (p = 0.038). Males were associated with the occurrence of back pain in past 7 days (p = 0.034) and past 24 h (p = 0.040). History of smoking was associated with the occurrence of back pain in past 6 months (p = 0.030) and past 1 month (p = 0.023). History of alcohol drinking was associated with the occurrence of back pain in past 6 months (p = 0.011) and past 1 month (p = 0.034). Major Cobb angle was associated with the occurrence of back pain in the lifetime (p = 0.041), past 6 months (p = 0.028), and past 24 h (p = 0.025). Stress symptoms were associated with the occurrence of back pain in the lifetime (p = 0.032) and past 1 month (p = 0.045). Notably, the self-image score consistently showed associations with the occurrence of back pain at all time points.
Moreover, linear regression was performed to predict the intensity of back pain among participants (Table 6). Age was associated with the pain intensity in the lifetime (p = 0.001), past 12 months (p = 0.040), past 6 months (p = 0.019), and past 24 h (p = 0.020). Body mass index was associated with the pain intensity in past 7 days (p = 0.044). History of alcohol drinking was associated with the pain intensity in the lifetime (p = 0.048), past 12 months (p = 0.020), and past 6 months (p = 0.012). Anxiety symptoms were associated with the pain intensity in the lifetime (p = 0.005). More importantly, males, self-image score, and depressive symptoms constantly associated with the pain intensity at all times.
Accordingly, the retrospective analyses were implemented on the pain and psychological scores during the first presentation of participants (Table 7). Their mean age was 15.8 ± 4.7 years old, and the mean duration of follow-ups was 9.8 ± 4.2 years. Lower self-image scores were characterised by participants with back pain in past 12 months (p = 0.018), past 6 months (p = 0.012), past 7 days (p = 0.002), and past 24 h (p = 0.006) compared to those without pain. Likewise, participants with back pain in past 7 days and 24 h had significantly poorer mental health scores than individuals with no pain (p = 0.002, p = 0.017). Essentially, all participants with pain in adulthood demonstrated inferior self-image and mental health scores during adolescence compared to the control group. Pain scores were similar between groups at all time points.
Discussion
The present study identified for the first time that participants aged 20 to 39 with back pain possessed lower self-image and mental health during adolescence as compared to their counterparts. It also shows relationships between the occurrence and intensity of back pain with self-image and depression in adulthood.
The current results entailed that the current back pain in young adults with conservatively treated AIS was 20%. Despite direct comparisons that could not be made, this prevalence seems to be in line with other studies of scoliotic subjects. It has been observed that the prevalence of back pain was 18% during adolescence [8]. While back pain in the above 40 years of age has increased to 69% [11], there were 77% of elderlies experienced back pain [10]. The results of the present study fit into the above figures.
Meanwhile, other periods of back pain also implied increasing trends from adolescence to young adulthood. For instance, the 7-day prevalence was from 21% in adolescents to 23% as documented in this study [8], as well as the prevalence of 1-month, 6-month, and 12-month consistently evidenced the same progression (i.e., from 25 [8] to 27%, from 26 [7] to 31%, and from 30 [8] to 35%, respectively). Collectively, the prevalence of back pain in AIS has been showing an increment along with age. This was also confirmed by the regression models in the present study that increasing age was a significant associated factor.
Interestingly, the psychological makeup was substantiated as an important risk factor for back pain. The poor self-image is a sequela of scoliosis, and the current results have shown that the self-image was independently associated with back pain. Comparably, Makino et al. [7] described a significant odds ratio of 0.30 in self-image for predicting back pain. In the meantime, the topic of depression is still an unsolved puzzle in AIS [26, 27]. While Weinstein et al. [10] declared that the difference in depressive symptoms between older patients and healthy controls was insignificant, Matamalas et al. [28] presented a significant difference in depressive scores between patients with and without back pain. These findings together have insinuated the independent relationship between depression and back pain, which has been studied in academia recently [29, 30].
Consequently, the retrospective analyses of the initial psychological data provided new insights into the existing knowledge. Participants with back pain in adulthood had diminished self-image and mental health during their adolescence. Based on this finding, it could be inferred that the defective psychological factors were not coming after the development of back pain. This vicious cycle of back pain was likely to be aggravated by the worsening mental health at the beginning, and then the magnified severity of pain also contributed to the reduced mental health. Thus, the psychological makeup constituted the prognosis of back pain in subjects with AIS throughout their age development.
As noted, there was a proportion of scoliotic subjects with back pain in their young adulthood. With reference to the current findings, self-image and depression were potentially modifiable associated factors for back pain. Clinicians should try to manage patients’ psychological distress through physical (e.g., physiotherapeutic scoliosis-specific exercises for the correction of spinal alignment) and mental health interventions (e.g., early referral to clinical psychologist). In the hope that, though controlling the occurrence and intensity of back pain, future severe back problems and their associated consequences can be prevented.
Future studies should have a more precise definition of back pain. Given the evidence of impaired pain modulation in patients with back pain [31], a cut-off value of either NRS or visual analogue scale for determining the pain of interest is required. Further validation with the pressure pain threshold in the AIS population may be exploited [32]. Subsequently, the current results suggested inadequate intervention in self-image. Surgical intervention is deliberated as beneficial to the improvement of the self-image [33], but not the bracing [34]. As a result, scoliotic adolescents with mild and moderate curves are disadvantaged by the situation. Future research should be targeted this particular group with psychological intervention. For the relationship between back pain and depression, treatment direction may also focus on the changes in depressive symptoms on the prognosis of back pain in AIS. Lastly, the absence of curve conditions in the development of back pain is poorly understood. Although a few studies have exhibited the effects of severe curves among teenagers with back pain [6, 8, 9], there is no study that investigated the progression of pain into young and middle adulthood.
Several limitations are noted in this study. A drawback was the incomplete profile of back pain estimated. The pain was not characterised by curve location or convexity of the major curve. A few more confounding factors of back pain were not reviewed [13], for example, coronal balance, sagittal alignment, and vertebral rotation. Besides, it remains uncertain whether spinal degeneration exists. The records of back pain in the present study were due to the spinal curve or other problems like nerve issues are also unclear. Notwithstanding the four psychological variables addressed, the exploration of psychological distress in subjects with back pain may not be comprehensively outlined. The present study has already incorporated the commonest psychological factors in AIS [35]. In view of the subgroup analyses being underpowered (insufficient samples in particular subgroups), some results should be interpreted with caution. Lastly, there was a 19.8% of drop-out rate as noted in the present study. This may slightly affect the quality of the current results.
Conclusion
The present study described the prevalence distribution and severity of back pain in young adults with conservatively treated AIS. Importantly, the current results revealed that psychological makeup predominantly constituted the development of back pain. The results have also elucidated that there was a relationship between back pain in adulthood and self-image and mental health during adolescence. It is strongly hinted that reduced psychological factors may not be the consequence but aggravating factors for back pain. The proposed knowledge gaps generated from this study, inclusive of the relationship between back pain and psychological distress, should be clarified in future studies.
References
Weinstein SL, Dolan LA, Wright JG, Dobbs MB (2013) Effects of bracing in adolescents with idiopathic scoliosis. N Engl J Med 369(16):1512–1521. https://doi.org/10.1056/nejmoa1307337
Rushton PR, Grevitt MP (2013) Comparison of untreated adolescent idiopathic scoliosis with normal controls: a review and statistical analysis of the literature. Spine 38(9):778–785. https://doi.org/10.1097/brs.0b013e31827db418
GBD 2019 Diseases and Injuries Collaborators (2020) Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet 396(10258):1204–1222. https://doi.org/10.1016/s0140-6736(20)30925-9
Sato T, Hirano T, Ito T et al (2011) Back pain in adolescents with idiopathic scoliosis: epidemiological study for 43,630 pupils in Niigata city, Japan. Eur Spine J 20(2):274–279. https://doi.org/10.1007/s00586-010-1657-6
Clark EM, Tobias JH, Fairbank J (2016) The impact of small spinal curves in adolescents who have not presented to secondary care: a population-based cohort study. Spine 41(10):E611–E617. https://doi.org/10.1097/brs.0000000000001330
Théroux J, Le May S, Hebert JJ, Labelle H (2017) Back pain prevalence is associated with curve-type and severity in adolescents with idiopathic scoliosis: a cross-sectional study. Spine 42(15):E914–E919. https://doi.org/10.1097/brs.0000000000001986
Makino T, Kaito T, Sakai Y, Takenaka S, Yoshikawa H (2019) Health-related quality of life and postural changes of spinal alignment in female adolescents associated with back pain in adolescent idiopathic scoliosis: a prospective cross-sectional study. Spine 44(14):E833–E840. https://doi.org/10.1097/brs.0000000000002996
Wong AYL, Samartzis D, Cheung PWH, Cheung JPY (2019) How common is back pain and what biopsychosocial factors are associated with back pain in patients with adolescent idiopathic scoliosis? Clin Orthop Relat Res 477(4):676–686. https://doi.org/10.1097/corr.0000000000000569
Teles AR, St-Georges M, Abduljabbar F et al (2020) Back pain in adolescents with idiopathic scoliosis: the contribution of morphological and psychological factors. Eur Spine J 29(8):1959–1971. https://doi.org/10.1007/s00586-020-06489-2
Weinstein SL, Dolan LA, Spratt KF, Peterson KK, Spoonamore MJ, Ponseti IV (2003) Health and function of patients with untreated idiopathic scoliosis: a 50-year natural history study. JAMA 289(5):559–567. https://doi.org/10.1001/jama.289.5.559
Grauers A, Topalis C, Möller H et al (2014) Prevalence of back problems in 1069 adults with idiopathic scoliosis and 158 adults without scoliosis. Spine 39(11):886–892. https://doi.org/10.1097/brs.0000000000000312
Watanabe K, Ohashi M, Hirano T et al (2020) Health-related quality of life in nonoperated patients with adolescent idiopathic scoliosis in the middle years: a mean 25-year follow-up study. Spine 45(2):E83–E89. https://doi.org/10.1097/brs.0000000000003216
Ohashi M, Watanabe K, Hirano T et al (2018) Predicting factors at skeletal maturity for curve progression and low back pain in adult patients treated nonoperatively for adolescent idiopathic scoliosis with thoracolumbar/lumbar curves: a mean 25-year follow-up. Spine 43(23):E1403–E1411. https://doi.org/10.1097/brs.0000000000002716
Vandenbroucke JP, von Elm E, Altman DG et al (2007) Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. PLoS Med 4(10):E297. https://doi.org/10.1371/journal.pmed.0040297
World Medical Association (2013) World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 310(20):2191–2194. https://doi.org/10.1001/jama.2013.281053
Ekşi M, Orhun Ö, Yaşar AH et al (2022) At what speed does spinal degeneration gear up?: Aging paradigm in patients with low back pain. Clin Neurol Neurosurg 215:107187. https://doi.org/10.1016/j.clineuro.2022.107187
Chiarotto A, Maxwell LJ, Ostelo RW, Boers M, Tugwell P, Terwee CB (2019) Measurement properties of visual analogue scale, numeric rating scale, and pain severity subscale of the brief pain inventory in patients with low back pain: a systematic review. J Pain 20(3):245–263. https://doi.org/10.1016/j.jpain.2018.07.009
Nugent SM, Lovejoy TI, Shull S, Dobscha SK, Morasco BJ (2021) Associations of pain numeric rating scale scores collected during usual care with research administered patient-reported pain outcomes. Pain Med 22(10):2235–2241. https://doi.org/10.1093/pm/pnab110
Cheung KMC, Senkoylu A, Alanay A, Genc Y, Lau S, Luk KDK (2007) Reliability and concurrent validity of the adapted Chinese version of Scoliosis Research Society-22 (SRS-22) questionnaire. Spine 32(10):1141–1145. https://doi.org/10.1097/01.brs.0000261562.48888.e3
Levis B, Benedetti A, Thombs BD (2019) Accuracy of patient health questionnaire-9 (PHQ-9) for screening to detect major depression: individual participant data meta-analysis. BMJ 365:l1476. https://doi.org/10.1136/bmj.l1476
Herr NR, Williams JWJ, Benjamin S, McDuffie J (2014) Does this patient have generalized anxiety or panic disorder?: The rational clinical examination systematic review. JAMA 312(1):78–84. https://doi.org/10.1001/jama.2014.5950
Lee J, Lee EH, Moon SH (2019) Systematic review of the measurement properties of the depression anxiety stress scales-21 by applying updated COSMIN methodology. Qual Life Res 28(9):2325–2339. https://doi.org/10.1007/s11136-019-02177-x
Mens RH, Bisseling P, de Kleuver M, van Hooff ML (2022) Relevant impact of surgery on quality of life for adolescent idiopathic scoliosis: a registry-based two-year follow-up cohort study. Bone Joint J 104-b(2):265–273. https://doi.org/10.1302/0301-620x.104b2.bjj-2021-1179.r1
Altaf F, Gibson A, Dannawi Z, Noordeen H (2013) Adolescent idiopathic scoliosis. BMJ 346:F2508. https://doi.org/10.1136/bmj.f2508
Slattery C, Verma K (2018) Classifications in brief: the Lenke classification for adolescent idiopathic scoliosis. Clin Orthop Relat Res 476(11):2271–2276. https://doi.org/10.1097/corr.0000000000000405
Duramaz A, Yılmaz S, Ziroğlu N, Bursal Duramaz B, Kara T (2018) The effect of deformity correction on psychiatric condition of the adolescent with adolescent idiopathic scoliosis. Eur Spine J 27(9):2233–2240. https://doi.org/10.1007/s00586-018-5639-4
Anastasio AT, Farley KX, Rhee JM (2020) Depression and anxiety as emerging contributors to increased hospital length of stay after posterior spinal fusion in patients with adolescent idiopathic scoliosis. N Am Spine Soc J 2:100. https://doi.org/10.1016/j.xnsj.2020.100012
Matamalas A, Figueras C, Pizones J et al (2022) How back pain intensity relates to clinical and psychosocial factors in patients with idiopathic scoliosis. Eur Spine J 31(4):1006–1012. https://doi.org/10.1007/s00586-022-07117-x
Cherkin DC, Sherman KJ, Balderson BH et al (2016) Effect of mindfulness-based stress reduction vs cognitive behavioral therapy or usual care on back pain and functional limitations in adults with chronic low back pain: a randomized clinical trial. JAMA 315(12):1240–1249. https://doi.org/10.1001/jama.2016.2323
Ferreira GE, McLachlan AJ, Lin CC et al (2021) Efficacy and safety of antidepressants for the treatment of back pain and osteoarthritis: systematic review and meta-analysis. BMJ 372:M4825. https://doi.org/10.1136/bmj.m4825
Teles AR, Ocay DD, Bin Shebreen A et al (2019) Evidence of impaired pain modulation in adolescents with idiopathic scoliosis and chronic back pain. Spine J 19(4):677–686. https://doi.org/10.1016/j.spinee.2018.10.009
Ruscheweyh R, Verneuer B, Dany K et al (2012) Validation of the pain sensitivity questionnaire in chronic pain patients. Pain 153(6):1210–1218. https://doi.org/10.1016/j.pain.2012.02.025
Helenius L, Diarbakerli E, Grauers A et al (2019) Back pain and quality of life after surgical treatment for adolescent idiopathic scoliosis at 5-year follow-up: comparison with healthy controls and patients with untreated idiopathic scoliosis. J Bone Joint Surg 101(16):1460–1466. https://doi.org/10.2106/jbjs.18.01370
Dunn J, Henrikson NB, Morrison CC, Blasi PR, Nguyen M, Lin JS (2018) Screening for adolescent idiopathic scoliosis: evidence report and systematic review for the us preventive services task force. JAMA 319(2):173–187. https://doi.org/10.1001/jama.2017.11669
Mitsiaki I, Thirios A, Panagouli E et al (2022) Adolescent idiopathic scoliosis and mental health disorders: a narrative review of the literature. Children 9:597. https://doi.org/10.3390/children9050597
Acknowledgements
The authors would like to thank Ms Lai Suet Wong, Ms Mun Yee Cheung, Ms Lai Ching Mar, and Ms Lok Ling Lam for their kind assistance in the subject recruitment. The authors would also like to thank Mr Jazz Ma for his technical support in retrieving electronic data.
Funding
KC received grants from the Sanming Project of Medicine in Shenzhen (SZSM201612055) and the University of Hong Kong Shenzhen Hospital Fund for Shenzhen Key Medical Discipline (SZXK2020084).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has any potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix: Adapted classification system for adolescent idiopathic scoliosis
Appendix: Adapted classification system for adolescent idiopathic scoliosis
Curve pattern | Apical level | ||
|---|---|---|---|
Proximal thoracic [Apex at T3–T5] | Main thoracic [Apex at T6–T11] | Thoracolumbar/Lumbar [Apex at T12–L4] | |
Main thoracic | ✔ (major) | ||
Double thoracic | ✔ | ✔ (major) | |
Double major I | ✔ (major) | ✔ | |
Triple major | ✔ | ✔ | ✔ |
Thoracolumbar/lumbar | ✔ (major) | ||
Double major II | ✔ | ✔ (major) | |
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lau, K.K.L., Kwan, K.Y.H., Cheung, J.P.Y. et al. Impact of mental health components on the development of back pain in young adults with adolescent idiopathic scoliosis. Eur Spine J 32, 3970–3978 (2023). https://doi.org/10.1007/s00586-023-07908-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07908-w