Abstract
Purpose
This study aims to compare midline lumbar interbody fusion (MIDLIF) and minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) for treatment of patients with severe stenosis and lumbar degenerative spondylolisthesis (DS), focusing on dural tears rates, other complications, clinical and radiological outcomes.
Methods
This cohort study included patients with severe lumbar spinal stenosis (Shizas C or D) and lumbar DS who underwent MIDLIF or MIS-TLIF. Propensity score matching was done and the groups were compared regarding surgery time, length of stay, perioperative complications, clinical results and radiological outcomes, at 1 year of follow-up.
Results
The study included initially 80 patients, and 72 patients after matching, 36 in each group. Six patients had dural tears, four in the MIDLIF group and two in the MIS-TLIF group (p = 0.67). General complication rates and reoperations were not significantly different between the groups. Good or excellent clinical was achieved in 75% of the MIDLIF patients and 72% of the MIS-TLIF patients (p = 0.91). Radiological parameters showed small but statistically significant (p < 0.01) improvements after surgery, particularly in segmental lordosis and lumbar lordosis (2.0° and 1.7°), while pelvic tilt and global tilt decreased (1.6° and 2.6°). These findings were similar for both groups.
Conclusion
Our study confirms that MIDLIF is a safe and reliable minimally invasive alternative for lumbar interbody fusion in DS, even in patients with severe stenosis and previous spine surgery. It seems to offer similar results to MIS-TLIF regarding clinical results, radiological outcomes and complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lumbar degenerative spondylolisthesis (DS) develops due to age-related changes in intervertebral disks and facet joints, resulting in stenosis of the vertebral canal and anterior translation of one vertebra relative to the subjacent one. This condition can significantly affect patients, causing claudication, pain and disability. Surgery, either decompression or fusion, is indicated in most severe cases or when conservative treatment fails. Although there are no clear guidelines, fusion is usually preferred for patients with instability and severe back pain [1].
Transforaminal lumbar interbody fusion (TLIF) is commonly used as fusion technique to treat DS [2]. It allows for direct decompression of the spinal canal and nerve roots, without the need of neural retraction for discectomy and cage insertion. Minimally invasive surgery (MIS), particularly MIS-TLIF, offers several benefits, such as minimal soft tissue damage, reduced blood loss, lower infection rates and fewer complications, shorter hospitalization, reduced use of opioid medication and faster recoveries [3,4,5]. However, MIS-TLIF is a complex technique that requires considerable experience to be performed safely and successfully [6]. Use of tubular retractors can be challenging as a result of a narrow visual field and reduced workability, which can potentially result in insufficient decompression and more dural tears [7].
In recent years, a new minimally invasive approach was developed, the midline lumbar interbody fusion (MIDLIF). This procedure uses a small midline incision, microsurgical decompression, interbody fusion and segmental fixation using cortical bone trajectory (CBT) screws. The medial-to-lateral screw trajectory leads to less retraction of the paraspinal muscles [8], allowing smaller skin incisions comparing to open fusion techniques. Satisfactory outcomes similar to other fusion procedures have been observed with this technique [9, 10], even during the learning curve of the surgeon, most likely due to the straightforward adaptation from open procedures [11, 12]. MIDLIF offers theoretical benefits over MIS-TLIF, including a more direct approach through the midline for severe spinal canal stenosis and a good access for laminotomy and bilateral facetectomies, potentially leading to fewer dural tears and wider decompressions.
While comparisons have been made between open lumbar interbody fusions and those with cortical bone trajectories [13], there is a lack of literature regarding comparisons between minimally invasive techniques. The objective of this study is to compare MIDLIF and MIS-TLIF for treating patients with severe stenosis and DS, with a focus on dural tears rates, as well as other complications, clinical and radiological outcomes.
Methods
Study design
This retrospective cohort study of prospectively collected data included patients with severe lumbar spinal stenosis and DS who underwent MIDLIF or MIS-TLIF in the spine unit of the neurosurgical department of a Portuguese university hospital. The study protocol was approved by hospital’s ethics committee (No. 329/22) and the Strengthening the Reporting of Observational studies in Epidemiology (STROBE) guidelines were followed for writing.
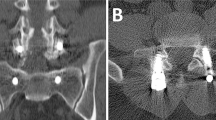
Inclusion criteria were patients with a diagnosis of symptomatic DS (slip more than 3 mm, with severe lumbar spinal stenosis (grade C or D on Schizas classification) [14], that were submitted to single-level minimally invasive lumbar interbody fusion with MIDLIF or MIS-TLIF. Exclusion criteria were previous spine fusion, deformity as main indication for surgery, more than 1 level of fusion, isthmic and other non-degenerative etiologies for the spondylolisthesis, such as trauma, infection or tumor.
The primary endpoint was the rate of dural tears, in order to study the effect of a more straightforward decompression with MIDLIF. Secondary endpoints were clinical outcome according to Odom’s criteria and lumbar lordosis improvement.
The operative procedures are standardized in our center and they have been previously described in the methods of our previous research [12, 15].
Clinical data
The following clinical parameters were collected from the medical records: age, sex, body mass index (BMI), smoker status, American Society of Anaesthesiologists’ classification of Physical Health (ASA grade), previous surgery at the same level, level of surgery, severity of the spinal stenosis according to Schizas grade, approach, surgery duration, complications, length of stay (LOS), reoperation and outcome defined by the Odom’s criteria at 1 year follow-up.
Radiological parameters
To evaluate the preoperative and postoperative sagittal alignment, the following parameters were used: pelvic incidence (PI), pelvic tilt (PT), sacral slope (SS), global tilt (GT), L1–S1 lordosis (LL), L4–S1 lordosis and the segmental lordosis of the operated segment [16, 17].
For each patient, the global alignment and proportion score (GAP) [16] was calculated at preoperative and postoperative periods, taking into account their age and the relative differences between the real and ideal values for pelvic retroversion, lumbar lordosis, lumbar lordosis distribution and global tilt. The GAP score ranges from 0 to 13 and classifies the sagittal profile as proportioned (0–2), moderately disproportioned (3–6) and severely disproportioned (≥ 7).
These parameters were measured on a lateral full-length standing spine radiograph preoperatively and at one year after surgery. They were taken independently by two researchers, for data analysis the mean of each pair of measurements was considered. Fusion status was evaluated in lumbar CT scan one year after surgery and classified as fusion, dubious or no fusion.
Statistical analysis and matching
R software (R Foundation for Statistical Computing, Vienna, Austria) version 4.2.1 was used for analysis. For agreement, intraclass correlation coefficients (ICCs) estimates were calculated based on mean rating, absolute agreement, 2-way random effects model. Variation values were obtained with subtraction of the preoperative measurements from the postoperative ones.
The matching was based on 1:1 nearest neighbor matching without replacement, with a caliper. Propensity score was used as distance and estimated with logistic regression, targeting the average treatment effect. The following covariates were used for matching: age, sex, smoker status, BMI (split at 30), previous surgery at the same level, stenosis grade, severe disproportion according to GAP score. Covariates assessment was based on standardized mean difference (SMD). SMD < 0.1 was considered an adequate balance for a variable between the groups, while values of SMD > 0.2 were considered as serious imbalance. Before matching, multiple missing imputation was performed with additive regression, bootstrapping and predictive mean matching.
After matching, continuous variables were analyzed with Wilcoxon signed-rank test for paired data and Kruskal–Wallis were used for median comparison between independent samples. Fisher’s test was used for associations between categorical variables. A p value < 0.05 was defined as statistically significant. General linear model was performed for adjustment for other variables. Decisions about the independent variables to include in the models were done by univariable selection with linear regression, based in a threshold of 0.1 for p value.
Results
The study included 80 patients diagnosed with DS and Schizas grade C (54%) or D (46%) spinal stenosis, with a median age of 66.5 years and 55 (69%) females. All patients underwent minimally invasive single-level fusion, 38 patients through MIS-TLIF and 42 MIDLIF. Table 1 presents the baseline characteristics of all patients and each group. The MIDLIF group had a higher proportion of patients with a history of previous surgery at the same level, smokers, grade D stenosis and GAP-proportioned, compared to the MIS-TLIF group.
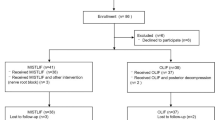
We conducted propensity score matching based on age, sex, smoker status, obesity, previous surgery, Schizas grade and GAP score severe disproportion. The resulting matched sample included 72 patients, 36 in each group, which represented 90% of the original sample. As demonstrated in Fig. 1, we obtained a good covariate balance after matching, as evidenced by SMD values below 0.1 for the selected variables.
Table 2 presents several outcome measures of all patients and each group, after matching. In the matched sample, 6 patients had dural tears, 4 in the MIDLIF group and 2 in the MIS-TLIF group, the rate of dural tears was not significantly different between the groups (Fisher’s exact test, p = 0.67). General complication rates and reoperations were not significantly different between the groups. Besides dural tears, four additional complications included one case of screw malposition and one case of postoperative radiculitis in each group. In the MIS-TLIF group, three patients were reoperated, one for screw repositioning and two due to adjacent segment disease. Also, in the MIDLIF group three patients were reoperated because of non-union, infection and adjacent segment disease. None of the patients required blood transfusion during the perioperative period.
Regarding clinical outcome, the groups did not differ significantly, as 75% of patients in the MIDLIF group and 72% in the MIS-TLIF group achieved a good or excellent outcome (Fisher’s exact test, p = 0.91). In univariate analysis, we did not find any significant association between the clinical outcome classified by Odom’s criteria and baseline characteristics, surgical data or radiological parameters. The fusion status after surgery was also similar between the groups.
Compared to the MIS-TLIF group, the duration of surgery was longer in the MIDLIF group, median of 237 min versus 150 min. The MIS-TLIF group had a longer median length of hospitalization (6 days) compared to the MIDLIF group (3.5 days). However, the patients in the MIS-TLIF group underwent surgery longer ago, they had a median follow-up of 8 years compared to 3 years for the MIDLIF group. Although the association with length of stay (LOS) was verified in univariate analysis, a multiple regression analysis found that follow-up time (intercept: 0.27, p = 0.14) and surgical group (intercept: − 0.79, p = 0.55) were not significant independent predictors of LOS. These results suggest that differences in clinical practices over the years may have influenced hospital discharge decisions and played a role in these findings.
A summary of radiological measurements before and after surgery are presented in Table 3. For those measurements, excellent reliability was achieved in inter-rater agreement analysis with ICC, ranging from 0.92 to 0.98. In the overall analysis of the sample, the radiological parameters showed statistically significant but small improvements after surgery, particularly in segmental lordosis and LL, which increased by approximately 2° (medians of 2.0 and 1.7), while PT decreased by 1.6° and GT decreased by 2.6°. The median GAP score did not change after single-level lumbar fusion. In the analysis by groups, the differences between preoperative and postoperative radiological parameters were similar for all measurements for both MIS-TLIF and MIDLIF groups (Table 4).
Discussion
Our study provides a comparison between MIS-TLIF and MIDLIF for patients with DS and severe lumbar spinal stenosis. Both techniques resulted in good to excellent symptom improvement in most patients, as well as small but statistically significant improvements in LL and segmental lordosis. For patients with severe stenosis, dural tear rates were low and similar for both groups, as well for other complications.
Previous research identified MIDLIF as a safe and reliable surgical technique for degenerative lumbar disease, with low complication rate and sustained symptom relief and disability at long-term [9, 10]. Also, MIDLIF is a suitable procedure for surgeons with limited experience in minimally invasive procedures, presumably due to its easy adaptation from open surgeries [11, 12]. In comparison with open TLIF, MIDLIF has also shown favorable results. Recent studies have consistently indicated that MIDLIF allows to achieve similar clinical and radiological outcomes with shorter surgery times, less blood loss and reduced soft tissue damage, becoming a reasonable alternative for patients with degenerative lumbar disease [18,19,20]. However, there is scarce evidence comparing MIDLIF with other minimally invasive approaches [13].
One of the theoretical advantages of MIDLIF is its reduced complication rate, given the simpler approach [11, 12]. Our study found no significant differences between the number of complications between both groups, including the number of dural tears. Similar results were reported by Maruo et al. [21] and Wu et al. [22]. In both studies, dural tear and other complications in the MIDLIF group did not significantly differ from the MIS-TLIF group, even though patients who underwent MIDLIF had more comorbidities and previous spine surgery. The MIDLIF group in the present study included more reoperated patients, which has been identified as a risk factor for accidental dural tears in minimally invasive surgeries, along with lumbar spinal stenosis [23, 24]. In contrast to other studies, we addressed this imbalance by using matching in our analysis, resulting in a balanced distribution of covariates, such as previous surgery at the same level.
No significant differences have been reported in disability and lumbar and leg pain improvement between MIDLIF and other lumbar fusion techniques. Wu et al. described better results in leg pain at 6 months postoperatively with MIS-TLIF compared to MIDLIF, but this difference disappears at 1 year of follow-up. For back pain, the article reports superior outcomes in the MIDLIF group [22]. A meta-analysis by Hu et al. that reviewed findings from 12 studies comparing MIDLIF and other posterior lumbar fusion surgeries found no difference in clinical outcomes, whether on back or leg pain [24]. We obtained similar results, with both groups presenting good to excellent symptom improvement in more than 70% of the patients.
Our study included a homogeneous diagnostic group—those with DS and severe stenosis. This comparison is important for this specific group because the choice between MIDLIF and MIS-TLIF becomes an interesting dilemma. Since the complication rate and outcomes are similar, the question remains whether there is a place for MIDLIF in this type of patients. In our opinion, this technique remains valid, firstly for surgeons who do not have experience with MIS-TLIF and see it as an optimal transition technique from open surgery to MIS. Secondly, it has the advantage of allowing a direct decompression of both foramina and a broader decompression of the central canal and lateral recesses, which can be regarded as useful in cases of bilateral foraminal stenosis or central stenosis caused by facet hypertrophy.
Lumbar spinal alignment can affect the development of lumbar pain and degenerative disease, and the long-term outcomes of lumbar fusion [25]. Elmekaty et al. found that MIDLIF patients had an increase of the lumbar lordosis and segmental disk angles after surgery in comparison with MIS-PLIF and MIS-TLIF patients [26]. Another study describes an increase in LL and decrease in PT in MIDLIF patients as well as in MIS-TLIF patients, with overall sagittal alignment not differing between groups [27]. These results are consistent with our findings that show small but significant increases in LL and segmental lordosis and decreases in PT and GT, but no difference between techniques. However, the likelihood of these changes being clinically significant is low. For interbody fusion, both techniques achieved good fusion rates, with no significant differences found.
Operation time in MIDLIF has been inconsistently reported. Some authors describe shorter operation times compared to other minimally invasive surgeries [22, 26] while others did not find differences [21, 24, 27]. Our study reveals longer operation times for MIDLIF compared to MIS-TLIF, and to the reported times in other studies. This could be due to the complexity of the surgeries contained in our study that includes patients with severe stenosis and previous spine surgeries, which are known to affect operation time.
This is a retrospective study analyzing existing records with essential exclusion criteria to reflect clinical practice. Surgery indication was similar for both groups and procedure selection were based on the standard of care at the time of intervention and surgeon preference. Propensity score matching was used to address possible bias, but observational studies are still prone to unidentifiable bias. The sample size, though larger than previous studies, is relatively small and limits the strength of conclusions.
Conclusion
MIDLIF is a safe and reliable alternative for lumbar interbody fusion in DS, even in patients with severe stenosis and previous spine surgery. Results show no significant differences between MIDLIF and MIS-TLIF, both in clinical and radiological outcomes at 1 year after surgery.
Availability of data and code
The datasets and code generated during analysis are available from the corresponding author on reasonable request.
References
Strube P, Putzier M, Siewe J et al (2019) To fuse or not to fuse: a survey among members of the German Spine Society (DWG) regarding lumbar degenerative spondylolisthesis and spinal stenosis. Arch Orthop Trauma Surg 139:613–621. https://doi.org/10.1007/s00402-018-3096-5
de Kunder SL, van Kuijk SMJ, Rijkers K et al (2017) Transforaminal lumbar interbody fusion (TLIF) versus posterior lumbar interbody fusion (PLIF) in lumbar spondylolisthesis: a systematic review and meta-analysis. Spine J 17:1712–1721. https://doi.org/10.1016/j.spinee.2017.06.018
Chan AK, Bisson EF, Bydon M et al (2020) A comparison of minimally invasive and open transforaminal lumbar interbody fusion for grade 1 degenerative lumbar spondylolisthesis: an analysis of the prospective quality outcomes database. Neurosurgery 87:555–562. https://doi.org/10.1093/neuros/nyaa097
Hockley A, Ge D, Vasquez-Montes D et al (2019) Minimally invasive versus open transforaminal lumbar interbody fusion surgery: an analysis of opioids, nonopioid analgesics, and perioperative characteristics. Glob Spine J 9:624–629 (discussion 874). https://doi.org/10.1177/2192568218822320
Khan NR, Clark AJ, Lee SL et al (2015) Surgical outcomes for minimally invasive vs open transforaminal lumbar interbody fusion: an updated systematic review and meta-analysis. Neurosurgery 77:847–874. https://doi.org/10.1227/NEU.0000000000000913
Ahn Y, Lee S, Kim W-K, Lee S-G (2022) Learning curve for minimally invasive transforaminal lumbar interbody fusion: a systematic review. Eur Spine J 31:3551–3559. https://doi.org/10.1007/s00586-022-07397-3
Wang Y, Zhang Y, Chong F et al (2020) Clinical outcomes of minimally invasive transforaminal lumbar interbody fusion via a novel tubular retractor. J Int Med Res 48:030006052092009. https://doi.org/10.1177/0300060520920090
Huang H-M, Chen C-H, Lee H-C et al (2018) Minimal invasive surgical technique in midline lumbar inter-body fusion: a technique note. J Clin Neurosci 55:103–108. https://doi.org/10.1016/j.jocn.2018.06.033
Samal F, Sterba A, Haninec P et al (2021) Long-term outcome after midline lumbar fusion for the treatment of lumbar spine instability due to degenerative disease. World Neurosurg 154:e641–e648. https://doi.org/10.1016/j.wneu.2021.07.108
Noh SH, Zhang HY (2021) Minimally invasive spine surgery with midline cortical bone trajectory screw fixation for lumbar degenerative disease in a retrospective study of 200 patients. Neurospine 18:355–362. https://doi.org/10.14245/ns.2142016.008
Dabbous B, Brown D, Tsitlakidis A, Arzoglou V (2016) Clinical outcomes during the learning curve of MIDline Lumbar Fusion (MIDLF®) using the cortical bone trajectory. Acta Neurochir 158:1413–1420. https://doi.org/10.1007/s00701-016-2810-8
Silva F, Silva PS, Vaz R, Pereira P (2019) Midline lumbar interbody fusion (MIDLIF) with cortical screws: initial experience and learning curve. Acta Neurochir 161:2415–2420. https://doi.org/10.1007/s00701-019-04079-w
Kim K-T, Song M-G, Park Y-J et al (2022) Cortical trajectory screw fixation in lumbar spine surgery: a review of the existing literature. Asian Spine J 16:127–140. https://doi.org/10.31616/asj.2020.0575
Schizas C, Theumann N, Burn A et al (2010) Qualitative grading of severity of lumbar spinal stenosis based on the morphology of the dural sac on magnetic resonance images. Spine 35:1919–1924. https://doi.org/10.1097/BRS.0b013e3181d359bd
Pereira C, Santos Silva P, Cunha M et al (2018) How does minimally invasive transforaminal lumbar interbody fusion influence lumbar radiologic parameters? World Neurosurg 116:e895–e902. https://doi.org/10.1016/j.wneu.2018.05.125
Yilgor C, Sogunmez N, Boissiere L et al (2017) Global alignment and proportion (GAP) Score: development and validation of a new method of analyzing spinopelvic alignment to predict mechanical complications after adult spinal deformity surgery. J Bone Joint Surg Am 99:1661–1672. https://doi.org/10.2106/JBJS.16.01594
Le Huec JC, Thompson W, Mohsinaly Y et al (2019) Sagittal balance of the spine. Eur Spine J 28:1889–1905. https://doi.org/10.1007/s00586-019-06083-1
Crawford CH, Owens RK, Djurasovic M et al (2019) Minimally-invasive midline posterior interbody fusion with cortical bone trajectory screws compares favorably to traditional open transforaminal interbody fusion. Heliyon 5:e02423. https://doi.org/10.1016/j.heliyon.2019.e02423
Hoffman H, Verhave B, Jalal MS et al (2019) Comparison of cortical bone trajectory screw placement using the midline lumbar fusion technique to traditional pedicle screws: a case–control study. Int J Spine Surg 13:33–38. https://doi.org/10.14444/6005
Menon N, Turcotte J, Speciale A, Patton CM (2020) Cortical bone trajectory instrumentation provides favorable perioperative outcomes compared to pedicle screws for single-level lumbar spinal stenosis and degenerative spondylolisthesis. J Orthop 22:146–150. https://doi.org/10.1016/j.jor.2020.04.001
Maruo K, Arizumi F, Kusuyama K et al (2021) Comparison of clinical outcomes after transforaminal interbody fusion using cortical bone trajectory versus percutaneous pedicle screw fixation. World Neurosurg 151:e821–e827. https://doi.org/10.1016/j.wneu.2021.04.130
Wu FL, Dang L, Zhou H et al (2020) Two-year outcomes of midline lumbar fusion versus minimally invasive transforaminal lumbar interbody fusion in the treatment of L4–L5 degenerative disease. Biomed Environ Sci BES 33:839–848. https://doi.org/10.3967/bes2020.114
Alshameeri ZAF, Jasani V (2021) Risk Factors for accidental dural tears in spinal surgery. Int J Spine Surg 15:536–548. https://doi.org/10.14444/8082
Hu J-N, Yang X-F, Li C-M et al (2019) Comparison of cortical bone trajectory versus pedicle screw techniques in lumbar fusion surgery: a meta-analysis. Medicine 98:e16751. https://doi.org/10.1097/MD.0000000000016751
Shin M-H, Ryu K-S, Hur J-W et al (2013) Comparative study of lumbopelvic sagittal alignment between patients with and without sacroiliac joint pain after lumbar interbody fusion. Spine 38:E1334–E1341. https://doi.org/10.1097/BRS.0b013e3182a0da47
Elmekaty M, Kotani Y, Mehy EE et al (2018) Clinical and radiological comparison between three different minimally invasive surgical fusion techniques for single-level lumbar isthmic and degenerative spondylolisthesis: minimally invasive surgical posterolateral fusion versus minimally invasive surgical transforaminal lumbar interbody fusion versus midline lumbar fusion. Asian Spine J 12:870–879. https://doi.org/10.31616/asj.2018.12.5.870
Wang Y-T, Li B-X, Wang S-J et al (2022) Radiological and clinical outcomes of midline lumbar fusion on sagittal lumbar-pelvic parameters for degenerative lumbar diseases. World J Clin Cases 10:12880–12889
Funding
Open access funding provided by FCT|FCCN (b-on). Not applicable.
Author information
Authors and Affiliations
Contributions
PSS and PP were involved in conceptualization and methodology; PSS, AJ, JP and RS helped in formal analysis and investigation; PSS and AJ contributed to writing—original draft preparation; PSS, PP and RV were involved in writing—review and editing; PP and RV helped in supervision.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
The study protocol was approved by the Ethics Committee of Centro Hospitalar Universitário de São João/ Faculdade de Medicina da Universidade do Porto.
Consent to participate
Informed consent was deemed unnecessary (retrospective cohort study).
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Silva, P.S., Jardim, A., Pereira, J. et al. Minimally invasive fusion surgery for patients with degenerative spondylolisthesis and severe lumbar spinal stenosis: a comparative study between MIDLIF and TLIF. Eur Spine J 32, 3210–3217 (2023). https://doi.org/10.1007/s00586-023-07847-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07847-6