Abstract
Purpose
Adjacent segment degeneration (ASDeg) after anterior cervical discectomy and fusion (ACDF) seriously affects the long-term efficacy of the operation. Therefore, our team has done a lot of research on allograft intervertebral disc transplantation (AIDT) to prove its feasibility and safety. This study will compare the efficacy between AIDT and ACDF in the treatment of cervical spondylosis.
Methods
All patients who received ACDF or AIDT in our hospital from 2000 to 2016 and followed up for at least 5 years were recruited and divided into ACDF and AIDT groups. The clinical outcomes including functional scores and radiological data of both groups were collected and compared preoperatively and postoperatively at 1 week, 3 months, 6 months, 12 months, 24 months, 60 months and last follow-up. Functional scores included Japanese Orthopedic Association score (JOA), Neck Disability Index (NDI), Visual Analog Scale of Neck (N-VAS) and Arms (A-VAS) pain, the Short Form Health Survey-36 (SF-36) and imaging dates including digital radiographs in the lateral, hyperextension and flexion positions to assess the stability, sagittal balance and mobility of the cervical spine and magnetic resonance imaging (MRI) scans to assess the degeneration of adjacent segment.
Results
There were 68 patients with 25 in AIDT group and 43 in ACDF group. Satisfactory clinical results were obtained in both groups, but the long-term NDI score and N-VAS score in the AIDT group were better. The AIDT obtained the same stability and sagittal balance of the cervical spine as fusion surgery. The range of motion of adjacent segments can be restored to the preoperative level after transplantation, but this increases significantly after ACDF. There were significant differences in the superior adjacent segment range of motion (SROM) between two groups at 12 months (P = 0.039), 24 months (P = 0.035), 60 months (P = 0.039) and the last follow-up (P = 0.011). The inferior adjacent segment range of motion (IROM) and SROM had a similar trend in the two groups. The ratio value of the greyscale (RVG) of adjacent segments showed a downward trend. At the last follow-up, the RVG decreased more significantly in the ACDF group. At the last follow-up, there was a significant difference in the incidence of ASDeg between the two groups (P = 0.000). And the incidence of adjacent segment disease (ASDis) is 22.86% in the ACDF group.
Conclusion
The allograft intervertebral disc transplantation may be as an alternative technique to traditional anterior cervical discectomy and fusion for the management of cervical degenerative diseases. For the more, the results showed it would improve cervical kinematics and reduce the incidence of adjacent segment degeneration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The incidence of intervertebral disc degenerative disease is relatively high, and it shows a trend of increasing and younger people year by year, with a high disability rate. The National Health Insurance System pays up to $50 billion annually for this disease [1]. After conservative treatment, a lot of patients are still need surgical treatment to relieve pain and numbness. However, ACDF, as the golden standard for the treatment of cervical spondylosis [2], still has many controversies [3]. The mechanism of adjacent segment degeneration after fusion is still unclear, and the debate on its mechanism mainly focuses on surgery-related biomechanical changes and age-related natural degeneration [3]. The ASDeg after fusion seriously affects the long-term efficacy of surgical treatment, and some patients even require secondary surgery to relieve symptom [4].
Therefore, intervertebral disc degenerative diseases have received increasingly attention. In the past several decades, major breakthroughs have been made in the research on the repair and regeneration of intervertebral disc degeneration, but the clinical application of these research results still needs considerable development [5, 6]. Based on the idea of organ transplantation, a lot of research works have been done in the field of intervertebral disc transplantation [7,8,9]. Ding et al. [9] found that the transplanted intervertebral disc can maintain good spinal motor function and improve the radiological and biological characteristics of the cervical spine in the research of cervical AIDT. Luk et al. [7, 10] found viable nucleus pulposus cells in animal experiments of intervertebral disc transplantation. In addition, Ruan et al. [8] found signs of hydration on T2-weighted MRI during follow-up after transplantation, which indicated that the water-absorbing properties of the nucleus pulposus were preserved. Huang et al. [11] found that the transplanted intervertebral disc was revascularized, and it was observed that there were abundant blood vessels in the endplate area at 6 months postoperatively. These showed that the AIDT had important clinical significance and scientific value in the management of intervertebral disc degenerative diseases.
Currently, the allograft intervertebral disc transplantation has been shown to relieve pain, maintain good segmental motion, and restore the imaging and biomechanical properties of the cervical spine in the management of degenerative disc disease [8, 9, 12]. However, there are no studies comparing the clinical efficacy and imaging characteristics of AIDT and ACDF. Therefore, this study will evaluate the efficacy of AIDT and ACDF in the management of cervical degenerative disease, including clinical symptom improvement, complications, imaging and biomechanical characteristics.
Materials and methods
This was a retrospective cohort study; all procedures were performed by the same surgeon team consisting of one senior spine surgeon and two assistants. The study was approved by the Institutional Review Board of the Sixth Medical Center of PLA General Hospital. Between January 2000 and December 2016, a total of 68 patients with the cervical degenerative diseases treated with ACDF and AIDT surgical techniques were included in this study according to the inclusion and exclusion criteria (Table 1).
The allograft intervertebral discs were collected from healthy young donors, who were 20–30 years old and died of trauma [8]. Bone abnormalities and any obvious disc degeneration were ruled out by cervical radiograph. Before operation, the allograft intervertebral discs were thawed by soaking in a water bath at 37 °C, and written informed consent was obtained from the donor's family and the patient. The protocol was reviewed and approved by the ethics committee of the hospital institution where the surgery was performed.
The right-side transverse or longitudinal incisions was used by Smith and Robinson approach. Complete discectomy by using pituitary rongeurs, bone scrapers, and Kerrison rongeurs, and careful preparation of the endplates with bone scrapers ensure that the endplates are not fractured. Then, the posterior longitudinal ligament was excised, the dura was fully visualized, and then the allograft intervertebral disc was placed. The location of the allograft intervertebral disc was determined by X-ray. A soft drainage tube is placed over the wound and sutured layer by layer. After the operation, the patient needs to wear a collar to limit the movement of the cervical spine for 4–6 weeks. No internal fixation was used in all 25 patients with AIDT. Among those 43 patients with ACDF, the same surgical technique above and cage/plate were used as a standard ACDF technique.
Data collection and measurement
Data collection Baseline demographic data included gender, age, and other medical conditions; Surgical data including cervical level, number of segments, whether it is internal fixation, type of cage and plate, and size of allograft intervertebral disc. The type and size of implants were excluded from the analysis because there were too many variables for a statistically significant analysis. The patients were followed up regularly at 1 week, 3 months, 6 months, 12 months, 24 months, 60 months postoperatively and last follow-up, and the data of the patient's condition and the corresponding recovery situation were recorded. Axial symptoms (AS) and neurological function were assessed at different follow-up duration, and radiology and MRI examinations were performed to complete a comprehensive evaluation.
Clinical evaluation
Clinical outcomes were determined by self-assessment questionnaires, including Neck Disability Index (NDI), Visual Analogue Score of Neck (N-VAS) and Arms (A-VAS) pain, and the Short Form Health Survey-36 (SF-36). The neurological status was assessed by Japanese Orthopaedic Association (JOA) scoring system. Intraoperative procedures and any postoperative complications were also recorded.
Imaging measurements
Patients of both groups underwent lateral, flexion, and extension digital radiographs and magnetic resonance imaging (MRI) scans of the cervical spine. Use ImageViewer or AnyPacs software installed on the workstation to acquire imaging data in DICOM or JPG format and perform measurements. All imaging data were measured three times by 3 independent reviewers and averaged. The symbol “ + ” indicates cervical kyphosis and "-" indicates cervical lordosis.
-
(1)
Disc Height Index (DHI): It is used to evaluate the change of disc height at different follow-up time points, according to the method used in previous studies [13]. The anterior height, central height, and posterior height of the intervertebral disc and the upper and lower vertebral body were measured on the lateral X-ray of the cervical spine. The ratio of twice the sum of the height of the intervertebral disc to the sum of the height of the upper and lower vertebral bodies is the DHI, that is: DHI = 2(b1 + b2 + b3)/(a1 + a2 + a3 + c1 + c2 + c3) *100%, as shown in Fig. 1A.
-
(2)
T1-Slope (T1S): Measure the angle between the upper endplate of the T1 vertebral body and the horizontal line on the lateral cervical radiograph [14], as shown in Fig. 1B.
-
(3)
C2-7 cervical lordosis (C2-7CL): the Cobb method [15] was used to measure the cervical curvature, two straight lines were drawn through the C2 inferior endplate and the C7 inferior endplate, respectively, and then the angle formed by the perpendicular lines of the first two straight lines is the curvature of the cervical spine. When the C7 vertebral body cannot be displayed on the lateral X-ray due to the occlusion of the surrounding bony tissue, according to the method of Zhang et al. [16], the measurement of C2–6CL is selected instead, as shown in Fig. 1B.
-
(4)
C2-7 Sagittal Vertical Axis (C2-7SVA): measure the horizontal distance between the vertical line through the centre of the C2 vertebral body and the posterior superior angle of the C7 vertebral body on the lateral X-ray of the cervical spine. The vertical line in front of the posterior superior angle of the C7 vertebral body is defined as a positive value, and it is defined as a negative value when it is behind [17], as shown in Fig. 1B.
-
(5)
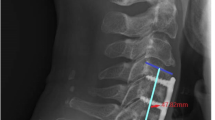
Range of motion (ROM): The Cobb method [18] is also used to measure the overall curvature of the cervical spine on the X-rays of hyperextension and flexion, and the difference between the two is the GROM (Fig. 1C, D). The Cobb angle of the intervertebral disc is the angle formed by the line connecting the lower endplate of the upper vertebral body and the upper endplate of the lower vertebral body. The difference in the Cobb angle of the transplanted disc between hyperextension and hyperflexion of the cervical spine is the range of motion of the transplanted segment (TROM) (Fig. 2B, C). The same method was used to measure the range of motion of the superior adjacent segment (SROM) and the range of motion of the inferior adjacent segment (IROM) (Fig. 1C, D).
-
(6)
The ratio value of the greyscale (RVG): To evaluate the water content of the intervertebral disc. The measurement of RVG is based on the modified Schneiderman method [19]. The MRI midsagittal T2-weighted image was imported into Photoshop software (Adobe Photoshop 2020 version) and appropriately enlarged, and a certain area of interest (ROI) was selected in the target intervertebral disc to measure the average grey value of the area. At the same time, in the cerebrospinal fluid area at the corresponding level of the intervertebral disc, a certain area of ROI side mean grey value is selected as a reference, and the ratio of the two grey values is RVG, that is: RVG = (intervertebral disc ROI average grey value/corresponding segment cerebrospinal fluid ROI average grey value) *100%. As shown in Fig. 2A.
-
(7)
Adjacent Segment Degeneration (ASDeg): To evaluate ASDeg using the method of Matsumoto M et al. [20]. On MRI, ASDeg is diagnosed if any one of the following four changes occurs: (1) decreased intervertebral disc T2 signal; (2) intervertebral disc herniation aggravates posteriorly; (3) intervertebral space is narrow; (4) intervertebral foramen stenosis. Adjacent segment degenerative disease (ASDis) is defined as obvious clinical and neurological symptoms based on the ASDeg [21], and surgical treatment is needed in severe cases.
-
(8)
The grade of allograft intervertebral disc degeneration: according to the characteristics of intervertebral disc degeneration after transplantation, combined with the modified Pfirrmann grade [22], the grade of allograft intervertebral disc degeneration was graded by T2-weighted image of MRI, as described in Table 2.
A Schematic diagram of the measurement of disc height index (DHI), DHI = [2(b1 + b2 + b3)]/[(a1 + a2 + a2) + (c1 + c2 + c3)] *100%. B Schematic diagram of the measurement of cervical lordosis (C2-7CL), sagittal vertical axis (C2-7SVA), and T1 slope (T1S). C the Cobb angle of global cervical lordosis (22.01°) and segmental angle (8.10°) in flexion. D the Cobb angle of global cervical lordosis (− 37.80°) and segmental angle (− 4.50°) in extension. The global range of motion (GROM = 22.01° − (− 37.80°) = 58.81°); the segmental range of motion (ROM = 8.10° − (− 4.50°) = 12.60°)
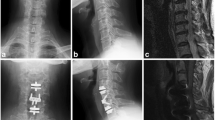
A Ratio value of the greyscale (RVG). Midsagittal T2-weighted images were chosen, and RVG was the greyscale of discs (a) normalized against the greyscale of cerebrospinal fluid at the same level (b). B and C At the last follow-up, range of motion of the transplanted segment in one patient. B, the Cobb angle of segmental angle (− 13.60°) in extension. C, the Cobb angle of segmental angle (4.41°) in flexion; the range of motion of the transplanted segment (TROM = 4.41° − (− 13.60°) = 18.01°)
Statistical analysis
The measurement data are expressed as mean ± SD, and the count data are expressed as percentage (%). Pearson's chi-square test, Fisher's exact test, Student's t test, Mann–Whitney U test, or Wilcoxon signed-rank test were used to analyse within- and between-group differences between groups in baseline data and after treatment. Repeated measures analysis of variance was used to compare the differences within- and between-groups at each time point, and when the data were not satisfied a normal distribution, nonparametric tests was used. Patients without baseline data were excluded from the respective analyses. Missing data were filled with multiple imputation methods [23]. All data were analysed using IBM SPSS Statistics 26.0. A statistically significant difference was defined as P ≤ 0.05.
Results
Demographics
According to the inclusion and exclusion criteria, there were 25 cases in AIDT group, including 18 (72%) males and 7 (28%) females, with an average age of 45.40 ± 7.30 (32–64) years old. Preoperative diagnosis included 19 cases of cervical spondylotic myelopathy, 1 case of cervical spondylotic radiculopathy, and 5 cases of cervical spondylotic myelo-radiculopathy. The involving levels were 7 cases of C4/5, 13 cases of C5/6 and 5 cases of C6/7. There were 43 cases in ACDF group, including 25 (58.14%) males and 18 (41.86%) females, with an average age of 48.12 ± 7.88 (32–62) years old. Preoperative diagnosis included 25 cases of cervical spondylotic myelopathy, 3 case of cervical radiculopathy, and 15 cases of cervical spondylotic myelo-radiculopathy. The fused segments were C3/4 in 5 cases, C4/5 in 13 cases, C5/6 in 18 cases and C6/7 in 7 cases. All of patients in both groups were followed up for at least 60 months. These data are shown in Table 3.
All patients were performed by the same surgeon team. In the AIDT group, the average operation time was 95.00 ± 12.08 min, the average intraoperative blood loss was 44.80 ± 24.00 ml, the median postoperative drainage was 20.00 ml, and the hospital time was 7.56 ± 1.71 days. In ACDF group, the average operation time was 88.37 ± 14.42 min, the average intraoperative blood loss was 46.63 ± 24.75 ml, the median postoperative drainage was 15.00 ml, and the hospital time was 6.93 ± 1.87 days. These are shown in Table 4. There was no significant difference between both two groups in all above measurement.
In the AIDT group, 1 patient had dysphagia, 1 patient had hoarseness, and 2 patients had obvious axial pain. One of the patients underwent secondary posterior foraminoplasty because axial pain and neurological dysfunction persisted to the next 2 years without significant improvement. In the ACDF group, postoperative complications included incision infection in 1 case, dysphagia in 8 cases, hoarseness in 1 case, and axial pain or neurological dysfunction in 17 cases. Only 1 case underwent secondary surgery for ASDis. The remaining postoperative complications were significantly relieved after conservative treatment. All complications are shown in Table 4.
Clinical outcome
Japanese Orthopedic Association Score (JOA): The mean JOA scores of the AIDT and ACDF groups were significantly improved from 7.92 ± 1.71 and 7.70 ± 1.83 before operation to 13.12 ± 1.54 and 12.60 ± 1.64 (P < 0.05) at 3 months post-op, 14.72 ± 1.14 and 14.21 ± 1.21 (P < 0.001) at 6 months post-op, 15.68 ± 1.18 and 15.44 ± 0.93 (P < 0.001) at 12 months post-op, 16.28 ± 1.06 and 16.02 ± 1.12 (P < 0.001) at 24 months post-op, 16.32 ± 0.85 and 15.88 ± 1.12 (P < 0.001) at 60 months post-op, 16.12 ± 0.88 and 15.51 ± 1.42 (P < 0.001) at last follow-up, respectively. The analysis found a similar trend of change between the two groups with no significant difference (Fig. 3A).
Clinical efficacy of functional scores in two groups over time. A Changes in JOA scores over time. B NDI scores over time. C and D N-VAS score and A-VAS score, respectively. E and F the PCS and MCS of SF-36, respectively. JOA, Japanese Orthopedic Association; NDI, Neck Disability Index; N-VAS, Neck Visual Analog Scale; A-VAS, Arm Visual Analog Scale; SF-36, the Short Form Health Survey-36; PCS, Physical Health Score; MCS, Mental Health Score. a-e indicate the letter labelling of the time point difference (comparison within the group), if 2 time points have the same letter, there is no significant difference between the 2 time points (P > 0.05); otherwise, different letters at 2-time points mean the difference is significant (P ≤ 0.05). Δ represents a significant difference between the two groups
Neck Disability Index (NDI): The mean NDI scores of the AIDT and ACDF groups decreased from 55.32 ± 9.15 and 56.52 ± 9.58 before operation to 50.82 ± 9.04 and 53.22 ± 9.03 (P < 0.001) at 3 months post-op, 42.63 ± 10.13 and 43.73 ± 10.47 (P < 0.001) at 6 months post-op, 31.61 ± 10.37 and 32.72 ± 11.94 (P < 0.001) at 12 months post-op, 12.33 ± 7.50 and 13.30 ± 8.69 (P < 0.001) at 24 months post-op, 11.89 ± 7.15 and 15.32 ± 8.27 (P < 0.001) at 60 months post-op, 13.95 ± 7.05 and 18.38 ± 8.66 at the last follow-up, respectively. The NDI scores in two groups recovered well in the early and middle stage after operation, but the NDI score in ACDF group was significantly higher than that in AIDT group at the last follow-up (P = 0.036), as shown in Fig. 3B.
Visual Analog Scale (VAS) of Pain: The mean N-VAS scores in the AIDT and ACDF groups decreased from 6.44 ± 0.58 and 6.63 ± 1.48 before operation to 4.36 ± 0.49 and 4.56 ± 0.55 (P < 0.05) at 3 months post-op, 3.36 ± 0.70 and 3.58 ± 0.88 (P < 0.001) at 6 months post-op, 2.36 ± 0.86 and 2.67 ± 0.68 (P < 0.001) at 12 months post-op, 1.24 ± 0.83 and 1.56 ± 1.03 (P < 0.001) at 24 months post-op, 1.16 ± 0.90 and 1.65 ± 1.13 (P < 0.001) at 60 months, 1.20 ± 0.82 and 1.86 ± 1.30 (P < 0.001) at the last follow-up, respectively. Compared with those before operation, the postoperative N-VAS scores in both groups were significantly improved. At the last follow-up, the N-VAS in ACDF group was significantly higher than that in AIDT group (P = 0.043; Fig. 3C).
The mean A-VAS scores in the AIDT and ACDF groups decreased from 4.40 ± 1.55 and 4.56 ± 1.40 before operation to 2.20 ± 1.08 and 2.37 ± 1.18 (P < 0.01) at 3 months post-op, 1.56 ± 1.16 and 1.70 ± 1.17 (P < 0.001) at 6 months post-op, 0.92 ± 0.95 and 1.07 ± 1.01 (P < 0.001) at 12 months post-op, 0.80 ± 0.65 and 0.88 ± 0.85 (P < 0.001) at 24 months post-op, 0.72 ± 0.74 and 0.98 ± 0.91 (P < 0.001) at 60 months post-op, 0.88 ± 0.78 and 1.16 ± 1.11(P < 0.001) at the last follow-up, respectively. The analysis found a similar trend of change between the two groups, with no significant difference between two groups (Fig. 3D).
The Short Form-36 The SF-36 [24] is made up of eight dimensions: physical functioning, role-physical, bodily pain, general health, vitality, social functioning, role-emotional and mental health. Therefore, total physical and mental health scores (SF-36 physical component score, SF-36 PCS, and SF-36 mental component score, SF-36 MCS) can be calculated separately [25].
The SF-36 PCS scores in the AIDT and ACDF groups improved from 32.30 ± 6.17 and 31.56 ± 9.47 before operation to 37.75 ± 6.44 and 36.19 ± 7.59 (P < 0.05) at 3 months post-op, 43.38 ± 7.28 and 41.70 ± 7.95 (P < 0.001) at 6 months post-op, 61.22 ± 6.12 and 59.78 ± 9.23 (P < 0.001) at 12 months post-op, 79.33 ± 6.80 and 77.41 ± 7.83 (P < 0.001) at 24 months post-op, 78.75 ± 7.15 and 76.68 ± 8.14 (P < 0.001) at 60 months post-op, 77.89 ± 6.86 and 74.66 ± 8.43 (P < 0.001) at the last follow-up, respectively. The analysis found that the two groups had similar trends, and there was no significant difference between two groups (P = 0.109; Fig. 3E).
The change curves of the SF-36 MCS in the two groups have a similar trend to that of the SF-36 PCS. There were also significant differences in the SF-36 MCS at postoperative any time points, compared with pre-operation, and there was no significant difference between two groups (P = 0.129; Fig. 3F).
Radiological assessment
All imaging data were measured three times by 3 independent reviewers. The analysis showed that there were no significant measurement error among the 3 independent reviewers.
Disc height index (DHI)
The mean DHI of the AIDT and ACDF groups increased from (42.85 ± 5.93)% and (42.49 ± 6.84)% before operation to (45.52 ± 4.82)% and (45.36 ± 6.74)% (P > 0.05) at 1 week post-op, respectively. The DHI remained at a stable level during the follow-up in ACDF group. The DHI in AIDT group decreased from (45.52 ± 4.82)% at 1 week post-op to (44.45 ± 5.54)% (P > 0.05) at 3 months post-op, (44.17 ± 5.67)% (P > 0.05) at 6 months post-op, (43.93 ± 5.26)% (P > 0.05) at 12 months post-op, (42.30 ± 5.74)% (P < 0.001) at 24 months post-op, (35.90 ± 4.90)% (P < 0.001) at 60 months post-op, (29.33 ± 6.67)% (P < 0.001) at the last follow-up. At 60 months post-op and the last follow-up, there was significant difference between the two groups (P < 0.001; Fig. 4A).
Results of imaging measurements. A Changes in DHI during the follow-up. B Changes in T1S during the follow-up. C Changes in C2-7CL during the follow-up. D Changes in C2-7SVA during the follow-up. E Changes in GROM during the follow-up. F and G Changes in the range of motion of the superior and inferior adjacent segments, respectively. H and I the changes of grey value of superior and inferior adjacent segments, respectively. DHI, Disc Height Index; T1S, T1-Slope; C2-7CL, C2-7 cervical lordosis; C2-7SVA, C2-7 Sagittal Vertical Axis; GROM, the global range of motion; SROM, the superior adjacent segment range of motion; IROM, the inferior adjacent segment range of motion; SRVG, the superior segment ratio value of the greyscale; IRVG, the inferior segment ratio value of the greyscale. a-d indicate the letter labelling of the time point difference (comparison within the group); if two time points have the same letter, there is no significant difference between the two time points (P > 0.05); otherwise, different letters at 2-time points mean the difference is significant (P ≤ 0.05). Δ represents a significant difference between the two groups
Sagittal balance
T1 slope (T1S): The T1S in both groups remained at a stable level during the follow-up, and there was no statistical significance within and between groups, as shown in Fig. 4B.
C2-7 cervical lordosis (C2-7CL): The mean C2-7CL in the AIDT and ACDF groups were significantly improved from (− 20.20 ± 6.57)° and (− 19.77 ± 7.44)° before operation to (− 23.38 ± 7.56)° and (− 22.85 ± 5.67)° (P > 0.05) at 1 week post-op, (− 27.09 ± 3.64)° and (− 26.31 ± 4.07)° (P < 0.001) at 3 months post-op, (− 29.06 ± 4.56)° and (− 28.27 ± 4.21)° (P < 0.001) at 6 months post-op, (− 31.48 ± 6.60)° and (− 30.08 ± 4.00)° (P < 0.001) at 12 months post-op, (− 32.01 ± 5.14)° and (− 31.25 ± 4.18)° (P < 0.001) at 24 months post-op, (− 31.84 ± 4.02)° and (− 30.79 ± 4.39)° (P < 0.001) at 60 months post-op, (− 31.25 ± 3.45)° and (− 29.81 ± 4.21)° (P < 0.001) at the last follow-up, respectively. The C2-7CL postoperatively were improved compared with that preoperatively and showed a similar trend between the two groups with no significant difference (P = 0.158; Fig. 4C).
C2-7 Sagittal Vertical Axis (C2-7SVA): The mean C2-7SVA in the AIDT and ACDF groups were significantly improved from (7.69 ± 3.32) mm and (7.91 ± 3.40) mm before operation to (12.82 ± 3.74) mm and (13.27 ± 4.09) mm (P < 0.001) at 1 week post-op, (13.59 ± 3.37) mm and (14.16 ± 4.47) mm (P < 0.001) at 3 months post-op, (14.39 ± 4.52) mm and (14.82 ± 3.31) mm (P < 0.001) at 6 months post-op, (15.46 ± 4.31) mm and (15.91 ± 3.97) mm (P < 0.001) at 12 months post-op, (16.29 ± 4.68) mm and (16.84 ± 4.69) mm (P < 0.001) at 24 months post-op, (16.18 ± 5.34) mm and (16.71 ± 4.52) mm (P < 0.001) at 60 months post-op, (16.44 ± 4.26) mm and (17.14 ± 4.69) mm (P < 0.001) at the last follow-up, respectively. The C2-7SVA postoperatively was improved compared with that preoperatively and had a similar trend in the two groups, and there was no significant difference between the groups (P = 0.549; Fig. 4D).
Range of motion (ROM)
The range of motion mainly includes the global range of motion of the cervical spine (GROM), the range of motion of the superior adjacent segment (SROM), the range of motion of the inferior adjacent segment (IROM) and the range of motion of the transplanted segment (TROM).
The mean GROM in the AIDT and ACDF groups were (44.89 ± 9.37)° and (44.27 ± 9.75)° before surgery, (42.13 ± 8.29)° and (40.09 ± 8.49)° (P = 0.576, P = 0.014) at 3 months post-op, (44.18 ± 9.34)° and (41.66 ± 8.86)° (P > 0.05) at 6 months post-op, (44.69 ± 9.66)° and (42.22 ± 8.49)° (P > 0.05) at 12 months post-op, (43.78 ± 8.92)° and (41.97 ± 8.39)° (P > 0.05) at 24 months post-op, (42.95 ± 8.97)° and (41.02 ± 7.84)° (P > 0.05) at 60 months post-op, and (41.16 ± 7.13)° and (39.54 ± 6.69)° (P = 0.319, P = 0.019) at the last follow-up, respectively. Compared with AIDT group, the GROM in ACDF group decreased slightly, but there was no statistical difference between the two groups (P = 0.303; Fig. 4E).
The SROM in the AIDT and ACDF groups were (9.08 ± 2.31)° and (9.12 ± 2.30)° before operation, (7.77 ± 1.99)° and (7.96 ± 2.01)° at 3 months post-op, (8.67 ± 2.24)° and (8.86 ± 1.89)° at 6 months post-op, (9.13 ± 2.47)° and (10.46 ± 2.16)° at 12 months post-op, (9.08 ± 2.26)° and (10.37 ± 2.13)° at 24 months post-op, (8.66 ± 1.93)° and (9.93 ± 2.36)° at 60 months post-op, and (7.94 ± 1.98)°and (9.28 ± 1.75)° at the last follow-up, respectively. The SROM in both groups returned to the preoperative level at 6 months post-op, and the SROM in ACDF group increased significantly at 12 months after operation. There were significant differences between the two groups at 12 months (P = 0.039), 24 months (P = 0.035), 60 months (P = 0.039) and the last follow-up (P = 0.011) postoperatively, as shown in Fig. 4F.
The IROM and SROM in the AIDT and ACDF groups had similar trends, and there were significant differences between the two groups at 12 months (P = 0.027), 24 months (P = 0.008), 60 months (P = 0.031), and the last follow-up (P = 0.046) after surgery postoperatively, as shown in Fig. 4G.
During the follow-up, the transplanted segment still maintained the motion function. The TROM was (9.38 ± 2.63)° before operation, (8.03 ± 1.74)° (P = 0.025) at 3 months post-op, (9.33 ± 1.72)° (P = 0.932) at 6 months post-op, (8.98 ± 2.02)° (P = 0.334) at 12 months post-op, (8.26 ± 1.86)° (P = 0.024) at 24 months post-op, (7.20 ± 2.04)° (P = 0.001) at 60 months post-op, and (5.04 ± 2.24)° (P < 0.001; Fig. 2B, C) at the last follow-up. At 60 months post-op and the last follow-up, the TROM was significantly decreased compared with that preoperatively.
During the entire follow-up period, no prolapse and loosening of implants, pseudoarthrosis, and instability of the responsible segment were found in both groups. In addition, we also found a unique phenomenon of transplanted intervertebral disc: allograft intervertebral disc remodelling.
MRI-related evaluation
The ratio value of the greyscale (RVG): The mean SRVG in AIDT and ACDF groups decreased from (44.75 ± 8.87)% and (44.35 ± 9.80)% before operation to (44.40 ± 8.35)% and (43.98 ± 8.65)% (P > 0.05) at 1 week post-op, (43.71 ± 7.50)% and (43.18 ± 9.46)% (P > 0.05) at 6 months post-op, (43.46 ± 8.12)% and (42.92 ± 9.53)% (P > 0.05) at 12 months post-op, (42.42 ± 8.54) % and (41.82 ± 8.75) % (P > 0.05) at 24 months post-op, (41.50 ± 8.11) % and (38.37 ± 7.08) % (P = 0.135, P < 0.001) at 60 months post-op, and (36.12 ± 7.56) % and (30.39 ± 7.68) % (P < 0.001) at the last follow-up, respectively. The SRVG in both groups showed a downward trend, and at the last follow-up, the decreasing trend of SRVG in the ACDF group was more significant than that in the AIDT group (P = 0.008; Fig. 4H).
The IRVG and SRVG in two groups had a similar trend. At the last follow-up, the decreasing trend of IRVG in ACDF group was more significant than that in AIDT group (P = 0.017; Fig. 4I).
Adjacent Segment Degeneration (ASDeg): At 24 months post-op, the ASDeg in AIDT and ACDF groups was 1 and 8 segments, respectively, and there was no significant difference between the two groups (P = 0.076). At 60 months post-op, the ASDeg had 2 and 29 segments in the AIDT and ACDF groups, respectively, with significant difference between the two groups (P = 0.000). At the last follow-up, the ASDeg was 7 and 37 segments in AIDT and ACDF groups, respectively, with significant differences between the two groups (P = 0.000; Fig. 5). These are shown in Table 5.
A–D Data were from an AIDT patient. A MRI before operation. B X-ray at one week after operation. C and D At the duration of last follow-up, the results of MRI and X-ray. The height of transplanted intervertebral disc (C5-6) decreased significantly. And no obvious degeneration was found in adjacent segments. E–H Data were from an ACDF patient. E MRI before operation. F X-ray at one week after operation. G and H At the duration of last follow-up, the results of MRI and X-ray. The MRI showed C3-4 herniation was more severe than that before operation
Adjacent segment disease (ASDis): No ASDis was found in AIDT group during the whole follow-up. At 24 months post-op, there were 2 cases of ASDis in ACDF group, of which 1 case received secondary operation. And the incidence of ASDis was 5.13%. At 60 months post-op, there were 5 cases of ASDis in ACDF group, and the incidence of ASDis was 12.82%. At the last follow-up, 8 cases of ASDis occurred in ACDF group, with an incidence of 22.86%.
Degeneration of the allograft intervertebral disc: According to the grading criteria of intervertebral disc degeneration, the signal intensity and height of the allograft intervertebral disc on the T2-weighted image of MRI decreased gradually in this follow-up, as shown in Table 6.
Discussion
Allograft intervertebral disc transplantation is a safe and effective method for the treatment of degenerative disc disease [8, 9]. This study is the first study to compare the clinical efficacy and imaging properties of this novel technique with conventional fusion surgery. Axial symptoms (AS) and neurological function were significantly improved in all patients, which was confirmed by JOA score, NDI, N-VAS, A-VAS and SF-36. And this suggests that AIDT has similar clinical outcomes to conventional fusion surgery. However, at the last follow-up, NDI score (P = 0.036) and N-VAS score (P = 0.043) in ACDF group were significantly higher than those in AIDT group. And some patients in ACDF group have neck pain or upper limb numbness, and even need to take painkillers or neurotrophic drugs for treatment, we believe that the main reason may be adjacent segmental disease (ASDis).
All patients achieved satisfactory clinical efficacy at early and mid-term follow-up, which mainly depended on whether the spinal cord and nerves were adequately decompressed. During surgical treatment of intervertebral disc degenerative diseases, it is one of the key factors for successful surgery to relieve the compression of the spinal cord and nerve roots by soft or bony tissues, relieve nerve tension, and facilitate the recovery of nerve function. However, the long-term clinical effect of cervical surgery is affected by adjacent segmental degeneration [3, 26, 27]. There are mainly adjacent segmental disc herniation and segmental instability leading to neck pain, limb numbness and other clinical symptoms, and some patients need a second operation to relieve the pain [4, 26, 28].
There were no serious complications in both two groups. Our study found that the incidence of dysphagia after ACDF (18.60%) was significantly higher than that of AIDT (4%). Dysphagia is the most common complication after anterior cervical surgery [29, 30]. A series of literature reports show that the incidence of ACDF is 1.7% to 67% [29]. The main reasons of dysphagia after cervical surgery are surgical injury of surrounding soft tissue, endotracheal intubation and internal fixation [30]. Our results show that internal fixation may be the leading cause of dysphagia.
Our study showed that AIDT achieved satisfactory clinical results, while also restoring and maintaining good imaging and biomechanical properties of the cervical spine. During early- and mid-term follow-up, the AIDT and ACDF both maintained a similar intervertebral height. At the duration of last follow-up, the height of the allograft intervertebral disc decreased significantly, which may lead to the local loss of cervical lordosis and malalignment of the spine. This shows that allograft intervertebral disc has a certain degree of degeneration after transplantation. However, in the ACDF group, cage subsidence was no found, and the disc height and cervical curvature were maintained at a good level. The intervertebral disc height of the transplanted segment decreases gradually with the increasing duration of follow-up, but this degeneration did not raise corresponding symptoms and did not affect the outcomes in long-term follow-up.
Although the allograft intervertebral disc had a certain degree of degeneration, it still maintained a good segmental range of motion. In addition, our study found that the allograft intervertebral disc also maintained the same range of motion at the adjacent segment as that preoperatively, which indicated that the AIDT might maximize the maintenance of normal spinal biomechanics. In theory, this could be beneficial for relieving or avoiding ASDeg after intervertebral disc transplantation [8, 9]. On the contrary, fusion technique leads to the loss of the range of motion of the responsible segment, which increases the load at the adjacent segment, changes the local biomechanics of the cervical spine, and accelerates the degeneration at the adjacent segment [31, 32]. In addition, intervertebral body fusion also leads to changes in the horizontal centre of rotation of adjacent segments and increased intradiscal pressure [31, 32], which may also accelerate the degeneration. But a study of a goat model of AIDT showed that due to the remodel-ability of the transplanted disc, the AIDT was able to restore the centre of rotation of the spine and returned to a normal spine at 6 months after transplantation [33]. Therefore, this further showed that the biomechanical properties of the cervical spine after intervertebral disc transplantation are in line with the normal physiological state of the human cervical spine to the greatest extent. It also showed that it was more advantageous to maintain the radiographic and biomechanical properties of adjacent segments after intervertebral disc transplantation.
Allograft intervertebral discs maintained reasonable spinal stability, improved C2-7 cervical lordosis and restored sagittal balance [8, 9, 12]. Whether the stability and sagittal balance of the cervical spine affect the motion of each micro-movement joint of the cervical spine, which is the key to the relief and maintenance of symptoms after surgery. Several literatures have confirmed that poor sagittal alignment after surgery is a risk factor for ASDeg [34,35,36]. Sagittal imbalance maintain effective posture by reducing the T1 slope [36, 37]. A retrospective study showed that T1 slope less than 19.50 may be an independent risk factor for ASDeg, and it is reasonable to keep T1 slope greater than 19.50 [36].
Comparing with fusion technique, the AIDT maintain the stability of the cervical spine for a long time, improve C2-7 cervical lordosis, and restore the sagittal balance. The main reason is that the endplate of the allograft intervertebral disc and the vertebral body of the recipient produce bony union [8]. This osseous healing ensures that the transplanted intervertebral disc still maintain cervical motion and biomechanics without the use of internal fixation devices [9, 38]. At the same time, this avoids the complications associated with internal fixation prolapse, heterotopic ossification, etc. In addition, no obvious immune response was found during the follow-up, which is also the main reason for maintaining spinal stability [7, 8, 10]. Therefore, the osseous healing of the transplanted intervertebral disc is the key to ensure the stability of the spine.
MRI is one of useful methods to evaluate the water content of the intervertebral disc, and it reflect the degeneration of the intervertebral disc through the change of the grey value of the intervertebral disc [19, 39]. On the midsagittal T2-weighted image of MRI, the change trend of the RVG of the adjacent intervertebral discs indicated that the RVG of the adjacent intervertebral discs after fusion decreased more obviously than that after transplantation. The main reason for the accelerated decrease of RVG in adjacent segments after ACDF may be the overactivity of segments and the increase of intervertebral disc pressure. Although there is a downward trend in RVG of adjacent segments after AIDT, the main reason may be age-related natural degeneration. In addition, we are still unable to evaluate the effect of surgical soft tissue injury on adjacent segmental degeneration. Therefore, what is clear from our findings is that segmental fusion changes the biomechanics of the cervical spine and accelerates the degeneration of adjacent segments.
In addition, the incidence of ASDeg in both groups also showed that AIDT has the advantage of protecting adjacent segment degeneration in the treatment of cervical spondylosis. At the duration of last follow-up, the incidence of ASDeg was 21.88% and no ASDis was found in AIDT group. But in the ACDF group, the incidence of ASDeg was 82.22% and the incidence of ASDis was 22.86%, of which one patient underwent secondary operation. However, the occurrence of ASDeg after fusion seriously affected the mid- and long-term efficacy of surgery, and led to the recurrence of axial symptoms or neurological dysfunction in patients, and some patients even required secondary surgery [4, 26, 28]. The literature showed that the incidence of ASDeg at 5-year follow-up after fusion was 92%, and the incidence at 10-year follow-up was 96.7% [27]. In addition, Hilibrand et al. [40, 41] reported an annual ASDeg incidence of 2.9% and predicted a 10-year incidence of 26%. At the same time, meta-analysis estimated that 1/4–1/3 of ASDeg would progress to the ASDis [26]. At present, it is generally believed that the pathogenesis of ASDeg is not clear, and the main debate is mainly focused on the biological changes after surgery and age-related natural degeneration [3].
There was degeneration in both allograft intervertebral disc and adjacent intervertebral discs after cervical spinal surgery. Intervertebral disc degeneration is often unavoidable with age, whether it is subchondral bone sclerosis, endplate calcification, decreased grey value of the intervertebral disc, and calcification of surrounding ligaments and soft tissues found on imaging [20, 42, 43], or the decrease in the number of disc cells, the less production of important matrix proteins, and the production of a large number of inflammatory factors, degrading enzymes and harmful molecules from molecular cytology [1, 44], all indicate that there is natural degeneration of the intervertebral disc. It is still a difficult problem to artificially reverse intervertebral disc degeneration. The application of stem cell transplantation, molecular therapy and gene therapy in intervertebral disc degeneration is still in the early stage of development. In addition, these studies focus more on the nucleus pulposus, often ignoring the ageing and damaged physical structure of the annulus fibrosus. Even if the nucleus pulposus cells are successfully regenerated, the degeneration of the mechanical properties of the annulus fibrosus will be so severe that the intervertebral disc cannot function normally [8]. The AIDT is influenced by the concept of organ, which is the transplantation of endplate-intervertebral disc-endplate complex. This transplantation technique not only considers the degeneration of the nucleus pulposus, but also considers the ageing and damage of the annulus fibrosus. The results of our study show that AIDT has obvious advantages in long-term clinical efficacy and degeneration of adjacent segments compared with traditional fusion. Therefore, the transplanted disc is promising as a biotype carrier for the treatment of degenerative disc disease.
However, this study is a retrospective cohort study, and the follow-up rate was 84.00% in the AIDT group and 81.39% in the ACDF group at the last follow-up. This study also has the following shortcomings: Firstly, this study may have selection bias, information bias and confounding bias. During follow-up, these biases are mainly due to incomplete data records of some patients, uneven follow-up time, a small number of patients who are lost to follow-up, and confounding factors such as age, smoking, and mental status that affect the results [1, 4]. Secondly, although all measurements were averaged over three measurements by 3 independent reviewers, there is still measurement error. Thirdly, the sample size of this study is small, and the results may be potentially biased, but this study still prove that AIDT has more advantages than traditional fusion in solving complications and ASDeg in the treatment of degenerative cervical disease.
Conclusion
The allograft intervertebral disc transplantation may be as an alternative technique to traditional anterior cervical discectomy and fusion for the management of cervical degenerative diseases. For the more, the results showed it would improve cervical kinematics and reduce the incidence of adjacent segment degeneration.
References
Kirnaz S, Capadona C, Lintz M, Kim B, Yerden R, Goldberg JL, Medary B, Sommer F, McGrath LB Jr, Bonassar LJ, Härtl R (2021) Pathomechanism and biomechanics of degenerative disc disease: features of healthy and degenerated discs. Int J Spine Surg 15(s1):10–25. https://doi.org/10.14444/8052
Brodke DS, Zdeblick TA (1992) Modified Smith–Robinson procedure for anterior cervical discectomy and fusion. Spine 17(10 Suppl):S427–S430. https://doi.org/10.1097/00007632-199210001-00014
Tobert DG, Antoci V, Patel SP, Saadat E, Bono CM (2017) Adjacent segment disease in the cervical and lumbar spine. Clin Spine Surg 30(3):94–101. https://doi.org/10.1097/BSD.0000000000000442
Wu JC, Chang HK, Huang WC, Chen YC (2019) Risk factors of second surgery for adjacent segment disease following anterior cervical discectomy and fusion: a 16-year cohort study. Int J Surg (London, England) 68:48–55. https://doi.org/10.1016/j.ijsu.2019.06.002
Huang YC, Hu Y, Li Z, Luk KDK (2018) Biomaterials for intervertebral disc regeneration: current status and looming challenges. J Tissue Eng Regen Med 12(11):2188–2202. https://doi.org/10.1002/term.2750
Bowles RD, Setton LA (2017) Biomaterials for intervertebral disc regeneration and repair. Biomaterials 129:54–67. https://doi.org/10.1016/j.biomaterials.2017.03.013
Luk KD, Ruan DK, Chow DH, Leong JC (1997) Intervertebral disc autografting in a bipedal animal model. Clin Orthop Relat Res 337:13–26. https://doi.org/10.1097/00003086-199704000-00003
Ruan D, He Q, Ding Y, Hou L, Li J, Luk KD (2007) Intervertebral disc transplantation in the treatment of degenerative spine disease: a preliminary study. Lancet (London, England) 369(9566):993–999. https://doi.org/10.1016/S0140-6736(07)60496-6
Ding Y, Ruan DK, He Q, Hou LS, Lin JN, Cui HP (2016) Imaging evaluation and relative significance in cases of cervical disk allografting: radiographic character after total disk transplantation. Clin Spine Surg 29(9):E488–E495. https://doi.org/10.1097/BSD.0b013e318290fc41
Luk KD, Ruan DK, Lu DS, Fei ZQ (2003) Fresh frozen intervertebral disc allografting in a bipedal animal model. Spine 28(9):864–870. https://doi.org/10.1097/01.BRS.0000058710.01729.29
Huang YC, Xiao J, Leung VY, Lu WW, Hu Y, Luk KDK (2018) Lumbar intervertebral disc allograft transplantation: the revascularisation pattern. Eur Spine J 27(3):728–736. https://doi.org/10.1007/s00586-017-5419-6
Luk KD, Ruan DK (2008) Intervertebral disc transplantation: a biological approach to motion preservation. Eur Spine J 17(Suppl 4):504–510. https://doi.org/10.1007/s00586-008-0748-0
Ying J, Han Z, Zeng Y, Du Y, Pei S, Su L, Ruan D, Chen C (2019) Evaluation of intervertebral disc regeneration with injection of mesenchymal stem cells encapsulated in PEGDA-microcryogel delivery system using quantitative T2 mapping: a study in canines. Am J Transl Res 11(4):2028–2041
Patwardhan AG, Khayatzadeh S, Havey RM, Voronov LI, Smith ZA, Kalmanson O, Ghanayem AJ, Sears W (2018) Cervical sagittal balance: a biomechanical perspective can help clinical practice. Eur Spine J 27(Suppl 1):25–38. https://doi.org/10.1007/s00586-017-5367-1
Harrison DE, Harrison DD, Cailliet R, Troyanovich SJ, Janik TJ, Holland B (2000) Cobb method or Harrison posterior tangent method: which to choose for lateral cervical radiographic analysis. Spine 25(16):2072–2078. https://doi.org/10.1097/00007632-200008150-00011
Zhang J, Buser Z, Abedi A, Dong X, Wang JC (2019) Can C2–6 Cobb angle replace C2-7 Cobb angle?: an analysis of cervical kinetic magnetic resonance images and X-rays. Spine 44(4):240–245. https://doi.org/10.1097/BRS.0000000000002795
Ames CP, Blondel B, Scheer JK, Schwab FJ, Le Huec JC, Massicotte EM, Patel AA, Traynelis VC, Kim HJ, Shaffrey CI, Smith JS, Lafage V (2013) Cervical radiographical alignment: comprehensive assessment techniques and potential importance in cervical myelopathy. Spine 38(22 Suppl 1):S149–S160. https://doi.org/10.1097/BRS.0b013e3182a7f449
Limanówka B, Sagan L (2020) Changes in cervical range of motion following anterior cervical discectomy with fusion—preliminary results. Neurol Neurochir Pol 54(6):568–575. https://doi.org/10.5603/PJNNS.a2020.0098
Schneiderman G, Flannigan B, Kingston S, Thomas J, Dillin WH, Watkins RG (1987) Magnetic resonance imaging in the diagnosis of disc degeneration: correlation with discography. Spine 12(3):276–281. https://doi.org/10.1097/00007632-198704000-00016
Matsumoto M, Okada E, Ichihara D, Watanabe K, Chiba K, Toyama Y, Fujiwara H, Momoshima S, Nishiwaki Y, Iwanami A, Ikegami T, Takahata T, Hashimoto T (2010) Anterior cervical decompression and fusion accelerates adjacent segment degeneration: comparison with asymptomatic volunteers in a ten-year magnetic resonance imaging follow-up study. Spine 35(1):36–43. https://doi.org/10.1097/BRS.0b013e3181b8a80d
Harrop JS, Youssef JA, Maltenfort M, Vorwald P, Jabbour P, Bono CM, Goldfarb N, Vaccaro AR, Hilibrand AS (2008) Lumbar adjacent segment degeneration and disease after arthrodesis and total disc arthroplasty. Spine 33(15):1701–1707. https://doi.org/10.1097/BRS.0b013e31817bb956
Griffith JF, Wang YX, Antonio GE, Choi KC, Yu A, Ahuja AT, Leung PC (2007) Modified Pfirrmann grading system for lumbar intervertebral disc degeneration. Spine 32(24):E708–E712. https://doi.org/10.1097/BRS.0b013e31815a59a0
Xuan A, Ruan D, Wang C et al (2022) Intradiscal injection of autologous discogenic cells in patients with discectomy: a prospective clinical study of its safety and feasibility. Stem Cells Transl Med 11(5):490–503. https://doi.org/10.1093/stcltm/szac013
Patel AA, Donegan D, Albert T (2007) The 36-item short form. J Am Acad Orthop Surg 15(2):126–134. https://doi.org/10.5435/00124635-200702000-00007
Ware JE Jr, Gandek B (1998) Overview of the SF-36 health survey and the international quality of life assessment (IQOLA) project. J Clin Epidemiol 51(11):903–912. https://doi.org/10.1016/s0895-4356(98)00081-x
Hashimoto K, Aizawa T, Kanno H, Itoi E (2019) Adjacent segment degeneration after fusion spinal surgery-a systematic review. Int Orthop 43(4):987–993. https://doi.org/10.1007/s00264-018-4241-z
Litrico S, Lonjon N, Riouallon G, Cogniet A, Launay O, Beaurain J, Blamoutier A, Pascal-Mousselard H, French Society of Spine Surgery (SFCR) (2014) Adjacent segment disease after anterior cervical interbody fusion: a multicenter retrospective study of 288 patients with long-term follow-up. Orthop Traumatol Surg Res OTSR 100(6 Suppl):S305–S309. https://doi.org/10.1016/j.otsr.2014.07.004
Burch MB, Wiegers NW, Patil S, Nourbakhsh A (2020) Incidence and risk factors of reoperation in patients with adjacent segment disease: a meta-analysis. J Craniovertebr Junction Spine 11(1):9–16. https://doi.org/10.4103/jcvjs.JCVJS_10_20
Epstein NE (2019) A review of complication rates for anterior cervical diskectomy and fusion (ACDF). Surg Neurol Int 10:100. https://doi.org/10.25259/SNI-191-2019
Vaishnav AS, Saville P, McAnany S, Patel D, Haws B, Khechen B, Singh K, Gang CH, Qureshi SA (2019) Predictive factors of postoperative dysphagia in single-level anterior cervical discectomy and fusion. Spine 44(7):E400–E407. https://doi.org/10.1097/BRS.0000000000002865
Cunningham BW, Hu N, Zorn CM, McAfee PC (2010) Biomechanical comparison of single- and two-level cervical arthroplasty versus arthrodesis: effect on adjacent-level spinal kinematics. Spine J 10(4):341–349. https://doi.org/10.1016/j.spinee.2010.01.006
Eck JC, Humphreys SC, Lim TH, Jeong ST, Kim JG, Hodges SD, An HS (2002) Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine 27(22):2431–2434. https://doi.org/10.1097/00007632-200211150-00003
Lam SK, Xiao J, Ruan D, Ding Y, Lu WW, Luk KD (2012) The effect of remodeling on the kinematics of the malpositioned disc allograft transplantation. Spine 37(6):E357–E366. https://doi.org/10.1097/BRS.0b013e318232909d
Alhashash M, Shousha M, Boehm H (2018) Adjacent segment disease after cervical spine fusion: evaluation of a 70 patient long-term follow-up. Spine 43(9):605–609. https://doi.org/10.1097/BRS.0000000000002377
Wang F, Hou HT, Wang P, Zhang JT, Shen Y (2017) Symptomatic adjacent segment disease after single-lever anterior cervical discectomy and fusion: incidence and risk factors. Medicine 96(47):e8663. https://doi.org/10.1097/MD.0000000000008663
Song J, Zhang YX, Song KH, Wang HL, Zou F, Jiang JY (2018) Risk factors of adjacent segment disease after anterior cervical arthrodesis: a retrospective study of sagittal measurement of thoracic inlet parameters. World Neurosurg 114:e1094–e1100. https://doi.org/10.1016/j.wneu.2018.03.152
Park JH, Cho CB, Song JH, Kim SW, Ha Y, Oh JK (2013) T1 slope and cervical sagittal alignment on cervical CT radiographs of asymptomatic persons. J Korean Neurosurg Soc 53(6):356–359. https://doi.org/10.3340/jkns.2013.53.6.356
Xiao J, Huang YC, Lam SK, Luk KD (2015) Surgical technique for lumbar intervertebral disc transplantation in a goat model. Eur Spine J 24(9):1951–1958. https://doi.org/10.1007/s00586-014-3631-1
Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N (2001) Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine 26(17):1873–1878. https://doi.org/10.1097/00007632-200109010-00011
Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH (1999) Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am Vol 81(4):519–528
Hilibrand AS, Robbins M (2004) Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine J 4(6 Suppl):190S-194S. https://doi.org/10.1016/j.spinee.2004.07.007
Buser Z, Chung AS, Abedi A, Wang JC (2019) The future of disc surgery and regeneration. Int Orthop 43(4):995–1002. https://doi.org/10.1007/s00264-018-4254-7
Lee SH, Son DW, Lee JS, Sung SK, Lee SW, Song GS (2020) Relationship between endplate defects, modic change, facet joint degeneration, and disc degeneration of cervical spine. Neurospine 17(2):443–452. https://doi.org/10.14245/ns.2040076.038
Feng C, Liu H, Yang M, Zhang Y, Huang B, Zhou Y (2016) Disc cell senescence in intervertebral disc degeneration: Causes and molecular pathways. Cell cycle (Georgetown, Tex.) 15(13):1674–1684. https://doi.org/10.1080/15384101.2016.1152433
Funding
No funds, grants or other support was received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no potential conflict of interest in the research, authorship and publication of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhang, J., Ruan, D., Xuan, A. et al. Comparative study of outcomes between allograft intervertebral disc transplantation and anterior cervical discectomy and fusion: a retrospective cohort study at least 5 years of follow-up. Eur Spine J 32, 3561–3574 (2023). https://doi.org/10.1007/s00586-023-07799-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07799-x